
Where can I find more information on eligible hospital attestation?
For more information on eligible hospital attestation, visit our Eligible Hospital Information page. If you are new to the QualityNet system, you must enroll. For further instruction on how to enroll, use this QualityNet Secure Portal Enrollment and Login User Guide (PDF).
When is an attestation statement acceptable?
Attestation Statements. An attestation after the date of service is acceptable in most cases. Exception: when the relevant regulation, [national coverage determination (NCD), local coverage determination (LCD), and Centers for Medicare & Medicaid Services (CMS) manuals] has specific signature requirements, (e.g.,...
How do I comply with the CMS policy regarding signature requirements?
To ensure compliance with the Centers for Medicare & Medicaid Services (CMS) policy regarding signature requirements follow the instructions outlined in the CMS Pub.100-08, Program Integrity Manual, Chapter 3, Section 3.3.2.4. Medicare services provided/ordered must be authenticated by the author by some form of signature.
How do I authenticate a signature for a Medicare order?
Medicare services provided/ordered must be authenticated by the author by some form of signature. This includes orders and medical record documentation of all services provided. The signature must include the credentials of the individual and be dated.
What is a Medicare attestation?
In general, attestation is the process of validating that something is true. A healthcare organization must demonstrate meaningful use in order to be eligible for payments from the federal government under either the Medicare or Medicaid EHR incentive program.
What does health attestation mean?
When you apply for health coverage through the Marketplace, you're required to agree (or "attest") to the truth of the information provided by signing the application.
Is meaningful use still in effect 2022?
For calendar year (CY) 2022, in order to be considered a meaningful user and avoid a downward payment adjustment, eligible hospitals and CAHs may use (1) existing 2015 Edition certification criteria, (2) the 2015 Edition Cures Update criteria, or (3) a combination of the two in order to meet the CEHRT definition, as ...
When did meaningful use end?
2018 is the last year of the meaningful use penalty. Starting in 2019, meaningful use becomes PI, a part of the Medicare MIPS.
How long is an attestation valid?
It is valid for five years. On joining an airline, the holder of an attestation must then complete training to cover any airline specific procedures and also conversion to the specifics of their allocated aircraft type(s).
What is the purpose of attestation?
Attestation is the act of witnessing the signing of a formal document and then also signing it to verify that it was properly signed by those bound by its contents. Attestation is a legal acknowledgment of the authenticity of a document and a verification that proper processes were followed.
Is meaningful use still in effect 2021?
This question comes up a lot. We've got a simple answer: No, it's not – but the name is. The EHR Incentive Program, commonly known as Meaningful Use (MU), has been considered over or has “died” many times, but it is still around.
What replaced meaningful use?
Meaningful use will now be called "Promoting Interoperability" as CMS focuses on increasing health information exchange and patient data access.
What is the Cures Act 2022?
To drive the theme of “Access and Choice”, the Act was written to: Provide seamless and secure access of Electronic Health Information. Increase innovation and competition by fostering an ecosystem of new applications. Encourage adoption of standardized Application Programming Interfaces (API)
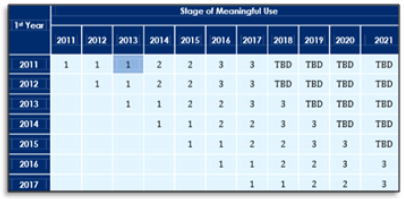
What year did meaningful use start?
2011Meaningful Use: Overview The program, which began in 2011, evolved over the course of 3 stages: Stage 1 established the base requirements for electronic capturing of clinical data. Stage 2 encouraged the use of EHRs for increased exchange of information and continuous quality improvement at the point of care.
When did Medicare require EHR?
2011In 2011, CMS established the Medicare and Medicaid EHR Incentive Programs (now known as the Medicare Promoting Interoperability Program) to encourage EPs, eligible hospitals, and CAHs to adopt, implement, upgrade, and demonstrate meaningful use of certified electronic health record technology (CEHRT).
When did meaningful use in healthcare start?
2009In 2009 the U.S. government introduced the Meaningful Use program as part of the 2009 Health Information Technology for Economic and Clinical Health (HITECH) Act.
How to contact Medicare EP?
Medicare EPs may contact the Quality Payment Program help desk for assistance at [email protected] or 1 (866) 288-8292. Back to TOP.
What is CMS in EP?
CMS allows an EP to designate a third party to register and attest on his or her behalf. To do so, users working on behalf of an EP must have an Identity and Access Management System (I&A) web user account (User ID/Password), and be associated with the EPs National Provider Identifier (NPI).
What is interoperability guide for medicaid?
The official Medicaid Program Interoperability user guides for Medicaid eligible hospital and EPs provide easy instructions for using CMS’s systems. They provide helpful tips and screenshots to walk the user through the registration process. Also, they provide important information needed to successfully register and attest.
What is Medicare authenticated?
Medicare services provided/ordered must be authenticated by the author by some form of signature. This includes orders and medical record documentation of all services provided. The signature must include the credentials of the individual and be dated.
Who must sign an attestation statement?
The attestation statement must be signed and dated by the author of the medical record entry and must contain sufficient information to identify the beneficiary. Attestation statements will not be accepted where there is no associated medical record entry.
What does it mean when a provider affixes a rubber stamp?
By affixing the rubber stamp, the provider is certifying that they have reviewed the document. If the signature is illegible, evidence in a signature log or attestation statement or other documentation will be considered. If the signature is missing from an order, the order shall be disregarded during the review of the claim.
When did CMS permit rubber stamps?
CMS permits use of a rubber stamp for signature in accordance with the Rehabilitation Act of 1973 in the case of an author with a physical disability that can provide proof to a CMS contractor of his/her inability to sign their signature due to their disability.
Does CMS require scribes to sign?
Note: When a scribe is used by a provider in documenting medical record entries (e.g. progress notes), CMS does not require the scribe to sign/date the documentation. Items or services will not be denied because a scribe has not signed/dated a note.
