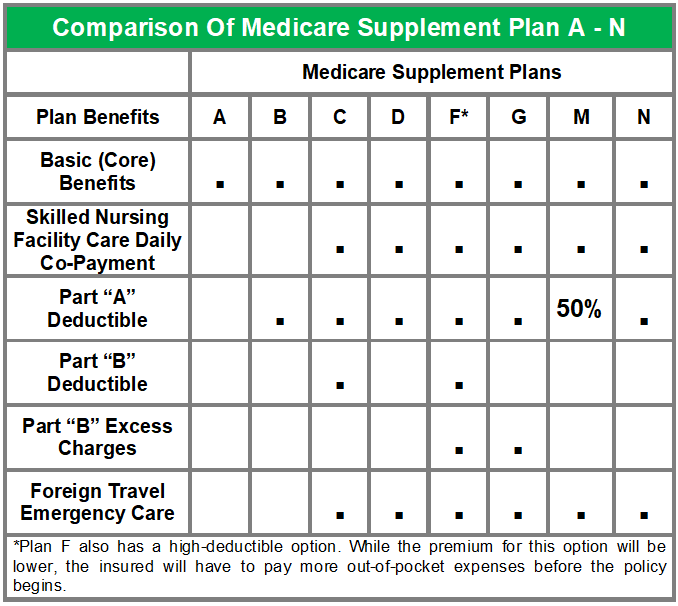
All Medicare supplement policies must provide certain core benefits, including coverage for Medicare Part A-eligible hospital expenses not covered by Medicare from the 61st day through the 90th day in any Medicare benefit period, the coinsurance amount of Medicare Part B-eligible expenses, and coverage under Medicare Parts A and B for the first 3 pints of blood.
Full Answer
What are the top 5 Medicare supplement plans?
A Medicare Supplement policy is required to do which of the following? a. Provide a 10 day free-look period b. Provide a 20 day free-look period c. Provide a 30 day free-look period d. Provide a 60 day free-look period
What is the best Medicare supplement insurance?
Dec 16, 2021 · Choosing Medicare Supplement insurance can help. It can cover up to 100% of out-of-pocket costs, depending on the plan. One out of every three Original Medicare beneficiaries — over 13 million seniors — have chosen to do so. 1. Centers for Medicare and Medicaid Services.
Should I Choose Medicare Advantage or Medigap?
Medigap is Medicare Supplement Insurance that helps fill "gaps" in . Original Medicare and is sold by private companies. Original Medicare pays for much, but not all, of the cost for covered health care services and supplies. A Medicare Supplement Insurance (Medigap) policy can help pay some of the remaining health care costs, like: Copayments
Why are Medicare Advantage plans bad?
Medigap (Medicare Supplement Health Insurance) A Medigap policy is health insurance sold by private insurance companies to fill the “gaps” in Original Medicare Plan coverage. Medigap policies help pay some of the health care costs that the Original Medicare Plan doesn't cover. If you are in the Original Medicare Plan and have a Medigap policy, then Medicare and your …
Which of the following must be included in a Medicare Supplement policy?
Medicare Supplement insurance Plan A covers 100% of four things: Medicare Part A coinsurance payments for inpatient hospital care up to an additional 365 days after Medicare benefits are used up. Medicare Part B copayment or coinsurance expenses. The first 3 pints of blood used in a medical procedure.
What is the purpose of Medicare supplemental insurance quizlet?
Terms in this set (21) private Medicare supplement insurance plans to help cover the out-of-pocket costs that remained for Medicare recipients. Commonly referred to as Medigap Plans, these private supplement plans were designed to help cover the costs associated with the 'gaps' in the Original Medicare coverage.
What does a Medicare Supplement policy cover quizlet?
Medicare supplement, or Medigap, policies supplement Medicare's benefits by paying most deductibles and co-payments as well as some health care services that Medicare does not cover. They do not cover the cost of extended nursing home care. Victoria currently as a Medicare Advantage plan.
Which of the following is true about Medicare Supplement insurance plans?
Which of the following is true about Medicare Supplement Insurance Plans? They are regulated by the Centers for Medicare & Medicaid Services (CMS). Plan benefit amounts automatically update when Medicare changes cost sharing amounts, such as deductibles, coinsurance and copayments.
What is Medicare supplement policies?
In Original Medicare, you generally pay some of the costs for approved services. Medicare Supplement Insurance (Medigap) is extra insurance you can buy from a private company that helps pay your share of costs.
What is a Medicare supplement quizlet?
Medicare Supplement Policy AKA Medigap. Also known as a Medigap Policy, is a health insurance policy sold by private insurance companies to fill in the coverage gaps in Original Medicare. The coverage gaps include deductibles and coinsurance requirements.
What is typically covered by supplemental plans quizlet?
What is typically covered by supplemental plans: copayments, coinsurance and deductibles.
Which of the following expenses are Medicare supplement policies not designed to cover?
Medicare Supplement Plan B covers basic benefits plus Medicare Part A deductible for hospitalization. Neither Medicare Supplement Plan A nor Plan B covers skilled nursing facility care or at-home recovery care.
Which renewal provision must all Medicare supplement policies contain quizlet?
A continuation provision must include any reservation by the issuer of the right to change premiums and any automatic renewal premium increases based on the policy holders age. Provisions must be captioned and appear on the first page of the policy. What is excluded under Medigap?
Who regulates Medicare Supplement plans?
Medicare Supplement plans are standardized and offer various benefits to help offset your healthcare cost. The California Department of Insurance (CDI) regulates Medicare Supplement policies underwritten by licensed insurance companies.
Which is true about Medicare Supplement open enrollment quizlet?
Which is true about Medicare Supplement Open Enrollment? By federal law, Medicare Supplement Open Enrollment is the first 6 months a consumer is 65 or older and enrolled in Medicare Part B.
What is supplemental health insurance?
Listen to pronunciation. (SUH-pleh-MEN-tul helth in-SHOOR-ents) An additional insurance plan that helps pay for healthcare costs that are not covered by a person's regular health insurance plan. These costs include copayments, coinsurance, and deductibles.
What is a Medigap policy?
Those plans are ways to get Medicare benefits, while a Medigap policy only supplements your Original Medicare benefits. The periodic payment to Medicare, an insurance company, or a health care plan for health or prescription drug coverage.
What happens if you buy a Medigap policy?
If you have Original Medicare and you buy a Medigap policy, here's what happens: Medicare will pay its share of the. Medicare-Approved Amount. In Original Medicare, this is the amount a doctor or supplier that accepts assignment can be paid. It may be less than the actual amount a doctor or supplier charges.
What is Medicare Advantage?
Medicaid. A joint federal and state program that helps with medical costs for some people with limited income and resources.
How many people does a Medigap policy cover?
for your Medigap policy. You pay this monthly premium in addition to the monthly Part B premium that you pay to Medicare. A Medigap policy only covers one person. If you and your spouse both want Medigap coverage, you'll each have to buy separate policies.
What is the difference between Medicare and Original Medicare?
Original Medicare. Original Medicare is a fee-for-service health plan that has two parts: Part A (Hospital Insurance) and Part B (Medical Insurance). After you pay a deductible, Medicare pays its share of the Medicare-approved amount, and you pay your share (coinsurance and deductibles). and is sold by private companies.
Can you cancel a Medigap policy?
This means the insurance company can't cancel your Medigap policy as long as you pay the premium. Some Medigap policies sold in the past cover prescription drugs. But, Medigap policies sold after January 1, 2006 aren't allowed to include prescription drug coverage.
Does Medicare cover all of the costs of health care?
Original Medicare pays for much, but not all, of the cost for covered health care services and supplies. A Medicare Supplement Insurance (Medigap) policy can help pay some of the remaining health care costs, like: Note: Medigap plans sold to people who are newly eligible for Medicare aren’t allowed to cover the Part B deductible.
What is a medicaid supplement?
Medigap (Medicare Supplement Health Insurance) A Medigap policy is health insurance sold by private insurance companies to fill the “gaps” in Original Medicare Plan coverage. Medigap policies help pay some of the health care costs that the Original Medicare Plan doesn't cover.
What is the difference between Medigap and Medicare?
Generally, the only difference between Medigap policies sold by different insurance companies is the cost. You and your spouse must buy separate Medigap policies.Your Medigap policy won't cover any health care costs for your spouse. Some Medigap policies also cover other extra benefits that aren't covered by Medicare.
Do you have to pay for Medigap?
Generally, when you buy a Medigap policy you must have Medicare Part A and Part B. You will have to pay the monthly Medicare Part B premium. In addition, you will have to pay a premium to the Medigap insurance company. As long as you pay your premium, your Medigap policy is guaranteed renewable.
Can insurance companies sell standardized Medicare?
Insurance companies can only sell you a “standardized” Medigap policy. Medigap policies must follow Federal and state laws. These laws protect you. The front of a Medigap policy must clearly identify it as “Medicare Supplement Insurance.”. It's important to compare Medigap policies, because costs can vary. The standardized Medigap policies that ...
What is Medicare Supplement Insurance?
Medicare supplement insurance fills the gaps in coverage left by Medicare, which provides hospital and medical expense benefits for persons aged 65 and older. All Medicare supplement policies must cover 100% of the Part A hospital coinsurance amount for each day used from.
Which Medicare supplement plan has the least coverage?
Explanation. In the 12 standardized Medicare supplement plans, Plan A provides the least coverage and is referred to as the core plan. Plan J has the most comprehensive coverage. Plans K and L provide basic benefits similar to plans A through J, but cost sharing is at different levels.
What happens after Tom pays the deductible?
After Tom pays the deductible, Medicare Part A will pay 100% of all covered charges. Explanation. Medicare Part A pays 100% of covered services for the first 60 days of hospitalization after the deductible is paid.
How long does Medicare cover skilled nursing?
Medicare will cover treatment in a skilled nursing facility in full for the first 20 days. From the 21st to the 100th day, the patient must pay a daily co-payment. There are no Medicare benefits provided for treatment in a skilled nursing facility beyond 100 days. Medicare Part A covers.
What is Medicare Part A?
Tap card to see definition 👆. Coverage of Medicare Part A-eligible hospital expenses to the extent not covered by Medicare from the 61st through the 90th day in any Medicare benefit period. Explanation. The benefits in Plan A, which is known as the core plan, must be contained in all other plans sold.
What is Medicaid in the US?
Medicaid is a federal and state program designed to help provide needy persons, regardless of age, with medical coverage. A contract designed primarily to supplement reimbursement under Medicare for hospital, medical or surgical expenses is known as. A) an alternative benefits plan. B) a home health care plan.
What is the core plan of Medicare?
Among the core benefits is coverage of Medicare Part A-eligible expenses for hospitalization, to the extent not covered by Medicare, from the 61st day through the 90th day in any Medicare benefit period.