ExxonMobil Aetna Medicare website: ExxonMobil.AetnaMedicare.com Introduction The Medicare Primary Option (MPO), is an option under the ExxonMobil Retiree Medical Plan for retirees, their eligible spouses and eligible surviving spouses who are also eligible for Medicare.
What Medicare Advantage plans does Aetna offer?
Sep 26, 2010 · If you have an Aetna Medicare Advantage HMO Plan, then the Aetna plan will always be primary as Medicare has assigned the benefits …
What does it mean when Aetna is secondary Medicare?
Sep 13, 2021 · When you’re dual eligible for both Medicare and Medicaid, Medicare is your primary payer. Medicaid will not pay until Medicare pays first. Medicaid will not pay until Medicare pays first. If you’re dual-eligible and need assistance covering the costs of Part B and Part D, you could qualify for a Medicare Savings Program to assist you with these costs.
Is Aetna Medicare PPO or HMO?
Commercial insurance claims in which another payer is primary and Aetna is secondary; Medicare primary claims for which Medicare* has not already forwarded their claims and payment information to us; When Aetna is secondary, you will need to include the appropriate code on your claim that tells us information about the primary payer’s payment.
Does Aetna Medicare cover dental?
When you have Medicare and another type of insurance, Medicare is either your primary or secondary insurer. Use the table below to learn how Medicare coordinates with other insurances. 1 Liability insurance only pays on liability-related medical claims. 2 VA benefits and Medicare do not work together. Medicare does not pay for any care provided ...

Is Medicare primary or Aetna?
Medicare pays first and your group health plan (retiree) coverage pays second . If the employer has 100 or more employees, then the large group health plan pays first, and Medicare pays second .
How do you determine which insurance is primary?
Primary insurance is a health insurance plan that covers a person as an employee, subscriber, or member. Primary insurance is billed first when you receive health care. For example, health insurance you receive through your employer is typically your primary insurance.Oct 8, 2019
Is Medicare automatically primary or secondary?
Medicare is always primary if it's your only form of coverage. When you introduce another form of coverage into the picture, there's predetermined coordination of benefits. The coordination of benefits will determine what form of coverage is primary and what form of coverage is secondary.
Is Medicare always the primary payer?
If you don't have any other insurance, Medicare will always be your primary insurance. In most cases, when you have multiple forms of insurance, Medicare will still be your primary insurance.
When two insurance which one is primary?
If you have two plans, your primary insurance is your main insurance. Except for company retirees on Medicare, the health insurance you receive through your employer is typically considered your primary health insurance plan.
What insurance is primary or secondary?
Primary insurance: the insurance that pays first is your “primary” insurance, and this plan will pay up to coverage limits. You may owe cost sharing. Secondary insurance: once your primary insurance has paid its share, the remaining bill goes to your “secondary” insurance, if you have more than one health plan.Jan 21, 2022
Is Aetna Medicare the same as Medicare?
Both terms refer to the same thing. Instead of Original Medicare from the federal government, you can choose a Medicare Advantage plan (Part C) offered by a private insurance company.Oct 1, 2021
Does Medicare become primary at 65?
Medicare is primary when your employer has less than 20 employees. Medicare will pay first and then your group insurance will pay second. If this is your situation, it's important to enroll in both parts of Original Medicare when you are first eligible for coverage at age 65.Mar 1, 2020
When Medicare is secondary payer?
Situations when Medicare is a secondary payer include when: You are covered by a group health plan (GHP) through employment, self-employed, or a spouse's employment, AND the employer has more than 20 employees.Jan 6, 2022
Is TRICARE primary or secondary to commercial insurance?
Ending Other Health Insurance Coverage If you lose your other health insurance, TRICARE becomes your primary payer. If you have TRICARE for Life, TRICARE becomes the second payer.Mar 17, 2021
What type of insurance is Medicare?
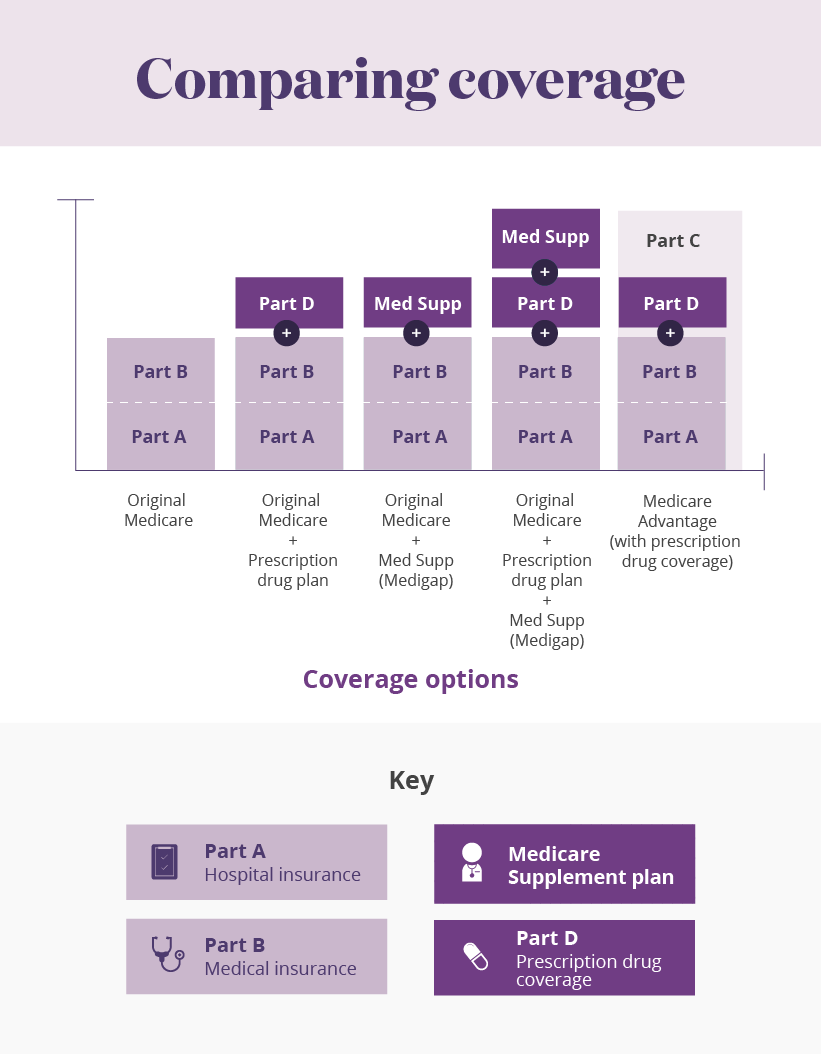
Original Medicare is a fee-for-service health plan that has two parts: Part A (Hospital Insurance) and Part B (Medical Insurance). After you pay a deductible, Medicare pays its share of the Medicare-approved amount, and you pay your share (coinsurance and deductibles).
Does Medicare automatically forward claims to secondary insurance?
Medicare will send the secondary claims automatically if the secondary insurance information is on the claim. As of now, we have to submit to primary and once the payments are received than we submit the secondary.Aug 19, 2013
What to do when Aetna is secondary?
When Aetna is secondary, you will need to include the appropriate code on your claim that tells us information about the primary payer’s payment. Contact the practice management support team and/or the clearinghouse you use to submit your electronic claims.
What is COB in healthcare?
Quick payment with coordination of benefits . Coordination of benefits (COB) occurs when a patient is covered under more than one insurance plan. This process lets your patients get the benefits they are entitled to. It helps determine which company is primarily responsible for payment.
Is Aetna responsible for the content of linked sites?
Aetna Inc. and its subsidiary companies are not responsible or liable for the content, accuracy, or privacy practices of linked sites, or for products or services described on these sites. Continue. You are now being directed to the US Department of Health and Human Services site.
Is Aetna a part of CVS?
and its subsidiary companies are not responsible or liable for the content, accuracy or privacy practices of linked sites, or for products or services described on these sites. Aetna is proud to be part of the CV S Health family . You are now being directed to the CVS Health site.
What is the difference between Medicare and Medicaid?
Eligible for Medicare. Medicare. Medicaid ( payer of last resort) 1 Liability insurance only pays on liability-related medical claims. 2 VA benefits and Medicare do not work together. Medicare does not pay for any care provided at a VA facility, and VA benefits typically do not work outside VA facilities.
Is Medicare a secondary insurance?
When you have Medicare and another type of insurance, Medicare is either your primary or secondary insurer. Use the table below to learn how Medicare coordinates with other insurances. Go Back. Type of Insurance. Conditions.
What is a D-SNP?
Our dual-eligible Special Needs Plan (D-SNP) is a type of Medicare Advantage plan, available to people who have both Medicare and Medicaid. We can help you find out if you qualify.
Does Aetna offer Medicare Advantage?
Medicare Advantage plans for every need. In addition to PPO plans, Aetna offers you other Medicare Advantage plan options — many with a $0 monthly plan premium. We can help you find a plan that’s right for you.
Does Aetna require a PCP?
Aetna Medicare Advantage plans at a glance. Our PPO plans. Requires you to use a provider network. No. But seeing out-of-network providers generally costs more. Requires you to have a primary care physician (PCP) Usually no PCP required.
Do you need a referral for a PPO?
Preferred provider organization (PPO) plans let you choose any provider who accepts Medicare. You don’t need a referral from a primary care physician for specialist or hospital visits. However, using providers in your plan’s network may cost less.
How does Medicare work with other insurance?
When there's more than one payer, "coordination of benefits" rules decide which one pays first. The "primary payer" pays what it owes on your bills first, and then sends the rest to the "secondary payer" (supplemental payer) ...
What is the difference between primary and secondary insurance?
The insurance that pays first (primary payer) pays up to the limits of its coverage. The one that pays second (secondary payer) only pays if there are costs the primary insurer didn't cover. The secondary payer (which may be Medicare) may not pay all the uncovered costs.
When does Medicare pay for COBRA?
When you’re eligible for or entitled to Medicare due to End-Stage Renal Disease (ESRD), during a coordination period of up to 30 months, COBRA pays first. Medicare pays second, to the extent COBRA coverage overlaps the first 30 months of Medicare eligibility or entitlement based on ESRD.
What is a group health plan?
If the. group health plan. In general, a health plan offered by an employer or employee organization that provides health coverage to employees and their families.
How long does it take for Medicare to pay a claim?
If the insurance company doesn't pay the claim promptly (usually within 120 days), your doctor or other provider may bill Medicare. Medicare may make a conditional payment to pay the bill, and then later recover any payments the primary payer should have made. If Medicare makes a. conditional payment.
What happens if a group health plan doesn't pay?
If the group health plan didn’t pay all of your bill, the doctor or health care provider should send the bill to Medicare for secondary payment. Medicare may pay based on what the group health plan paid, what the group health plan allowed, and what the doctor or health care provider charged on the claim.
What is a copayment?
A copayment is usually a set amount, rather than a percentage. For example, you might pay $10 or $20 for a doctor's visit or prescription drug. or a. deductible. The amount you must pay for health care or prescriptions before Original Medicare, your prescription drug plan, or your other insurance begins to pay.
What is an IPA plan?
Independent practice associations (IPAs): Plan members can request that their PCP or specialist is part of an IPA group. These groups are made up of providers, specialists, health care systems and programs. The IPA will manage all your care.
What is a PCP?
Choosing a primary care physician (PCP) Choosing the right PCP is one of the most important parts of your health care. We’re here to support and inform you so that you can make the best choice for you and your family. You can select your PCP after you enroll with Aetna Better Health ®.
Where can I see a PCP?
There are many places where you can see a PCP. Some providers have their own offices, some work in group offices and some work in clinics. Other types of care centers include: Federally Qualified Health Centers (FQHCs): Plan members have the right to get services at these community-based health centers in our network.
What is the job of a PCP?
They may also do small procedures in the office. Internists: They take care of adults with a variety of medical problems. Obstetrician/gynecologists ( Ob/Gyns): They treat female health issues. They often serve as a PCP for women who are of childbearing age.
Where is AJ Murphy?
AJ Murphy is an evocative young writer who grew up in Boston's Charlestown neighborhood. AJ began his writing career at Alaska Ice Rinks Inc. in Anchorage, AK, where he also drove a Zamboni and took care of outdoor hockey rinks.
Need a provider directory?
If you’re looking for a provider directory in a different language, you can view our Spanish and Chinese versions. If you need a printed copy, you can request one.
Need help with Medicare enrollment?
Call a licensed agent at 1-855-335-1407 (TTY: 711) , Monday to Friday, 8 AM to 8 PM.
Get member help
Aetna members have access to contact information and resources specific to their plans.