If you qualify for Medicare because of a disability, your Initial Enrollment Period for a Medicare Advantage plan will consist of a 7-month period that begins three months before your 25th month of receiving disability benefits, includes your 25th month of receiving benefits and continues for another three months after your 25th month of receiving benefits.
Full Answer
Does Aetna have a Medicare Advantage plan?
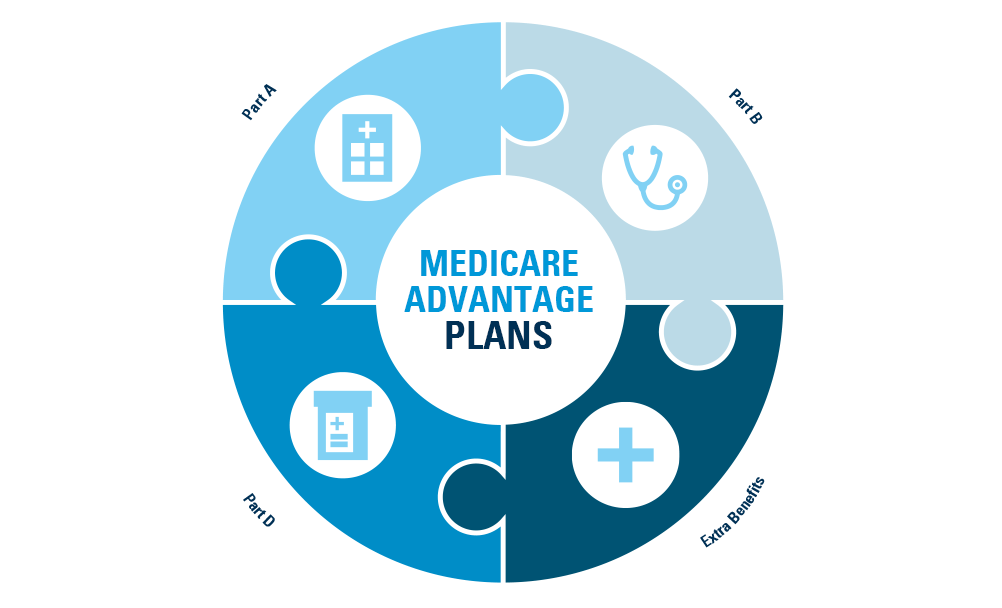
Depending on where you live, you may be able to enroll in one of the following types of Aetna Medicare Advantage plans: Aetna Medicare Advantage HMO (Health Maintenance Organization) plans may have lower costs than other types of Medicare Advantage plans because they use a contracted provider network to keep health-care expenses low.
What are Medicare Advantage plans does Aetna offer?
As mentioned, Aetna Medicare Advantage plans may offer extra benefits not normally covered by Original Medicare, including prescription drug coverage and routine vision or dental benefits. If you’d like to learn more about Aetna Medicare plan options, visit the Aetna page to find coverage that may fit your needs.
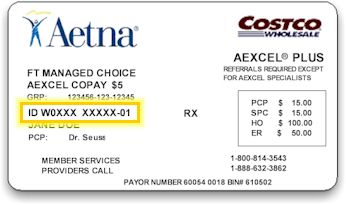
How do I verify Aetna?
Check your plan’s Evidence of Coverage (EOC) to see if or how these rules apply. Tip: If you’re viewing an EOC online, you can simply press Ctrl + F to search for an item. You can find most rules for referrals or prior authorizations in Chapter 4 — Benefits Chart — of the EOC. Check your claims.
What is the preferred pharmacy for Aetna?
The plan’s preferred pharmacy network comprises 4,200 Walmart, 580 Sam’s Club and 7,500 CVS/pharmacy locations. In addition to the preferred pharmacy network, members also can use any of the 52,700 pharmacies in the Aetna Medicare network.

Can you be denied a Medicare Advantage plan?
Generally, if you're eligible for Original Medicare (Part A and Part B), you can't be denied enrollment into a Medicare Advantage plan. If a Medicare Advantage plan gave you prior approval for a medical service, it can't deny you coverage later due to lack of medical necessity.
What are the criteria for Medicare Advantage?
Generally, you can get Medicare if one of these conditions applies: You are at least 65 years old. You are disabled and receive Social Security Disability Insurance (SSDI) or Railroad Retirement disability payments. You have End-Stage Renal Disease (ESRD) and require dialysis or a kidney transplant.
How do you qualify to get $144 back from Medicare?
How do I qualify for the giveback?Are enrolled in Part A and Part B.Do not rely on government or other assistance for your Part B premium.Live in the zip code service area of a plan that offers this program.Enroll in an MA plan that provides a giveback benefit.
Is Aetna Medicare considered an advantage plan?
Aetna Medicare Advantage D-SNPs Our dual-eligible Special Needs Plan (D-SNP) is a type of Medicare Advantage plan, available to people who have both Medicare and Medicaid. We can help you find out if you qualify.
What are the 3 requirements for Medicare?
Be age 65 or older; Be a U.S. resident; AND. Be either a U.S. citizen, OR. Be an alien who has been lawfully admitted for permanent residence and has been residing in the United States for 5 continuous years prior to the month of filing an application for Medicare.
Who is not eligible for Medicare?
Did not work in employment covered by Social Security/Medicare. Do not have 40 quarters in Social Security/Medicare-covered employment. Do not qualify through the work history of a current, former, or deceased spouse.
What is the $16 728 Social Security secret?
1:266:46My Review: Motley Fool's $16,728 Social Security Bonus - YouTubeYouTubeStart of suggested clipEnd of suggested clipIf you've read any of their articles you've probably seen this it says the sixteen thousand sevenMoreIf you've read any of their articles you've probably seen this it says the sixteen thousand seven hundred and twenty eight dollar social security bonus most retirees completely overlook.
How can I get more money from Social Security disability?
How to Maximize the Benefits You Receive from SSDIYou must have earned enough work credits through paying into Social Security.You must meet the SSA's disability definition and have been disabled (or be expected to be disabled) for at least a year.You must be unable to earn substantial gainful activity (SGA)
Who is eligible for Medicare Part B reimbursement?
1. How do I know if I am eligible for Part B reimbursement? You must be a retired member or qualified survivor who is receiving a pension and is eligible for a health subsidy, and enrolled in both Medicare Parts A and B.
Is Aetna Medicare Advantage the same as Medicare?
Both terms refer to the same thing. Instead of Original Medicare from the federal government, you can choose a Medicare Advantage plan (Part C) offered by a private insurance company. These plans include all of the benefits and services of Parts A and B. They may include prescription drug coverage as part of the plan.
Can I have Medicare and Aetna at the same time?
You will still be considered a Medicare beneficiary while enrolled in the Aetna MA plan, and you should always keep your Medicare enrollment card. However, when you seek medical care you will no longer have to file claims with Medicare first and then to Aetna as secondary.
What is the highest rated Medicare Advantage plan?
According to MoneyGeek's scoring system, the top-rated Medicare Advantage plans are Blue Cross Blue Shield for preferred provider organizations and UnitedHealthcare for health maintenance organizations.
How old do you have to be to qualify for Medicare?
You may be eligible for Medicare if: You are age 65 or older. You have a qualifying disability for which you have been receiving Social Security Disability Insurance (SSDI) for more than 24 months. You have been diagnosed with end-stage renal disease (permanent kidney failure requiring a kidney transplant or dialysis)
When do you sign up for Medicare?
As an example, you can first sign up for Medicare during the 7-month period that begins 3 months before the month you turn 65, includes the month you turn 65, and ends 3 months after the month you turn 65. If you sign up for Medicare during the first 3 months of your Initial Enrollment Period, in most cases, your coverage starts the first day ...
Medicare Eligibility for People With Disabilities
Even if you’re under the age of 65, you can qualify for Medicare if you have certain disabilities. You may be eligible for Medicare coverage if any of the following apply to you:
Enrolling in Medicare With a Disability
In some cases, you’ll be automatically enrolled in Medicare Parts A and B, also known as Original Medicare, if you have a disability.
How Much Does Medicare Cost?
Your out-of-pocket costs will depend on which Medicare coverage you have. Medicare Part A typically costs nothing, but you may have to pay an annual premium if you didn’t pay Medicare taxes for enough quarters through your work. Medicare Part B, Part C, and Part D all have separate premiums and deductibles.
Medicare Resources for People With Disabilities
If you need help determining if you’re eligible for Medicare, navigating the Medicare enrollment process, or understanding how Medicare coverage works with SSDI or RRB disability benefits, consult the resources below.
FAQs About Medicare for People With Disabilities
The Medicare guidelines can be confusing, especially if you’re under the age of 65 and need to know if you qualify for coverage because you have ALS, ESRD, or another disability. Below you’ll find answers to some of the most frequently asked questions about Medicare for a person with a disability.
What conditions are considered to be eligible for Medicare?
Even though most people on Social Security Disability Insurance must wait for Medicare coverage to begin, two conditions might ensure immediate eligibility: end-stage renal disease (ESRD) and Lou Gehrig’s disease (ALS).
When will Medicare be available for seniors?
July 16, 2020. Medicare is the government health insurance program for older adults. However, Medicare isn’t limited to only those 65 and up—Americans of any age are eligible for Medicare if they have a qualifying disability. Most people are automatically enrolled in Medicare Part A and Part B once they’ve been collecting Social Security Disability ...
What is ESRD in Medicare?
ESRD, also known as permanent kidney failure, is a disease in which the kidneys no longer work. Typically, people with ESRD need regular dialysis or a kidney transplant (or both) to survive. Because of this immediate need, Medicare waives the waiting period. 2
What to do if your income is too high for medicaid?
If your income is too high to qualify for Medicaid, try a Medicare Savings Program (MSP), which generally has higher limits for income. As a bonus, if you qualify for an MSP, you automatically qualify for Extra Help, which subsidizes your Part D costs. Contact your state’s Medicaid office for more information.
How long does it take to get Medicare if you appeal a decision?
The result: your wait for Medicare will be shorter than two years.
How long does a disability last?
The government has a strict definition of disability. For instance, the disability must be expected to last at least one year. Your work history will also be considered—usually, you must have worked for about 10 years but possibly less depending on your age.
Does Medicare cover ALS?
Medicare doesn’t require a waiting period for people diagnosed with ALS, but they need to qualify based on their own or their spouse’s work record. 3
What is Medicare Advantage HMO?
With our Medicare Advantage HMO plans, you typically choose a primary care physician who helps coordinate your care within a network of doctors and hospitals. It’s Medicare coverage that can help you get the right care at the right time. Read More Read Less.
What is dual eligible special needs?
Our dual-eligible Special Needs Plan is a type of Medicare Advantage plan that offers extra benefits, available to anyone who has both Medicare and Medicaid. We can help you find out if you qualify.
Can you see out of network providers with Medicare Advantage?
With our Medicare Advantage HMO-POS plans, you have the flexibility to see out-of-network providers for certain services. You may pay more when you go out of network. It’s a coordinated approach to your Medicare coverage that may give you more options.
Is SilverScript a Medicare plan?
Enrollment in our plans depends on contract renewal. SilverScript is a Prescription Drug Plan with a Medicare contract marketed through Aetna Medicare. Enrollment in SilverScript depends on contract renewal. (Effective 1/2021)
Is Aetna a PPO?
Aetna Medicare is a HMO, PPO plan with a Medicare contract. Our SNPs also have contracts with State Medicaid programs. Enrollment in our plans depends on contract renewal. SilverScript is a Prescription Drug Plan with a Medicare contract marketed through Aetna Medicare.
Dental, vision and hearing
Original Medicare doesn’t include routine dental, vision and hearing benefits like checkups, exams, eyeglasses and hearing aids. But most of our plans do.
Benefits that fit your life
We know you want to keep doing what you love. That’s why all of our Medicare Advantage plans offer you benefits and services that can help you:
Benefits for your total health
We want to help make life easier for you. From prescription mail-order service* and a 24-Hour Nurse Line, to no-added-cost annual flu shots, the extra benefits included in many of our plans offer you real convenience:
Benefits that may surprise you
Many of our plans include benefits that help take care of the whole you. And in ways you might not expect.
How old do you have to be to qualify for Medicare Advantage?
To be eligible to apply for a Medicare Advantage plan prior to turning 65 years old, you must first qualify for Original Medicare. This typically requires that you meet the following criteria:
What are the benefits of Medicare Advantage?
Some Medicare Advantage plans may offer additional benefits that are not covered by Medicare, such as dental care, vision care, hearing care, prescription drugs and more. Someone with a disability may find that these additional benefits fit their health coverage needs.
How long is the waiting period for Medicare Part A?
Note: If you receive disability benefits because of Amyotrophic Lateral Sclerosis (ALS), the 24-month waiting period is voided and you will be automatically enrolled in Medicare Part A and Part B the first month that you receive disability benefits.
What is a special enrollment period?
There is also an opportunity for people under 65 who are already enrolled in a Medicare Advantage plan to change to a different plan or drop their Medicare Advantage plan coverage entirely. A Special Enrollment Period may be granted at any time throughout the year under certain circumstances.
What is a SNP plan?
A Medicare Special Needs Plan (SNP) is a type of Medicare Advantage plan that limits membership to people who live with specific diseases or characteristics. The benefits, provider choices and drug formularies tied to the plan may then be tailored to meet the specific needs of the members they serve.
What is SSI disability?
Supplemental Security Income (SSI), which is different from Social Security Disability Income, pays benefits to disabled people who can in turn use those benefits to help pay for Medicare Advantage costs.
When does Medicare start to send out a 24-month disability check?
The 24-month period begins the first month you receive a disability check. At the beginning of the 25th month of receiving benefits, you will be automatically enrolled in Medicare Part A and Part B. Your Medicare card should arrive in the mail three months prior to your 25th month of receiving benefits.