Your PCP will issue referrals to participating specialists and facilities for certain services. For some services, your PCP is required to obtain prior authorization from Aetna Medicare. You’ll need to get a referral from your PCP for covered, non‐emergency specialty or hospital care, except in an emergency and for certain direct‐access service.
Full Answer
How do I get a referral for Aetna Medicare?
Referrals are not required for Medicare Advantage HMO members As of January 1, 2020, all Aetna Medicare Advantage health maintenance organization (HMO) members in Washington have direct access to in-network Medicare HMO network providers. We no longer require primary care providers to submit referral requests to us.
Do Aetna Medicare Advantage plans require a provider network?
• Referrals aren’t required for direct-access services, such as routine eye care and ob/gyn services. Refer to our Office Manual for Health Care Professionals for a list of direct-access specialties. • If you’re part of an independent practice association (IPA), follow current referral procedures for members HMO plans. Aetna.com 7
Did Aetna change its PCP referral requirements for commercial plans?
Jan 05, 2022 · Aetna Medicare Advantage plans at a glance. Our HMO plans. Requires you to use a provider network. Yes, unless it’s an emergency. Requires you to have a primary care physician (PCP) Yes, in many plans. Requires referral to see a specialist. Some plans. Monthly premiums.
Does Aetna review precertification requests?
Feb 24, 2022 · For some services, your PCP is required to obtain prior authorization from Aetna Medicare. You’ll need to get a referral from your PCP for covered, non‐emergency specialty or hospital care, except in an emergency and for certain direct‐access service. There are exceptions for certain direct access services.

Does Aetna Medicare assure require referrals?
Patients are encouraged, but not required, to choose and use a participating PCP. PCP referrals are not required.
Does Aetna Medicare PPO require prior authorization?
For some services, your PCP is required to obtain prior authorization from Aetna Medicare. You'll need to get a referral from your PCP for covered, non‐emergency specialty or hospital care, except in an emergency and for certain direct‐access service. There are exceptions for certain direct access services.Feb 24, 2022
How do you send a referral to Aetna?
Visit www.aetnaelectronicprecert.com to check if a service requires precertification. To request a referral, you must be: A participating Aetna provider designated as a PCP - Note: The PCP making the referral must participate in the member's benefits plan.
Is Aetna Medicare the same as Medicare?
Both terms refer to the same thing. Instead of Original Medicare from the federal government, you can choose a Medicare Advantage plan (Part C) offered by a private insurance company.Oct 1, 2021
What is the difference between precertification and prior authorization?
Sometimes called prior authorization, prior approval or precertification. Your health insurance or plan may require preauthorization for certain services before you receive them, except in an emergency. Preauthorization isn't a promise your health insurance or plan will cover the cost.
How long does it take to get a pre authorization from Aetna?
You and your provider will get a letter stating whether the service has been approved or denied. We will make a decision within 5 business days, or 72 hours for urgent care.
How do I get Aetna remittance advice?
the EFT payment or ERA remittance advice, contact your Provider Relations representative at 1-855-772-9076 or email us at [email protected], or fax us at 1-844-886-8349.
Does Aetna Open Access select require a referral?
The Aetna Open Access Plan is an HMO that gives members more freedom. Members can visit any in-network provider (PCP or specialist) for covered services without a referral.
What type of insurance is Aetna Medicare?
Aetna is one of the largest private insurance companies that offers Medicare Advantage plans. Aetna offers HMO, HMO-POS, PPO, and D-SNP plans. Not all of Aetna's Medicare Advantage plans may be available in your area.
Is Medicare primary or Aetna?
Even if you have a group health plan, Medicare is the primary insurer as long as you've been eligible for Medicare for 30 months or more.
Is Aetna a Medicare Advantage Plan?
Aetna Medicare Advantage plans take a total approach to health. Our Part C plans often include prescription drug coverage and extra benefits. And many feature an affordable plan premium – sometimes as low as $0. Error or missing data.Jan 6, 2022
What does Medicare not pay for?
In general, Original Medicare does not cover: Long-term care (such as extended nursing home stays or custodial care) Hearing aids. Most vision care, notably eyeglasses and contacts. Most dental care, notably dentures.
How does Medicare Advantage HMO work?
How do Medicare Advantage HMO plans work? A health maintenance organization (HMO) gives you access to a network of doctors and hospitals that you must use in most cases. Some HMO plans require you to get a referral from a primary care physician for hospital care and specialist visits.
What is a D-SNP?
Our dual-eligible Special Needs Plan (D-SNP) is a type of Medicare Advantage plan, available to people living in our service area who have both Medicare and Medicaid. We can help you find out if you qualify.
Does Aetna offer Medicare Advantage?
Medicare Advantage plans for every need. In addition to HMO plans, Aetna offers you other Medicare Advantage plan options — some with a $0 monthly plan premium. We can help you find a plan that’s right for you.
Does Aetna offer HMO?
In addition to HMO plans, Aetna offers you other Medicare Advantage plan options — some with a $0 monthly plan premium. We can help you find a plan that’s right for you.
Does Aetna require a primary care physician?
Our HMO plans. Requires you to use a provider network. Yes, unless it’s an emergency. Requires you to have a primary care physician (PCP) Yes, in many plans. Requires referral to see a specialist. Some plans. Monthly premiums.
What is a referral for medical care?
Sometimes you need a referral or prior authorization before you can get care. A referral is a kind of preapproval from your primary care doctor to see a specialist. A prior authorization or precertification is when your doctor has to get approval from us before we cover an item or service.
What is telehealth coverage?
Telehealth coverage. Telehealth – or telemedicine – means virtual care you can get at home or away. These visits are live, video conferences between you and a doctor over a computer or smart phone. Consider using telehealth when you have a time sensitive medical need or can’t get to the doctor in person.
What is prior authorization?
Prior authorizations are often used for things like MRIs or CT scans. Your doctor is in charge of sending us prior authorization requests for medical care. Each plan has rules on whether a referral or prior authorization is needed. Check your plan’s Evidence of Coverage (EOC) to see if or how these rules apply.
Does Aetna cover out of network providers?
If you’re enrolled in a standard Aetna Medicare Plan (HMO) If you get coverage from an out‐of‐network provider, your plan won’t cover their charges. Medicare and Aetna Medicare won’t be responsible either. Generally, you must get your health care coverage from your primary care physician (PCP).
What is Aetna insurance?
Aetna is the brand name used for products and services provided by one or more of the Aetna group of companies, including Aetna Life Insurance Company and its affiliates (Aetna). Health benefits and health insurance plans contain exclusions and limitations. See all legal notices. Additional FAQs. COVID-19 vaccine.
How long does a health insurance authorization last?
Authorizations will remain in effect until the end of the plan year. Authorization may be extended beyond the plan year, for a period of six months, if continued eligibility can be confirmed. However, at this time there are some states that have issued orders prohibiting elective procedures. Health care providers are responsible for complying ...
Is Aetna Inc. responsible for the content of its websites?
Aetna Inc. and its subsidiary companies are not responsible or liable for the content, accuracy, or privacy practices of linked sites, or for products or services described on these sites. Links to various non-Aetna sites are provided for your convenience only.
Is Aetna a part of CVS?
and its subsidiary companies are not responsible or liable for the content, accuracy or privacy practices of linked sites, or for products or services described on these sites. Aetna is proud to be part of the CV S Health family . You are now being directed to the CVS Health site.
What is Aetna insurance?
Aetna is the brand name used for products and services provided by one or more of the Aetna group of companies, including Aetna Life Insurance Company and its affiliates (Aetna). Health benefits and health insurance plans contain exclusions and limitations. See all legal notices.
Can you transition Part D drugs?
Members who are taking Part D drugs that are not on the plan's formulary, or that are subject to utilization management requirements, can get a transition supply of their drug under certain circumstances. They can work with you to complete a successful transition and avoid disruption in treatment.
Does Medicare Part D cover drugs?
Any health care professional who prescribes drugs to patients with Part D plans must now enroll in the Medicare program or opt out. If you do not enroll or opt out, Medicare Part D may no longer cover these drugs as of February 1, 2017. Please try to enroll or opt out by November 1, 2016.
Is Aetna a Medicare Supplement?
The Aetna Supplemental Retiree Medical Plan is a fully insured, non-network-based commercial retiree group health product. In all states but Florida and Minnesota, it is offered as a supplementary medical plan, not a Medicare plan. In Florida and Minnesota, it is approved as a group Medicare Supplement product.
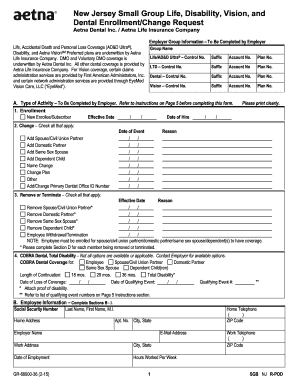
Find the forms you need
Print and complete this form for medical, dental, vision, hearing, or vaccine reimbursement.
Call us
Aetna handles premium payments through InstaMed, a trusted payment service. Your InstaMed log-in may be different from your Caremark.com secure member site log-in.
What is Aetna insurance?
Aetna is the brand name used for products and services provided by one or more of the Aetna group of companies, including Aetna Life Insurance Company and its affiliates (Aetna). Health benefits and health insurance plans contain exclusions and limitations. See all legal notices.
Why is availabilty important?
Availity helps you spend less time on administration so you can focus more on patient care. You get a self-service portal to quickly check on benefits eligibility and many other key tasks you do every day.
Is Aetna Inc. responsible for the content of its websites?
Aetna Inc. and its subsidiary companies are not responsible or liable for the content, accuracy, or privacy practices of linked sites, or for products or services described on these sites. Links to various non-Aetna sites are provided for your convenience only.
Is Aetna a part of CVS?
and its subsidiary companies are not responsible or liable for the content, accuracy or privacy practices of linked sites, or for products or services described on these sites. Aetna is proud to be part of the CV S Health family . You are now being directed to the CVS Health site.