:no_upscale()/cdn.vox-cdn.com/uploads/chorus_asset/file/10622325/Screenshot_2018_04_10_08.50.00.png)
Current estimates are that Medicare will run out of funding for hospital insurance as soon as 2026, and other parts of Medicare aren’t that far behind. Because of changing economies and the aforementioned longer life spans of Americans, Medicare looks to be heading toward insolvency sooner rather than later.
Full Answer
What is the future of Medicare Advantage plans?
Steven Nelson, CEO of Medicare Advantage plan provider UnitedHealthcare, predicted that 50% of seniors will soon be enrolled in a Medicare Advantage plan. 4 Nobody knows for sure what the future will hold, but there are plenty of reasons to be optimistic about the future of Medicare Advantage plans.
How will Medicare spending change in the future?
Over a 40-year period, the majority of Medicare spending has moved from inpatient spending to managed care organization spending. According to Stipalnic, Medicare spending factors will continue to shift in the future as other healthcare services increase in utilization within the Medicare ecosystem.
Will Medicare stop paying for hospital insurance in eight years?
It doesn’t mean Medicare will stop paying hospital insurance benefits in eight years. We don’t know what Congress will do—though the answer is probably nothing until the last minute. Lawmakers could raise the payroll tax.
When will Medicare costs flatten out?
In that case, the trustees forecast Medicare costs will not flatten out in the mid-2030s, and instead keep rising—to 8 percent of GDP by 2070 and 9 percent of the entire economy by 2090. That’s a long way away, you may say, and a lot can happen in the next 75 years.
Will there be Medicare in the future?
After a 9 percent increase from 2021 to 2022, enrollment in the Medicare Advantage (MA) program is expected to surpass 50 percent of the eligible Medicare population within the next year. At its current rate of growth, MA is on track to reach 69 percent of the Medicare population by the end of 2030.
Why is it anticipated that Medicare spending will increase over the next 10 years?
Medicare per capita spending is projected to grow at an average annual rate of 5.1 percent over the next 10 years (2018 to 2028), due to growing Medicare enrollment, increased use of services and intensity of care, and rising health care prices.
What will Medicare cost in 2030?
$1.72 trillionMedicare cost $775 billion in 2019, and is projected to grow to $1.2 trillion by 2025, and $1.72 trillion by 2030.
What challenges will Medicare face in the future?
Financing care for future generations is perhaps the greatest challenge facing Medicare, due to sustained increases in health care costs, the aging of the U.S. population, and the declining ratio of workers to beneficiaries.
What is the expected growth of Medicare beneficiaries by the year 2030?
The Congressional Budget Office (CBO) projects that the share of all Medicare beneficiaries enrolled in Medicare Advantage plans will rise to about 51 percent by 2030. This analysis has been updated to reflect changes in methodology in how KFF calculates the total number of Medicare beneficiaries.
How Long Will Medicare be funded?
The trust fund for Medicare Part A will be able to pay full benefits until 2026 before reserves will be depleted. That's the same year as predicted in 2020, according to a summary of the trustees 2021 report, which was released on Tuesday.
How will baby boomers retiring affect healthcare?
The Impact of Baby Boomers on Health Care By 2020, retiring baby boomers are expected to more than double Medicare and Medicaid costs. As a result, some pundits anticipate that the Trust Fund will be bankrupt by 2033. Meanwhile, taxes will cover only 48 percent of the associated health care costs.
How much did Medicare cost in 2021?
$696 billionWhat is the spending on Medicare? In FY 2021 the federal government spent $696 billion on Medicare.
Why are Social Security and Medicare spending expected to increase?
The rise in Social Security and Medicare spending over time reflects an aging population and rising health care costs. Combined spending for these two programs is projected to rise from 7.9 percent of GDP in 2019 to 10.3 percent by 2029, well above the average over the past 40 years of 6.5 percent.
Will Medicare ever go away?
Medicare is not going bankrupt. It will have money to pay for health care. Instead, it is projected to become insolvent. Insolvency means that Medicare may not have the funds to pay 100% of its expenses.
What are some of the biggest challenges with Medicare today?
Top concerns for Medicare beneficiaries: Part B, appeals and affordable medications. The top concerns of Medicare enrollees include navigating Part B, appealing Medicare Advantage (MA) denials and affording meds, according to an annual report from the Medicare Rights Center.
Is Medicare running out of money?
A report from Medicare's trustees in April 2020 estimated that the program's Part A trust fund, which subsidizes hospital and other inpatient care, would begin to run out of money in 2026.
What are the two trust funds for Medicare?
The Medicare program has two separate trust funds: the Hospital Insurance Trust Fund (HI) and the Supplementary Medical Insurance Trust Fund (SMI). The Social Security Act established the Medicare Board of Trustees to oversee the financial operations of the HI and SMI trust funds.1
Is Medicare running out of money?
In the following video, Barkett assures us that the Medicare program is not destined to run out of money, and that there are both legislative changes and trends in health care that change over time to help ensure Medicare remains intact for the future.
When was Medicare created?
Medicare was created in 1965 as a means to address the sudden explosion in births that followed the end of WWII. The so-called Baby Boomers are a generation that makes up the bulk of Medicare recipients in 2020, and more are retiring and taking advantage of Medicare every single day.
What is Medicare benefits?
Medicare benefits provide access to affordable healthcare for millions of seniors and those with certain disabilities in the United States, meaning the future of this vital program is often on the minds of recipients.
Why is Medicare going into insolvency?
Because of changing economies and the aforementioned longer life spans of Americans, Medicare looks to be heading toward insolvency sooner rather than later. Combine this with lower birth rates in the United States in the current generation, and it seems like some major changes will need to be put into place in order to bring ...
Is Medicare going to be viable in the future?
In recent decades, there have been a number of concerns as to the viability of Medicare in the future, both in terms of financing the program and ensuring that its liabilities are covered. These concerns raise the question as to how long Medicare can continue in its current configuration, but they also cause potential future recipients ...
Is it a good time to discuss Medicare benefits?
Whether you currently receive Medicare benefits or you will be taking advantage of Medicare coverage in the future, now would be a good time to discuss your needs and options with a Medicare plan administrator. These professionals will be able to guide you in selecting the options that are right for you now, but they will also be able ...
What is the role of Medicare in the future?
Medicare plays a central role in broader discussions about the future of entitlement programs. Together, Medicare, Medicaid and Social Security account for more than 40 percent of the federal budget.
When did Medicare start?
Before Medicare was signed into law in 1965, about half of all seniors lacked hospital insurance. Today, virtually all people ages 65 and over are covered by Medicare. Medicare is a popular program, but faces a number of issues and challenges in the years to come. A critical challenge is how to finance care for future generations without unduly ...
What is Medicare Advantage?
Medicare beneficiaries have the option to get their benefits through the traditional fee-for-service (FFS) program – sometimes called Original Medicare – or through private health plans, such as health maintenance organizations (HMOs) and preferred provider organizations (PPOs) – currently called Medicare Advantage.
What is the source of Medicare funding?
Medicare funding comes primarily from three sources: payroll tax revenues, general revenues, and premiums paid by beneficiaries.
How does Medicare affect spending?
Annual growth in Medicare spending is largely influenced by the same factors that affect health spending in general: increasing prices of health care services, increasing volume and utilization of services, and new technologies. In the past, provider payment reforms, such as the hospital prospective payment system, ...
What is Medicare and Social Security?
Like Social Security, Medicare is a social insurance program that provides health coverage to individuals, without regard to their income or health status.
Why is Medicare facing a challenge?
Financing care for future generations is perhaps the greatest challenge facing Medicare, due to sustained increases in health care costs, the aging of the U.S. population, and the declining ratio of workers to beneficiaries. Annual increases in health care costs are placing upward pressure on Medicare spending, as for other payers.
How many Medicare Advantage plans are there in 2020?
By 2020, that number increased to 3,148. Also in 2020, the average Medicare beneficiary can choose from 28 available plan options, compared to only 18 plan options in 2014. 1. Many Medicare Advantage plans offer $0 premiums. With more Medicare Advantage plan options being sold by more providers, the increased competition between insurance companies ...
How many Medicare beneficiaries were there in 2003?
Based on current trends, here are four predictions Medicare beneficiaries can keep an eye on. In 2003, just over five million Medicare beneficiaries enrolled in a Medicare Advantage plan, which represented only 13 percent of the total Medicare beneficiary population.
Is Humana a Medicare Advantage?
Humana, one company that provides Medicare Advantage plans, pulled out of the individual health insurance exchange in 2018 to invest more heavily in the Medicare Advantage program. 3.
Does Medicare have a star rating?
In addition to the bonus program, Medicare issues star ratings for all Medicare Advantage plans each year, and these Medicare Star Ratings can be a large point of emphasis for shoppers. 2. Medicare offers a Special Enrollment Period for anyone who is not enrolled in a five-star Medicare Advantage plan (the highest Medicare Star Rating) ...
Is Medicare Advantage plan going to drop?
Medicare Advantage plan prices should remain stable or possibly drop. The number of available Medicare Advantage plan options in the U.S. is on the rise. In 2012, there were a total of 1,974 Medicare Advantage plans available nationwide. By 2020, that number increased to 3,148.
Who is the CEO of UnitedHealthcare?
Steven Nelson, CEO of Medicare Advantage plan provider UnitedHealthcare, predicted that 50% of seniors will soon be enrolled in a Medicare Advantage plan. 4.
Does Medicare Advantage offer the same benefits as Original Medicare?
Medicare Advantage plans offer the same benefits that are covered by Medicare Part A and Part B (Original Medicare), and many Medicare Advantage plans offer additional benefits not covered by Original Medicare. These additional benefits can serve as an incentive to consumers.
When will Medicare deplete?
June 06, 2018 - The Medicare Board of Trustees (MBT)’s latest report anticipates that Medicare’s Hospital Insurance (HI) Trust Fund will deplete by the year 2026 as Medicare spending continues to outgrow the trust’s collective revenues.
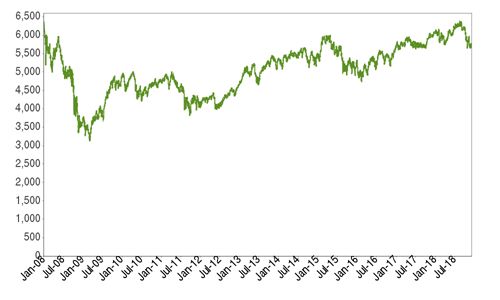
How much did Medicare spend in 2017?
In 2017, Medicare covered 58 million beneficiaries and spent a total of $710.2 billion to cover services across all of Medicare.
When will the HI fund deplete?
CMS Chief Actuary Paul Spitalnic told attendees during an American Enterprise Institute (AEI) event that the HI Fund will deplete in the next eight years as the fund’s income streams weaken to a point where it can no longer cover beneficiary care costs.
Does the repeal of the Affordable Care Act affect Part A?
Spitalnic briefly mentioned that the repeal of the Affordable Care Act’s individual mandate would likely exacerbate care costs under Part A. “A repeal of the individual mandate is expected to lead to a higher number of uninsured and will result in a higher number of uncompensated payments to hospitals,” he added.
Does Medicare continue to shift?
Medicare’s spending factors also continue to shift, Spitalnic explained, since the program has gradually moved from primarily covering inpatient costs to a broader range of services. Over a 40-year period, the majority of Medicare spending has moved from inpatient spending to managed care organization spending.
When did Medicare change to Medicare Access and CHIP?
But that forecast is built on several key assumptions that are unlikely to occur. In the 2010 Affordable Care Act, Congress adopted a package of cost-cutting measures. In 2015, in a law called the Medicare Access and CHIP Reauthorization Act (MACRA), it began to change the way Medicare pays physicians, shifting from a system that pays by volume to one that is intended to pay for quality. As part of the transition, MACRA increased payments to doctors until 2025.
How is Medicare funded?
Rather, they are funded through a combination of enrollee premiums (which support only about one-quarter of their costs) and general revenues —another way of saying the government borrows most of the money it needs to pay for Medicare.
Why did Medicare build up a trust fund?
Because it anticipated the aging Boomers, Medicare built up a trust fund while its costs were relatively low. But that reserve is rapidly being drained, and, in 2026, will be out the money. That is the source of all those “going broke” headlines.
Is Medicare healthy?
Not broke, but not healthy. However, that does not mean Medicare is healthy. Largely because of the inexorable aging of the Baby Boomers, program costs continue to grow. And, as the Trustee’s report forthrightly acknowledges, long-term costs could well increase even faster than the official predictions.
Will Medicare go out of business in 2026?
No, Medicare Won't Go Broke In 2026. Yes, It Will Cost A Lot More Money. Opinions expressed by Forbes Contributors are their own. It was hard to miss the headlines coming from yesterday’s Medicare Trustees report: Let’s get right to the point: Medicare is not going “broke” and recipients are in no danger of losing their benefits in 2026.
Will Medicare stop paying hospital insurance?
It doesn’t mean Medicare will stop paying hospital insurance benefits in eight years. We don’t know what Congress will do—though the answer is probably nothing until the last minute. Lawmakers could raise the payroll tax.
Will Medicare be insolvent in 2026?
Government Says Medicare won't be able to cover costs by 2026. Report puts Medicare insolvency sooner than forecast. Let’s get right to the point: Medicare is not going “broke” and recipients are in no danger of losing their benefits in 2026.
When was Medicare expanded?
For example, Medicare was expanded in 1972 to cover the disabled, people over 65, and others. Medicare includes more benefits today, including limitless home health visits and quality standards for Medicare-approved nursing homes. Medicaid has also been expanded to cover a larger group than initially intended.
What is the complexity of health insurance?
About half of Americans who have private health insurance are covered under self-insured plans, each with their own design. The other half of the insured population is covered under traditional indemnity plans, Health Maintenance Organizations (HMOs), or Preferred Provider Organizations (PPOs). The one commonality among all insurance plans is how dramatically they vary. Deductibles, co-insurance, co-payments, and maximum out-of-pocket expenses are a few of the inconsistent variables among insurance plans. Additionally, some insurance companies are for-profit and others are not-for-profit, indicating another point of confusion.
How did the Bubonic Plague affect the healthcare system?
The bubonic plague is a good example of a disease that can drastically change the healthcare system by quickly shifting all resources to handle an epidemic. In the Middle Ages, the Black Death spread so quickly across Europe that it is responsible for an estimated 75 million deaths.
Why is there wide variation in Medicaid?
Wide variations in Medicaid programs across the nation occur because individual states have the ability to tailor Medicaid programs to serve the needs of their residents. In 2010, the Affordable Care Act introduced the Health Insurance Marketplace, which has had a direct impact on Medicaid service.
What are the factors that contribute to healthcare change?
Complex and slow-to-change policies are an obvious factor, but environmental and technological factors also contribute to changes in healthcare. Illness trends, doctor demographics, and technology also contribute to shifts in our overall healthcare system.
Why does demand change in healthcare?
Demands on healthcare change due to various reasons, including the needs of patients. Every year, new cures and treatments help manage common diseases. Each such development affects the entire healthcare system as much as it has a positive impact on patients.
Why are providers important?
Providers are an important part of the healthcare system and any changes to their education, satisfaction or demographics are likely to affect how patients receive care. Future healthcare providers are also more likely to focus their education on business than ever before.