Full Answer
What are the best insurance companies for Medicare?
Top 10 Medicare Supplement Insurance Companies in 2021
- Aetna Medicare Supplements
- Cigna Medicare Supplements
- Mutual of Omaha Medicare Supplements
- Manhattan Life Medicare Supplements
- Bankers Fidelity Medicare Supplements
- Blue Cross Blue Shield Medicare Supplements
- Western United Life Medicare Supplements
- Anthem Medicare Supplements
- United Healthcare Medicare Supplements
- Combined Medicare Supplements
How to deal with Medicare as a secondary insurance?
- Vision: Your medical plan will not cover you for vision care. ...
- Dental: A dental plan can cover you for preventive care such as routine teeth cleanings and some X-rays. ...
- Disability: Short- and long-term disability plans are a type of secondary insurance coverage. ...
Will my secondary insurance be compatible with Medicare?
The one that pays second (secondary payer) only pays if there are costs the primary insurer didn't cover. The secondary payer (which may be Medicare) may not pay all the uncovered costs. If your group health plan or retiree health coverage is the secondary payer, you may need to enroll in Medicare Part B before your insurance will pay.
What is the best supplemental insurance plan for Medicare?
Fort Worth, Jan. 31, 2022 (GLOBE NEWSWIRE) -- Fort Worth, Texas - Boomer Benefits, an award-winning insurance agency ... to look into getting a Medicare Supplement plan. Since Original Medicare ...

What is the best secondary insurance if you have Medicare?
Best Medicare Supplement Insurance Companies of 2022Best Overall: Mutual of Omaha.Best User Experience: Humana.Best Set Plans and Coverage: AARP.Best Medigap Coverage Information: Aetna.Best Discounts for Multiple Policyholders: Cigna.
Is it necessary to have supplemental insurance with Medicare?
For many low-income Medicare beneficiaries, there's no need for private supplemental coverage. Only 19% of Original Medicare beneficiaries have no supplemental coverage. Supplemental coverage can help prevent major expenses.
Who is the largest Medicare Supplement insurance company?
UnitedHealthCareAARP/United Health Group has the largest number of Medicare Supplement customers in the country, covering 43 million people in all 50 states and most U.S. territories. AARP licenses its name to insurer UnitedHealthCare, which helps make these policies so popular.
Can you have both Medicare and a Medicare Advantage plan?
In most types of Medicare Advantage Plans, you can't join a separate Medicare drug plan. In most cases, you don't have to get a service or supply approved ahead of time for Original Medicare to cover it.
How much do most seniors pay for Medicare?
Most people don't pay a monthly premium for Part A (sometimes called "premium-free Part A"). If you buy Part A, you'll pay up to $499 each month in 2022. If you paid Medicare taxes for less than 30 quarters, the standard Part A premium is $499.
What are the negatives of a Medicare Advantage plan?
Medicare Advantage can become expensive if you're sick, due to uncovered copays. Additionally, a plan may offer only a limited network of doctors, which can interfere with a patient's choice. It's not easy to change to another plan. If you decide to switch to a Medigap policy, there often are lifetime penalties.
What are the top 3 most popular Medicare Supplement plans in 2021?
Three Popular Medicare Supplement PlansBlue Cross Blue Shield. According to Blue Cross Blue Shield (BCBS), Plans F and N are available in most areas. ... AARP United Healthcare. The United Healthcare Medicare Supplement plan is also very popular. ... Humana.
Who has the cheapest Medicare supplement insurance?
What's the least expensive Medicare Supplement plan? Plan K is the cheapest Medigap plan, with an average cost of $77 per month for 2022.
What insurance companies work with Medicare?
Best Medicare Advantage Providers RatingsProviderForbes Health RatingsCoverage areaBlue Cross Blue Shield5.0Offers plans in 48 statesCigna4.5Offers plans in 26 states and Washington, D.C.United Healthcare4.0Offers plans in all 50 statesAetna3.5Offers plans in 44 states1 more row•Feb 25, 2022
Which two Medicare plans Cannot be enrolled together?
You generally cannot enroll in both a Medicare Advantage plan and a Medigap plan at the same time.
Do you still pay Medicare Part B with an Advantage plan?
You continue to pay premiums for your Medicare Part B (medical insurance) benefits when you enroll in a Medicare Advantage plan (Medicare Part C). Medicare decides the Part B premium rate. The standard 2022 Part B premium is estimated to be $158.50, but it can be higher depending on your income.
What are 4 types of Medicare Advantage plans?
Below are the most common types of Medicare Advantage Plans.Health Maintenance Organization (HMO) Plans.Preferred Provider Organization (PPO) Plans.Private Fee-for-Service (PFFS) Plans.Special Needs Plans (SNPs)
Is it worth it to get supplemental life insurance?
Supplemental life insurance can be a useful add-on, particularly if health conditions make it tough for you to get enough coverage elsewhere. But be sure to compare policies and prices. In some cases, the benefits may not be worth the cost.
What is the cost of supplemental insurance for Medicare?
In 2020, the average premium for Medicare supplemental insurance, or Medigap, was approximately $150 per month or $1,800 per year, according to Senior Market Sales, a full-service insurance organization.
What is the difference between Medicare supplemental plans and Medicare Advantage plans?
Medicare Advantage and Medicare Supplement are different types of Medicare coverage. You cannot have both at the same time. Medicare Advantage bundles Part A and B often with Part D and other types of coverage. Medicare Supplement is additional coverage you can buy if you have Original Medicare Part A and B.
What is the difference between Medicare Advantage and Medigap?
Medigap is supplemental and helps to fill gaps by paying out-of-pocket costs associated with Original Medicare while Medicare Advantage plans stand in place of Original Medicare and generally provide additional coverage.
What is secondary coverage for health insurance?
Secondary health insurance policies can fill in any coverage gaps, such as vision coverage, and available policies can also reduce the cost of heal...
Can you have two health insurance plans at the same time?
Yes, it's common to have multiple health insurance policies, and dual coverage can help cover more of your medical costs so that you pay less out o...
Which insurance companies offer secondary health insurance?
Plans are available from Blue Cross Blue Shield, USAA, AARP, UnitedHealthcare, Aetna, Aflac, Alliance, Humana, Cigna and more.
Is secondary health insurance worth it?
Secondary health insurance can give you financial protection if your main insurance policy has limitations. Most people have some form of secondary...
How To Shop & Compare Medicare Supplement Plans
Researching the plan thats right for you is key to getting the coverage you need. Each plan offers specific benefits depending on your state, which benefits you desire, and the costs.
Is Supplemental Insurance Worth It
It depends. Most seniors do supplement Medicare in some way. Those that dont have access to group health coverage will often invest in a Medigap policy to supplement Original Medicare or Medicare Advantage plan in lieu of Original Medicare. The right choice between these two really hinges on what you need.
Compare Medicare Supplement Insurance Plans
Many or all of the products featured here are from our partners who compensate us. This may influence which products we write about and where and how the product appears on a page. However, this does not influence our evaluations. Our opinions are our own. Here is a list of our partners and here’s how we make money.
Best Medicare Supplement Companies
Unlike health insurance, where policies differ among providers, Medicare supplement plans are standardized so that the benefits for each plan letter are the same for each company. This means that Medicare supplement Plan G from UnitedHealthcare will be identical in coverage to the Plan G offered through Aetna.
What Do Medicare Supplement Plans Not Cover
Most Medicare Supplement plans have limits and exclusions to what they cover. For example, Plans C, D, F, G, and N cover 80% of medically necessary emergency care outside the U.S., but each of those four plans has other areas that they dont cover. Medicare.gov offers a detailed explanation of benefits for each plan.
Find A Secondary Health Insurance Quote With First Quote Health
If youre still wondering if a secondary health insurance plan is for you, its best to talk to a health insurance professional. Health insurance agents and brokers are a great tool and resource when it comes to shopping for a plan, or even just getting answers to your health insurance questions.
Aarp By United Healthcare
AARP is a special interest group that has served seniors since 1958. The company was founded with the goal of keeping aging Americans informed, empowered, and independent. Through various programs and services, it works to make the world more accessible and enjoyable for seniors across the country.
What is secondary health insurance?
A secondary insurance policy is a plan that you get on top of your main health insurance.
How does secondary insurance work?
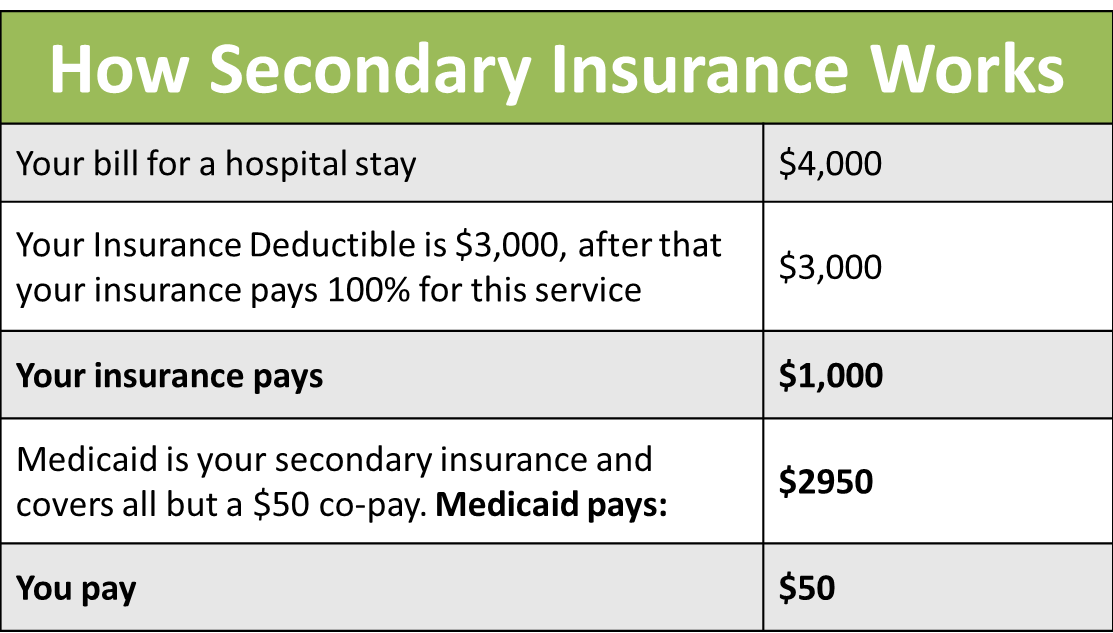
If you have multiple insurance policies, there is a clear order in which the plans will pay for health care services.
What types of coverage can you get?
The category of secondary health insurance includes multiple types of insurance plans. Some plans help with the costs of your primary insurance policy by addressing things such as high deductibles or the cost of a hospital stay.
What's the cost of secondary health insurance?
Secondary health insurance can cost anywhere from $5 per month to hundreds of dollars per month, depending on the type of coverage and the level of support the plan provides.
How do you choose the best secondary insurance plan?
Just as there are multiple considerations when choosing the best health insurance company, asking yourself the following questions can help you choose the best secondary health insurance policy.
Frequently asked questions
Secondary health insurance policies can fill in any coverage gaps, such as vision coverage, and available policies can also reduce the cost of health care services, such as hospital indemnity to help you cover the cost of hospital care.
What is the difference between primary and secondary insurance?
The insurance that pays first (primary payer) pays up to the limits of its coverage. The one that pays second (secondary payer) only pays if there are costs the primary insurer didn't cover. The secondary payer (which may be Medicare) may not pay all the uncovered costs.
How does Medicare work with other insurance?
When there's more than one payer, "coordination of benefits" rules decide which one pays first. The "primary payer" pays what it owes on your bills first, and then sends the rest to the "secondary payer" (supplemental payer) ...
How long does it take for Medicare to pay a claim?
If the insurance company doesn't pay the claim promptly (usually within 120 days), your doctor or other provider may bill Medicare. Medicare may make a conditional payment to pay the bill, and then later recover any payments the primary payer should have made. If Medicare makes a. conditional payment.
How many employees does a spouse have to have to be on Medicare?
Your spouse’s employer must have 20 or more employees, unless the employer has less than 20 employees, but is part of a multi-employer plan or multiple employer plan. If the group health plan didn’t pay all of your bill, the doctor or health care provider should send the bill to Medicare for secondary payment.
When does Medicare pay for COBRA?
When you’re eligible for or entitled to Medicare due to End-Stage Renal Disease (ESRD), during a coordination period of up to 30 months, COBRA pays first. Medicare pays second, to the extent COBRA coverage overlaps the first 30 months of Medicare eligibility or entitlement based on ESRD.
What is the phone number for Medicare?
It may include the rules about who pays first. You can also call the Benefits Coordination & Recovery Center (BCRC) at 1-855-798-2627 (TTY: 1-855-797-2627).
What happens when there is more than one payer?
When there's more than one payer, "coordination of benefits" rules decide which one pays first. The "primary payer" pays what it owes on your bills first, and then sends the rest to the "secondary payer" (supplemental payer) to pay. In some rare cases, there may also be a third payer.
What is a Medicare Supplement Plan?
A Medicare Supplement Plan, also called a Medigap plan, is a plan sold by private companies, separate from Medicare. Medicare Supplement plans pay for the costs, or “gaps,” in coverage that are not paid for by Original Medicare. These can include prescriptions, doctor visits, vision and dental care, and more.
How long do you have to switch back to Medicare Advantage?
If you’re unhappy with your Advantage plan and switch back to a Medicare Original Plan (which you can do within 12 months of enrolling in the Medicare Advantage plan), you then become eligible for Medicare Supplement insurance.
Is Medicare Advantage the same as Medigap?
Both Medicare Advantage and Medigap plans are supplements to Original Medicare, but they are different. Medicare Advantage is an alternative Medicare plan. Medicare Advantage has a low or $0 monthly charge and covers most prescription medicine, though the choice of doctors and networks may be limited.
Do all Medicare Supplement plans have the same benefits?
No matter which insurance company offers a particular Medicare Supplement plan, all plans with the same letter cover the same basic benefits. For instance, all Plan C policies have the same basic benefits no matter which company sells the plan.
Does Cigna cover Part B?
Warning. As of Jan. 1, 2020, Medicare Supplement plans sold to new Medicare recipients aren't allowed to cover the Part B deductible. Because of this, Plans C and F are not available to people new to Medicare starting on Jan. 1, 2020. Medicare Supplement plans don't cover the costs ...
Does Medicare Supplement cover out of pocket costs?
As the cost of healthcare continues to increase, so do the out-of-pocket costs for services that are not covered by Original Medicare. Because it can be difficult to predict your exact health care needs and costs, Medicare Supplement plans are used to cover many of the services you may need.
Does Aetna offer Medicare Supplement?
Aetna stands out because it offers several Medicare Supplement plans, including Parts A, B, C, D, F, G, and N, with each plan’s information and coverage clearly laid out on the company website. Consumers are supplied with ample details to really understand the options before making a decision.
What does Medicare Part B cover?
Both plans also cover Medicare Part B coinsurances and copays, the first three pints of blood, Part A hospice care coinsurances or copays, skilled nursing facility care coinsurances, and the Part A deductible, but not at 100% like other plans. Plan K covers these benefits at 50% and Plan L covers them at 75%.
How long do you have to be on Medicare if you have a disability?
If you have a disability and you’re receiving disability benefits from the Social Security Administration, you’ll automatically be enrolled in Parts A and B of Medicare once you’ve been receiving benefits for 24 months.
What is a Medigap plan?
Also called Medigap because it covers “gaps” in costs after Medicare Parts A and B pay their share. Medigap Plans C and F, which cover the Medicare Part B deductible, are being discontinued in 2020. Sign up for Medigap during Open Enrollment to lock in the best premium for your plan. Our Approach.
What is covered by Plan A?
Plan A also covers 100% of coinsurances or copayments for hospice care services, 100% of Medicare Part B coinsurances or copayments for medical outpatient services, and 100% of the cost of the first three pints of blood you are administered during a procedure.
How much does Medicare pay for a doctor's visit?
Here’s an example with numbers: if the doctor’s visit had a Medicare-approved cost of $100, Medicare would pay $80, your Medigap would pay $15, and you would only have to pay $5.
How much is Medicare Part B deductible?
For 2019, the deductible for Medicare Part B is $185. After the deductible, you’ll pay 20% of most medical expenses.
What happens if you don't enroll in Medicare?
If you don’t enroll in Part A (inpatient hospital services) when you initially qualify, you may find yourself saddled with a 10% late enrollment penalty on your Part A premium. Says the Medicare website, “You'll have to pay the higher premium for twice the number of years you could have had Part A, but didn't sign up.”