Mail your payment to Medicare. Pay by check, money order, credit card, or debit card. Fill out the payment coupon at the bottom of your bill, and include it with your payment.
Full Answer
How do I receive Medicare and Medi-Cal?
If you have both Medicare and Medi-Cal, how you receive your benefits depends on the county you live in. For Medicare benefits, you may choose fee-for-service Original Medicare in all counties, or a Medicare Advantage (MA) plan, if available in your county.
How do I find the amount of my Medicare premium Bill?
Amount of your Medicare premium bill Account number: Medicare claim number without dashes. You can find this number on the red, white, and blue Medicare card. Biller name: CMS Medicare Insurance
What information do I need to bill for Medicare?
When billing for traditional Medicare (Parts A and B), billers will follow the same protocol as for private, third-party payers, and input patient information, NPI numbers, procedure codes, diagnosis codes, price, and Place of Service codes.
Do I need a manual form to bill Medicare?
If a biller has to use manual forms to bill Medicare, a few complications can arise. For instance, billing for Part A requires a UB-04 form (which is also known as a CMS-1450). Part B, on the other hand, requires a CMS-1500.
How do I bill Medicare services?
Contact your doctor or supplier, and ask them to file a claim. If they don't file a claim, call us at 1-800-MEDICARE (1-800-633-4227). TTY: 1-877-486-2048. Ask for the exact time limit for filing a Medicare claim for the service or supply you got.
Why am I getting a bill for Medicare Part B?
If you have Medicare Part B but you are not receiving Social Security or Railroad Retirement Board benefits yet, you will get a bill called a “Notice of Medicare Premium Payment Due” (CMS-500). You will need to make arrangements to pay this bill every month.
How is Medicare payment determined?
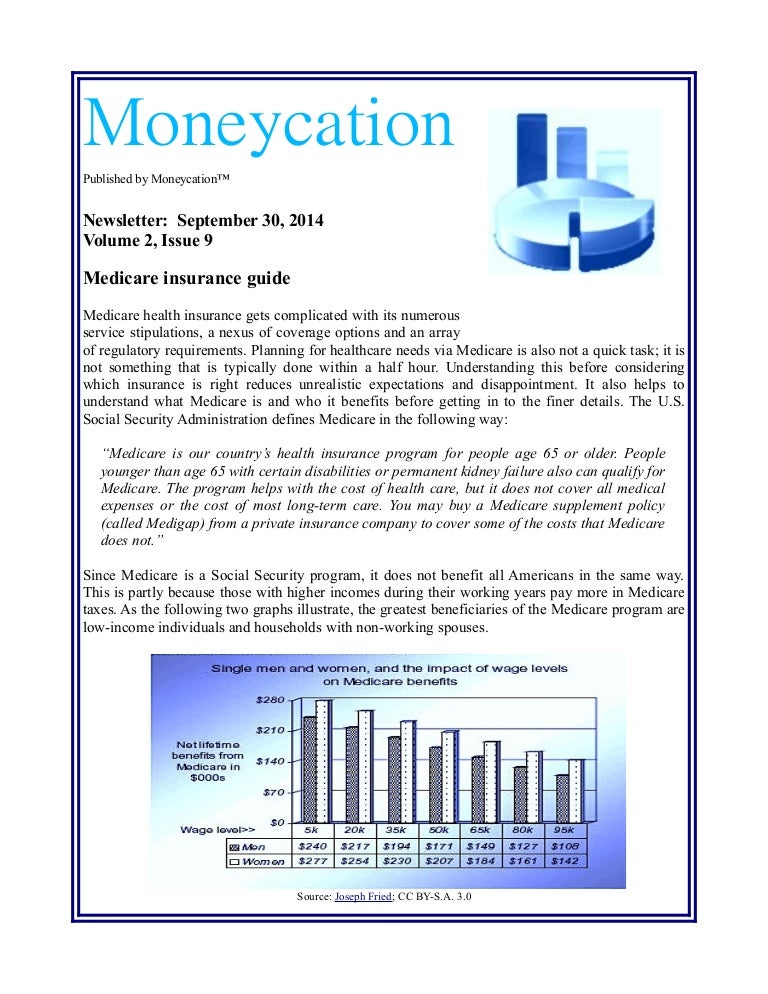
Medicare premiums are based on your modified adjusted gross income, or MAGI. That's your total adjusted gross income plus tax-exempt interest, as gleaned from the most recent tax data Social Security has from the IRS.
How much do you pay for Medicare in California?
Part B – Medical Insurance Premiums & DeductiblesFor 2022For 2021Annual Deductible$233$203Your Annual IncomeYour Monthly Premium*Your Monthly Premium*Single: up to $91,000 Couple: up to $182,000$170.10$148.50Single: $91,001 to $114,000 Couple: $182,001 to $228,000$238.10$207.903 more rows
Is Medicare Part B deducted from your Social Security check?
Medicare Part B (medical insurance) premiums are normally deducted from any Social Security or RRB benefits you receive. Your Part B premiums will be automatically deducted from your total benefit check in this case. You'll typically pay the standard Part B premium, which is $170.10 in 2022.
How often does Medicare bill for Part B?
Part B premiums You pay a premium each month for Part B. Your Part B premium will be automatically deducted from your benefit payment if you get benefits from one of these: Social Security. Railroad Retirement Board.
What income level affects Medicare premiums?
How much will I pay for premiums in 2022?Yearly income in 2020: singleYearly income in 2020: married, joint filing2022 Medicare Part B monthly premium> $114,000–$142,000> $228,000–$284,000$340.20> $142,000–$170,000> $284,000–$340,000$442.30> $170,000– < $500,000> $340,000– < $750,000$544.30≥ $500,000≥ $750,000$578.302 more rows•Nov 16, 2021
Why is my Medicare bill so high?
Medicare Part B covers doctor visits, and other outpatient services, such as lab tests and diagnostic screenings. CMS officials gave three reasons for the historically high premium increase: Rising prices to deliver health care to Medicare enrollees and increased use of the health care system.
Are Medicare premiums calculated every year?
The Part B premium is calculated every year. You may see a change in the amount of your Social Security checks or in the premium bills you receive from Medicare. Check the amount you're being charged and follow up with Medicare or the IRS if you have questions.
Does the state of California pay for Medicare?
The State of California participates in a buy-in agreement with the Centers for Medicare and Medicaid Services (CMS), whereby Medi-Cal automatically pays Medicare Part B premiums for all Medi-Cal beneficiaries who have Medicare Part B entitlement as reported by Social Security Administration (SSA).
Is Medicare different in California?
Medicare and Supplemental Coverage Eligibility If You Move Out of California. If you are enrolled in Original Medicare and you move out of California (or to a different service area within the state), your Medicare benefits will not change.
Do you have to pay Medicare premiums?
Most people don't pay a monthly premium for Part A (sometimes called "premium-free Part A"). If you buy Part A, you'll pay up to $499 each month in 2022. If you paid Medicare taxes for less than 30 quarters, the standard Part A premium is $499.
How to file a claim with Medicare?
Follow these steps: Fill out the claim form provided by your insurance company (if required). Attach copies of the bills you are submitting for payment (if required). Attach copies of the MSN related to those bills.
How does Medicare receive claims?
Your Medigap (supplemental insurance) company or retiree plan receives claims for your services 1 of 3 ways: Directly from Medicare through electronic claims processing. This is done online. Directly from your provider, if he/she accepts Medicare assignment. This is done online, by fax or through the mail.
How much does Medicare pay for Part B?
If the provider accepts assignment (agrees to accept Medicare’s approved amount as full reimbursement), Medicare pays the Part B claim directly to him/her for 80% of the approved amount. You are responsible for the remaining 20% (this is your coinsurance ). If the provider does not accept assignment, he/she is required to submit your claim ...
Is MSN a bill?
How much Medicare approved and paid. How much you owe. Previously known as the Explanation of Medicare Benefits, the MSN is not a bill. You should not send money to Medicare after receiving an MSN. Your provider will bill you separately.
Does Medicare send a bill for MSN?
For more information, see Assignment for Original Fee-for-Service Medicare . Medicare will send you a Medicare Summary Notice (MSN) form each quarter. Previously known as the Explanation of Medicare Benefits, the MSN is not a bill. You should not send money to Medicare after receiving an MSN.
How long do you have to enroll in Medicare after 65?
While the Special Enrollment Period is eight months, the window to enroll in a CalPERS Medicare health plan is only 30-60 days post-retirement, so immediate action is strongly encouraged.
How long do you have to work to get Medicare Part A?
Medicare Part A will be premium-free if you: Worked for at least 10 years (40 quarters) in Social Security/Medicare-covered employment; Are eligible through the work history of a current, former, or deceased spouse; and/or.
Does SSA pay Medicare Part B?
Medicare Part B. The SSA establishes a Medicare Part B premium amount annually, which must be paid to SSA to remain enrolled in Part B. If you receive SSA benefits, the Medicare Part B premium will be deducted from your SSA benefits; otherwise, the SSA will bill you quarterly.
Is Calpers Health Plan a primary payer?
If you enroll in Part A, your current CalPERS Health Plan will continue to be the primary payer of your insurance claims and Medicare Part A will be a secondary payer. As a secondary payer, Medicare pays up to their allowable amount of costs not covered by your CalPERS health insurance, potentially reducing your out-of-pocket costs.
Does Medicare Part A help with Calpers?
Therefore, remaining in a CalPERS health plan and enrolling in Medicare Part A will only help defray cost sharing for those covered services up to the allowable amount based on the Medicare fee schedule.
Do you need to send additional documentation to CalPers?
You will not need to send any additional documentation to us if: Your enrollment is more than 30 days from retirement, you may be required to provide supporting Medicare documentation (i.e., Medicare card or entitlement letter) to CalPERS.
Is Calpers a primary payer?
If you choose to enroll in a Medicare Part B while still actively working, you will remain in a CalPERS Basic (non-Medicare) health benefits plan and your CalPERS Employer Group Health Plan will be the primary payer, and Medicare becomes the secondary payer.
When do you need to update your Medicare premium?
You’ll need to tell the bank how much money to deduct from your account to pay for the Medicare premium. You’ll also need to update the amount with your bank whenever there is a change in the Medicare premium amount. This usually happens in January when CMS announces the new Medicare premium rates.
Does Medicare charge a fee for electronic payments?
This usually happens in January when CMS announces the new Medicare premium rates. You can find more information at Medicare.gov or CMS’s online bill pay webpage. Remember, CMS does not charge a fee for processing the electronic payments, but in some situations, a bank may charge their customers a fee for using their online bill payment service.
APPLYING FOR MEDICARE AND MEDI-CAL
Information about Medi-Cal, resources for applying and eligibility are provided by the Department of Health Care Services.
GENERAL INFORMATION
California Health Advocates offers Medicare advocacy, benefits information, and education for Californians.
FRAUD
The Bureau of Medi-Cal Fraud Elder Abuse explains how to report suspected Medi-Cal fraud or elder abuse to the Department of Justice.
What form do you need to bill Medicare?
If a biller has to use manual forms to bill Medicare, a few complications can arise. For instance, billing for Part A requires a UB-04 form (which is also known as a CMS-1450). Part B, on the other hand, requires a CMS-1500. For the most part, however, billers will enter the proper information into a software program and then use ...
What is a medical biller?
In general, the medical biller creates claims like they would for Part A or B of Medicare or for a private, third-party payer. The claim must contain the proper information about the place of service, the NPI, the procedures performed and the diagnoses listed. The claim must also, of course, list the price of the procedures.
What is 3.06 Medicare?
3.06: Medicare, Medicaid and Billing. Like billing to a private third-party payer, billers must send claims to Medicare and Medicaid. These claims are very similar to the claims you’d send to a private third-party payer, with a few notable exceptions.
How long does it take for Medicare to process a claim?
The MAC evaluates (or adjudicates) each claim sent to Medicare, and processes the claim. This process usually takes around 30 days .
Is it harder to bill for medicaid or Medicare?
Billing for Medicaid. Creating claims for Medicaid can be even more difficult than creating claims for Medicare. Because Medicaid varies state-by-state, so do its regulations and billing requirements. As such, the claim forms and formats the biller must use will change by state. It’s up to the biller to check with their state’s Medicaid program ...
Can you bill Medicare for a patient with Part C?
Because Part C is actually a private insurance plan paid for, in part, by the federal government, billers are not allowed to bill Medicare for services delivered to a patient who has Part C coverage. Only those providers who are licensed to bill for Part D may bill Medicare for vaccines or prescription drugs provided under Part D.
Do you have to go through a clearinghouse for Medicare and Medicaid?
Since these two government programs are high-volume payers, billers send claims directly to Medicare and Medicaid. That means billers do not need to go through a clearinghouse for these claims, and it also means that the onus for “clean” claims is on the biller.
What is Medi-Cal for Medicare?
Medi-Cal (for People with Medicare) Medi-Cal, the Medicaid program in California, provides health coverage to people with low-income and asset levels who meet certain eligibility requirements. While there are several ways to qualify for Medi-Cal, this section focuses only on Medi-Cal beneficiaries who also qualify for Medicare — individuals who are ...
How much does a person need to be to qualify for Medi-Cal?
To qualify for SSI, you must be age 65 or older, blind or disabled. Your countable monthly income may not exceed $954.72 for an individual or $1,598.14 for a couple (higher income levels apply for individuals who are blind).
What is Cal MediConnect?
Cal MediConnect is a demonstration program with the goal of integrating care for people with both Medicare and Medi-Cal. The demonstration is happening in 7 selected counties: Los Angeles, Orange, Riverside, San Bernardino, San Diego, San Mateo and Santa Clara, and began on various dates depending on the county.
What is Medicare Part D?
2. Prescription Drugs. If you are receiving both Medicare and Medi-Cal benefits, the Medicare Part D drug benefit will provide your prescription-drug coverage instead of Medi-Cal. You must be enrolled in a Medicare Part D drug plan or a Medicare Advantage prescription drug plan to get these benefits.
How much does Medi-Cal pay for SOC?
For example, if you have an individual monthly income of $1,300, Medi-Cal subtracts $600 for a SOC of $700 . This means you must pay at least $700 in covered medical expenses and/or health care premiums in a given month before Medi-Cal covers any of your health care costs for that month.
How much does Medi-Cal pay for medical expenses?
Your SOC is determined according to your monthly income, using the following formula: Medi-Cal subtracts $600 (for an individual) or $934 (for a couple) from your monthly income, and any other health-insurance premiums you may be paying.
Which MA plan works best for people with Medicare and Medi-Cal?
If you choose an MA plan, the MA plan that works best for people with both Medicare and Medi-Cal is the Special Needs Plan (SNP) for dual eligibles or D-SNP. If you’re enrolled in a D-SNP, you do not have copays, coinsurance or premiums associated with other types of MA plans.
How long does it take to change your Medicare billing?
To avoid having your Medicare billing privileges revoked, be sure to report the following changes within 30 days: a change in ownership. an adverse legal action. a change in practice location. You must report all other changes within 90 days. If you applied online, you can keep your information up to date in PECOS.
How to become a Medicare provider?
Become a Medicare Provider or Supplier 1 You’re a DMEPOS supplier. DMEPOS suppliers should follow the instructions on the Enroll as a DMEPOS Supplier page. 2 You’re an institutional provider. If you’re enrolling a hospital, critical care facility, skilled nursing facility, home health agency, hospice, or other similar institution, you should use the Medicare Enrollment Guide for Institutional Providers.
How to get an NPI?
If you already have an NPI, skip this step and proceed to Step 2. NPIs are issued through the National Plan & Provider Enumeration System (NPPES). You can apply for an NPI on the NPPES website.
Do you need to be accredited to participate in CMS surveys?
ii If your institution has obtained accreditation from a CMS-approved accreditation organization, you will not need to participate in State Survey Agency surveys. You must inform the State Survey Agency that your institution is accredited. Accreditation is voluntary; CMS doesn’t require it for Medicare enrollment.
Can you bill Medicare for your services?
You’re a health care provider who wants to bill Medicare for your services and also have the ability to order and certify. You don’t want to bill Medicare for your services, but you do want enroll in Medicare solely to order and certify.