Is Medicare Advantage regulated?
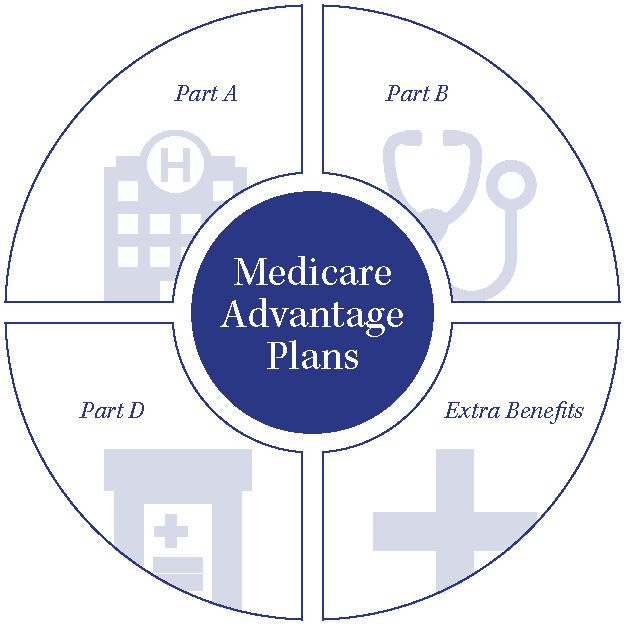
The private health plans are known as Medicare Advantage plans and are regulated and reimbursed by the federal government. MA plans combine Part A and Part B and oftentimes Part D, into one plan so your entire package of benefits comes from a private insurance company.
Who regulates California health insurance companies?
the California Department of Insurance (CDI)In California, health insurance is regulated by the California Department of Insurance (CDI). Our mission is to protect consumers, foster a vibrant and stable insurance marketplace, and enforce laws related to health insurance and the health insurance code fairly and impartially.
Who is Medicare regulated by?
The federal agency that oversees CMS, which administers programs for protecting the health of all Americans, including Medicare, the Marketplace, Medicaid, and the Children's Health Insurance Program (CHIP).
What is the Department of Managed Health Care Oversight?
Created in 2000, the California Department of Managed Health Care is a consumer protection agency that oversees the operations of managed care organizations. Its mission is to protect consumer healthcare rights and ensure “a stable health care delivery system.”
Who regulates third party administrators in California?
In California, regulation and oversight of fully insured employee health benefit plans is split between two state departments — the Department of Managed Health Care (DMHC) and the California Department of Insurance (CDI).
Who are insurance companies regulated by?
Insurance is regulated by the states. This system of regulation stems from the McCarran-Ferguson Act of 1945, which describes state regulation and taxation of the industry as being in “the public interest” and clearly gives it preeminence over federal law. Each state has its own set of statutes and rules.
What is the difference between the FDA and CMS?
Although FDA and CMS regulate different aspects of health care—FDA regulates the marketing and use of medical products, whereas CMS regulates reimbursement for healthcare products and services for two of the largest healthcare programs in the country (Medicare and Medicaid)—both agencies share a critical interest in ...
How is Medicare regulated?
The Social Security Administration (SSA) oversees Medicare eligibility and enrollment.
What level of government administers Medicare?
Medicare is a federal program. It is basically the same everywhere in the United States and is run by the Centers for Medicare & Medicaid Services, an agency of the federal government.
What does Department of Managed Healthcare do?
The Department of Managed Health Care (DMHC) is the primary government watchdog overseeing managed health care in California. It exists within the state's Business, Transportation and Housing Agency. The DMHC is charged with being an advocate for consumer rights and enforcing access to treatment.
What is the difference between health maintenance organizations and preferred provider organizations?
To start, HMO stands for Health Maintenance Organization, and the coverage restricts patients to a particular group of physicians called a network. PPO is short for Preferred Provider Organization and allows patients to choose any physician they wish, either inside or outside of their network.
What is Dhmc California?
Mission. The California Department of Managed Health Care protects consumers' health care rights and ensures a stable health care delivery system.
How many health insurance plans are there in California?
The DMHC regulates 121 California health insurance plans, including 72 full service plans and 49 specialized plans. They regulate all HMO plans in California and some PPO and EPO products as well as dental and vision plans.
What is DMHC in California?
The Department of Managed Health Care (DMHC) was established in 2000 through consumer sponsored legislation. It regulates the health care and medical insurance for 25 million Californians including the majority of those on Obamacare California plans insured through Covered California.
What is the mission of the DMHC?
The Mission: Protect Health Care Consumers. The mission of the DMHC is to “protect consumers’ health care rights and ensure a stable health care delivery system in California.”. The department is funded by assessments on health plans, so they are not dependent on the state legislature for income.
Does California regulate Medicare?
This government agency in California does not regulate California Department of Insurance (C DI) products, most Medicare coverage. They do not oversee some Medi-Cal coverage including fee-for-service and County Organized Health Systems (COHS).
How many Medicare Advantage Plans are there in California?
Medicare Advantage is an especially popular option in California, with the state reporting some of the highest enrollment rates in the nation. In 2019, there were 220 Medicare Advantage Plans available in California. 40% of the total Medicare population in California was enrolled in Medicare Advantage Plans as of 2018.
How many counties are there in California for Medicare Advantage?
Available Medicare Advantage Plans range from one to 90 across California’s 58 counties. Medicare-approved private health insurance companies administer Medicare Advantage Plans. Depending on your health care needs, this may be the more economical option. These plans usually cover more than Original Medicare and have annual out-of-pocket limits, ...
What is HICAP in Medicare?
HICAP provides a wide array of services to those who are eligible or will soon be eligible for Medicare. Through this statewide program, you can get information on how to sign up for a Medicare Advantage Plan, find out which plans are available in your region, and get answers to any questions you may have about your prescription drug coverage or cost-sharing responsibilities. It’s staffed with trained counselors who provide free one-on-one consultations regarding health insurance-related issues and Medicare and who can assist you with understanding your medical bills or resolving billing problems.
What is a PPO plan?
To get the most from your coverage and prevent denied claims, always follow the plan’s rules, such as getting prior approval for certain screenings and services. Preferred Provider Organizations (PPO) PPO plans are similar to HMOs in having network providers.
How old do you have to be to be eligible for Medicare Advantage?
To be eligible to join a Medicare Advantage Plan, you must be at least 65 years old or have a disability that qualifies you for Original Medicare Parts A and B. You must live within the service area of the plan you choose.
When is the open enrollment period for Medicare Advantage?
Medicare Advantage Open Enrollment Period: This period goes from January 1 to March 31 and is exclusively for those enrolled in Medicare Advantage. During this time, you can switch to another Medicare Advantage Plan or back to Original Medicare one time.
When is open enrollment for Medicare?
Open Enrollment Period: This period runs from October 15 to December 7. During this period, you can enroll in a Medicare Advantage plan or switch between plans, and any changes you make to your coverage will take effect on January 1. Medicare Advantage Open Enrollment Period: This period goes from January 1 to March 31 and is exclusively ...
What is Medicare Advantage?
Medicare is a national health insurance program for seniors or those with disabilities. Medicare Advantage is Medicare's managed care program. If you join Medicare Advantage, you get all your care through an HMO or PPO that has a contract with Medicare.
What is a Medi-Cal plan?
Medi-Cal is health care for people with low or no incomes. Some people who have Medi-Cal are in a Medi-Cal Managed Care plan. These plans have networks of providers, including doctors, pharmacies, clinics, labs, and hospitals. Medi-Cal covers the basic benefits that all health plans cover. Medi-Cal also covers prescription drugs, vision care, and hearing care.
What is a PPO plan?
A PPO is good plan for people who want to see providers without prior approval from their health plan or medical group and who do not want to choose a primary care doctor.
What is the MAP enrollment rate in California?
In California, 40% of all Medicare beneficiaries are currently enrolled in a MAP, which places California in a group of 21 other states with MAP enrollment rates between 31% and 40%. [5] . Of note, six states, plus Puerto Rico, have MAP enrollment rates greater than 40%. [6]
Does California have a MAP?
California has a high MAP enrollment rate. After a slow start, MAP enrollment has nearly doubled in the past decade. MAPs have become more popular for many reasons, including that MAPs often offer more benefits than traditional Medicare.
Can MAPs sue insurers for PCA damages?
While it is unknown where the Ninth Circuit (or other California courts) may ultimately fall on this issue, for now, the Central District of California is part of a growing number of jurisdictions finding that MAP s can sue insurers for PCA damage s under the MSP.
Can a MAP charge for medical services?
As MAP enrollment increases, questions are surfacing regarding the nature and extent of MAP recovery rights. Under specific MAP statutes and regulations, MAPs may “bill” or “charge” their enrollees or insurers for reimbursement of medical services they provide for claim-related treatment. [7] These provisions have been interpreted as permitting MAPs to establish contractual recovery rights as part of their underlying insurance agreements, but not creating an implied federal private cause of action right. [8]
SPOTLIGHT & RELEASES
09/15/2021 : CMS released the Second (Preliminary) Evaluation Report and associated Findings At-a-Glance for the California capitated model demonstration under the Medicare-Medicaid Financial Alignment Initiative
Cal MediConnect Model
On March 27, 2013, the Department of Health and Human Services announced that the State of California will partner with the Centers for Medicare & Medicaid Services (CMS) to test a new model for providing Medicare-Medicaid enrollees with a more coordinated, person-centered care experience, along with access to new services.
What is an HMO plan?
Health Maintenance Organization (HMO) plans have a defined network of contracted local physicians and hospitals to provide member care. Generally, members must use these care providers to receive benefits for covered services, except in emergencies. Some HMO plans do not need referrals for specialty care.
Do you need a referral for PPO?
Members do not need a referral for specialty care. PPO plans are available as either local PPO (certain counties within a state) or regional PPO (RPPO) offerings. RPPOs serve a larger geographic area - either a single state or a multi-state area.