You can still have other insurance, but once you apply for Medicare, it becomes your primary health insurance. Healthcare charges will be submitted to Medicare first, and any non-covered costs can then be submitted to your other plan. The bottom line
Should you stay on your employer health insurance or get Medicare?
By law, employer group health insurance plans must continue to cover you at any age so long as you continue working. Turning 65 would not force you to take Medicare so long as you're still working. The only exception is if your employer has fewer than 20 people (or fewer than 100 if you are disabled).
Do I need Medicare if I have insurance?
The vast majority of people receive Part A benefits without paying any premiums at all. Even if you are currently insured, you should go ahead and sign up for Medicare Part A. The standard premium for Medicare Part B, however, is $90.90 per month.
What other insurance do I need with Medicare?
What it means to pay primary/secondary
- The insurance that pays first (primary payer) pays up to the limits of its coverage.
- The one that pays second (secondary payer) only pays if there are costs the primary insurer didn't cover.
- The secondary payer (which may be Medicare) may not pay all the uncovered costs.
Can I have Medicare and private insurance at the same time?
It is possible to have both private insurance and Medicare at the same time. When you have both, a process called coordination of benefits determines which insurance provider pays first. This provider is called the primary payer. The primary payer pays for any covered services, until the coverage limit has been reached.
Can you have Medicare and employer insurance at the same time?
Yes, you can have both Medicare and employer-provided health insurance. In most cases, you will become eligible for Medicare coverage when you turn 65, even if you are still working and enrolled in your employer's health plan.
What insurance goes best with Medicare?
Best Medicare Advantage Providers RatingsProviderForbes Health RatingsCoverage areaHumana5.0Offers plans in all 50 states and Washington, D.C.Blue Cross Blue Shield5.0Offers plans in 48 statesCigna4.5Offers plans in 26 states and Washington, D.C.United Healthcare4.0Offers plans in all 50 states1 more row•Jun 8, 2022
Can I have dual coverage with Medicare?
If you qualify for both Medicare and Medicaid, you are considered "dual eligible." Sometimes the two programs can work together to cover most of your health care costs. Individuals who are dual eligible can often qualify for special kinds of Medicare plans.
Is Medicare primary or secondary insurance?
Medicare is always primary if it's your only form of coverage. When you introduce another form of coverage into the picture, there's predetermined coordination of benefits. The coordination of benefits will determine what form of coverage is primary and what form of coverage is secondary.
What will Medicare not pay for?
In general, Original Medicare does not cover: Long-term care (such as extended nursing home stays or custodial care) Hearing aids. Most vision care, notably eyeglasses and contacts. Most dental care, notably dentures.
Can I get Medicare Part B for free?
While Medicare Part A – which covers hospital care – is free for most enrollees, Part B – which covers doctor visits, diagnostics, and preventive care – charges participants a premium. Those premiums are a burden for many seniors, but here's how you can pay less for them.
What is the highest income to qualify for Medicaid?
Federal Poverty Level thresholds to qualify for Medicaid The Federal Poverty Level is determined by the size of a family for the lower 48 states and the District of Columbia. For example, in 2022 it is $13,590 for a single adult person, $27,750 for a family of four and $46,630 for a family of eight.
How do I qualify for dual Medicare and Medicaid?
Persons who are eligible for both Medicare and Medicaid are called “dual eligibles”, or sometimes, Medicare-Medicaid enrollees. To be considered dually eligible, persons must be enrolled in Medicare Part A (hospital insurance), and / or Medicare Part B (medical insurance).
Why do doctors not like Medicare Advantage plans?
If they don't say under budget, they end up losing money. Meaning, you may not receive the full extent of care. Thus, many doctors will likely tell you they do not like Medicare Advantage plans because private insurance companies make it difficult for them to get paid for their services.
Is Medicare Part B automatically deducted from Social Security?
Yes. In fact, if you are signed up for both Social Security and Medicare Part B — the portion of Medicare that provides standard health insurance — the Social Security Administration will automatically deduct the premium from your monthly benefit.
What happens if you don't have health insurance and you go to the hospital?
However, if you don't have health insurance, you will be billed for all medical services, which may include doctor fees, hospital and medical costs, and specialists' payments. Without an insurer to absorb some or even most of those costs, the bills can increase exponentially.
Does Medicare coverage start the month you turn 65?
The date your coverage starts depends on which month you sign up during your Initial Enrollment Period. Coverage always starts on the first of the month. If you qualify for Premium-free Part A: Your Part A coverage starts the month you turn 65.
What age do you have to be to be enrolled in Medicare?
are age 65 or over and enrolled in Medicare Part B. have a disability, end stage renal disease (ESRD), or amyotrophic lateral sclerosis (ALS) and are enrolled in both Medicare Part A and Part B. have Medicare and are a dependent of an active duty service member with TRICARE.
How does Medicare work with a group plan?
How Medicare works with your group plan’s coverage depends on your particular situation, such as: If you’re age 65 or older. In companies with 20 or more employees, your group health plan pays first. In companies with fewer than 20 employees, Medicare pays first. If you have a disability or ALS.
How to contact the SSA about Medicare?
Contacting the SSA at 800-772-1213 can help you get more information on Medicare eligibility and enrollment. State Health Insurance Assistance Program (SHIP). Each state has its own SHIP that can aid you with any specific questions you may have about Medicare. United States Department of Labor.
What is the process called when you have both insurance and a primary?
When you have both, a process called “coordination of benefits” determines which insurance provider pays first. This provider is called the primary payer. Once the payment order is determined, coverage works like this: The primary payer pays for any covered services until the coverage limit has been reached.
What is health insurance?
Health insurance covers much of the cost of the various medical expenses you’ll have during your life. Generally speaking, there are two basic types of health insurance: Private. These health insurance plans are offered by private companies.
What percentage of Americans have private health insurance?
Others include Medicaid and Veteran’s Affairs benefits. According to a 2020 report from the U.S. Census Bureau, 68 percent of Americans have some form of private health insurance. Only 34.1 percent have public health insurance, including 18.1 percent who are enrolled in Medicare. In certain cases, you can use private health insurance ...
Does Medicare pay first or second for ESRD?
You have ESRD. COBRA pays first. Medicare may pay second, depending whether there’s overlap between your COBRA coverage and your first 30 months of Medicare eligibility based on having ESRD.
Medicare: How it Works
Medicare works with a range of other insurance providers to pay your medical bills. How payment is worked out will vary, depending on your health insurance plan. When you shift to Medicare at age 65, you have many choices on arranging your health insurance.
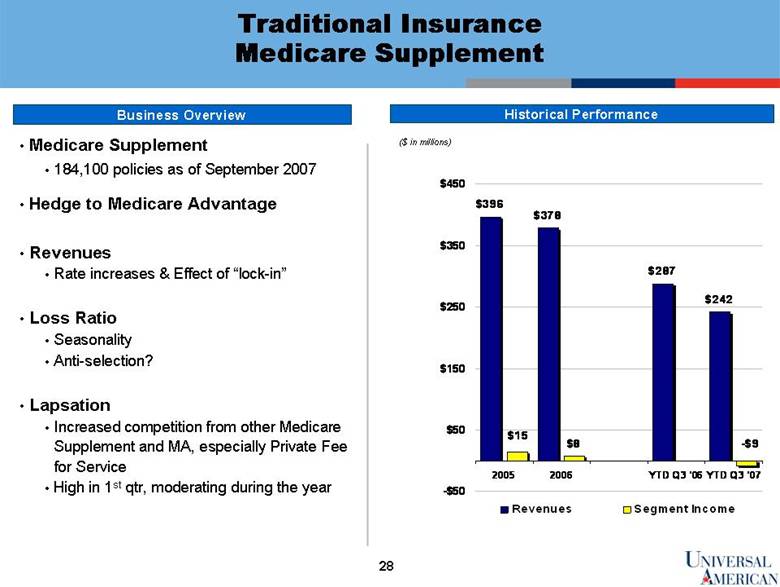
Medicare Part C
Medicare Part C, or a Medicare Advantage Plan, are bundled plans offered by private health insurance companies that meet all Medicare requirements.
Medicare Part D (Medicare Drug Plans)
Medications can be extremely expensive, so you should consider including a Medicare Drug Plan when you arrange your health insurance when you reach age 65. Sign up for this insurance in the first year, because if you do not, the price increases.
What if I am Still Employed?
If you are still employed and your employer has more than 20 employees, they are legally required to continue paying for your health insurance. You are required to take Medicare, but it is well worth reviewing your options at that time.
Navigating Medicare
If you are nearing age 65 and need help with Medicare, you can speak to one of our helpful agents. Navigating the system can be confusing and complicated, and once you make a choice, you must live with it until the next Medicare enrollment period. You want to arrange your health insurance so it works best for youth a reasonable cost.
How does Medicare work with other insurance?
When there's more than one payer, "coordination of benefits" rules decide which one pays first. The "primary payer" pays what it owes on your bills first, and then sends the rest to the "secondary payer" (supplemental payer) ...
Which insurance pays first, Medicare or No Fault?
No-fault insurance or liability insurance pays first and Medicare pays second.
What is a Medicare company?
The company that acts on behalf of Medicare to collect and manage information on other types of insurance or coverage that a person with Medicare may have, and determine whether the coverage pays before or after Medicare. This company also acts on behalf of Medicare to obtain repayment when Medicare makes a conditional payment, and the other payer is determined to be primary.
How long does it take for Medicare to pay a claim?
If the insurance company doesn't pay the claim promptly (usually within 120 days), your doctor or other provider may bill Medicare. Medicare may make a conditional payment to pay the bill, and then later recover any payments the primary payer should have made. If Medicare makes a. conditional payment.
What is the difference between primary and secondary insurance?
The insurance that pays first (primary payer) pays up to the limits of its coverage. The one that pays second (secondary payer) only pays if there are costs the primary insurer didn't cover. The secondary payer (which may be Medicare) may not pay all the uncovered costs.
How many employees does a spouse have to have to be on Medicare?
Your spouse’s employer must have 20 or more employees, unless the employer has less than 20 employees, but is part of a multi-employer plan or multiple employer plan. If the group health plan didn’t pay all of your bill, the doctor or health care provider should send the bill to Medicare for secondary payment.
Which pays first, Medicare or group health insurance?
If you have group health plan coverage through an employer who has 20 or more employees, the group health plan pays first, and Medicare pays second.
How long can you go without Medicare?
If 120 days go by without an insurance company paying a claim, your doctor may bill Medicare. Medicare may cover a bill on the condition it can recover any portion of the payment that the primary insurer ends up being responsible for.
What happens if your insurance isn't synced with Medicare?
You may be responsible for overpayments or penalties if your primary insurance isn’t synced with your Medicare correctly.
How to get Medicare Advantage?
There are also three major services that almost always aren’t covered by Original Medicare: hearing aids, dental work, and vision care. If you’re a Medicare beneficiary, you can: 1 Pay for these services out of your own pocket; 2 Enroll in separate vision, dental, or hearing insurance; or: 3 Join a Medicare Advantage plan that may cover all three of these services.
How many workers are eligible for Medicare?
Your employer coverage will be primary if. Your employer has 20 workers or more, and you’re over 65 years old and therefore qualify for Medicare; or: Your employer has 100 workers or more, and you qualify for Medicare due to a disability.
How many different Medicare Supplement plans are there?
Medicare Supplement plans (also known as “ Medigap ”): These are available in every state. There are 10 different types of plans, each with different levels of coverage to pay for your excess Medicare costs.
How many different types of Medicare Advantage Plans are there?
There are 10 different types of plans, each with different levels of coverage to pay for your excess Medicare costs. Medicare Advantage plans (also known as “Part C”): These are another option. They replace your Medicare Part A and Part B coverage.
What are the services that are not covered by Medicare?
There are also three major services that almost always aren’t covered by Original Medicare: hearing aids, dental work, and vision care. If you’re a Medicare beneficiary, you can: Pay for these services out of your own pocket; Enroll in separate vision, dental, or hearing insurance; or: Join a Medicare Advantage plan that may cover all three ...
How long before you turn 65 can you apply for Medicare?
A person does not have to be retired to apply for Medicare; instead you can apply online or at your local social security office, up to three months before turning 65. Or, once you apply for and begin receiving social security benefits, you will be automatically enrolled in Parts A and B.
What is Medicare for people 65 and older?
Medicare is the federal health insurance program for people who are 65 or older, certain younger people with disabilities, and people with permanent kidney failure. Medicare is compromised of four “parts” that cover a range of medical services:
What is the Medicare website?
The Medicare website has several helpful online tools, including a checklist to help you pick the level of Medicare you will need, or a quick finder to see if your service is covered .
Can you cancel a Medigap policy?
Medigap policies are sold by private agencies but are regulated by the government and must be guaranteed to be renewable; in other words, they cannot be cancelled if your health declines. They must also not duplicate your existing coverage.
Is Medigap the same as Medicare?
Medigap policies often exclude many of the same services as Medicare (see below), so it is important to carefully review what is and is not covered. You can purchase varying degrees of Medigap coverage based on what you are able and willing to pay for your monthly premium; for example, some Medigap policies will help pay for medical expenses you may incur when traveling outside of the U.S. You also have a right to cancel a policy within a certain amount of time (usually 30 days) if you are not happy with the policy.
Does Medicare cover dental care?
When planning your retirement, it’s important to remember that Medicare (and most Medigap) policies do not cover all services you may need in the future. Services excluded by Medicare are: Long-term care (also called custodial care) Most dental care. Eye examinations related to prescribing glasses.
Does Medicare require copays?
In addition, not everyone knows that Medicare requires that you meet deductibles (certain amounts of money spent before the insurance kicks in) as well as pay co-payments (money due when visiting a doctor). Also, not all health care services are covered by Medicare, so you may need to allot additional funds in your future budget to purchase supplemental private insurance.
Medicare As An Automatic
In some cases, Medicare is an automatic. For instance, Medicare.gov says that if you receive benefits via either Social Security or the Railroad Retirement Board (RRB) for more than four months before turning 65, you automatically receive Medicare Part A (hospital insurance) and Part B (medical insurance).
Choosing the Private Insurance Option
If none of these situations apply to you and you want to use private insurance instead, it’s important to understand that there is only a seven-month window in which you can apply for Medicare benefits, according to Medicare.gov.
Using Medicare With Other Insurances
You can also have both Medicare and private insurance to help cover your health care expenses. In situations where there are two insurances, one is deemed the “primary payer” and pays the claims first. The other becomes known as the “secondary payer” and only applies if there are expenses not covered by the primary policy.
What age does Medicare cover?
Medicare is the federal health insurance program that covers people age 65 and older as well as some younger people with disabilities or specific health conditions. If you’re still working at 65 and covered by your employer plan, several factors will affect your Medicare enrollment status:
What happens if you don't have employer based insurance?
If you don’t have employer-based insurance, or your employer has fewer than 20 employees, declining Medicare now means you’ll end up paying higher premiums each month when you do finally enroll:
What happens if you don't have creditable coverage?
The quality of your drug coverage: If your health insurance doesn’t include “ creditable drug coverage ,” as defined by Medicare, you’ll need to purchase a stand-alone drug plan that meets those standards. Going without this level of prescription drug coverage for more than a few months will cause Medicare to charge you a late enrollment penalty on top of your Part D premium after you sign up.
How much is Medicare Part B in 2021?
While Medicare Part A is free, Medicare Part B — which covers doctor visits and outpatient medical supplies — requires you to pay a monthly premium (in 2021, the premium is $148.50 per month for most enrollees; high earners may pay more). If you keep your existing insurance, you could end up paying premiums for two policies, which could get expensive.
How long can you delay Medicare enrollment?
As soon as one of those events occurs, you’ll enter Medicare’s 8-month special enrollment period .
How long does it take to sign up for Medicare?
As mentioned above, if you work for a company with fewer than 20 people, you’ll be expected to sign up for Medicare ( including Part D) as soon as your initial enrollment period rolls around. That period begins 3 months before your 65th birthday and continues for 3 months after the month you turn 65. You won’t be allowed to combine your Medicare plan with your existing job coverage.
Can you have two insurances?
Also, having two insurance policies can be confusing and possibly lead to billing complications . You and your doctor would have to keep track of which plan is primary and which is seconda ry .
How long do you have to sign up for Medicare?
In the year that you turn 65, you have seven months to sign up for Medicare Part A (if you have to pay for it) and Part B. You also have seven months to sign up for Part D unless you have other prescription drug coverage considered acceptable by Medicare (“creditable” prescription drug coverage). The initial enrollment period begins three months before you turn 65 and ends three months after, including the month of your birthday.
How long do you have to enroll in Medicare Advantage?
3 You have eight months from the time your employment ends or your coverage ends (whichever comes first) to enroll in Part B. 10 You have two months after the month your coverage ends to join Part D or a Medicare Advantage plan.
What is a Medigap plan?
Medigap Plans: These plans are supplemental insurance sold by private insurance companies that can help fill gaps in Medicare coverage like copays, coinsurance (the amount you may have to pay toward a claim), and any deductibles. You must have Parts A and B to buy a Medigap plan. 6
What happens if you miss your Medicare enrollment deadline?
If you miss your enrollment deadline, you may face penalties for signing up late— especially if you don’t have employer-provided coverage or drug coverage that Medicare considers comparable to its own.
What happens if you go without prescription coverage?
If you go without creditable prescription drug coverage for 63 consecutive days, you may owe a late enrollment penalty. The penalty is permanently added to your Part D premium. 12
How many parts does Medicare have?
Before diving into how Medicare works with your existing health coverage, it’s helpful to understand how it works on its own. Medicare has four main parts: A, B, C, and D. You can also purchase Medicare supplement insurance, known as Medigap.
Is it important to know when to apply for Medicare?
But it’s important to know when you need to apply for coverage—especially if you have other health insurance coverage—so you don’t get hit with costly penalties. Here’s how Medicare works, what to consider when you already have health insurance, and how to avoid penalties for late enrollment.
What is private insurance?
Private insurance is the predominant source of health coverage in the U.S. and is provided by private health insurance companies instead of a state or federal government. Private health insurance comprises two markets: group market and non-group market. The group market mainly focuses on employer-sponsored insurance plans, while the non-group, or individual, market includes plans that are purchased directly from an insurer. Individual plans can be purchased on and off health insurance exchanges. Individual plans purchased off the marketplace must cover 10 essential health benefits. 2
Does Medicaid have to be covered by the federal government?
Although the federal government sets the minimum standards for Medicaid, this program gives states a lot of flexibility to customize their programs, including whom to cover, the benefits to provide, and how health care services are delivered. While there are mandatory benefits states must cover, there’s also room to cover additional optional benefits.
Do you have to show your medicaid card to your doctor?
If you have both Medicaid and private health insurance, you should show both your private health insurance card and Medicaid card to your medical provider every time you receive services.
Does Medicaid pay for care?
Some Medicaid programs pay for care directly, while others use private insurance carriers to offer Medicaid coverage.
Is Medicaid a federal or state program?
At their most basic, Medicaid and private insurance offer health coverage, but their inner workings are different. Medicaid is a state and federally funded program that covers the cost of medical services for low-income parents, children, pregnant women, older adults, those living with disabilities, and women with cervical or breast cancer. These individuals must meet the qualifying income requirements and satisfy other eligibility requirements.
Is Medicaid cheaper than private insurance?
In fact, it’s cheaper to cover adults of similar health status through Medicaid than private insurance.
Does Medicaid cover out of pocket expenses?
Private health insurance policies usually have copay and deductible requirements. If you qualify for both Medicaid and private insurance, Medicaid may cover these out-of-pocket expenses for you.