While you generally don’t have to change your Medicare Supplement insurance coverage when you move, you may decide you want to. Also, in some cases it may be necessary. Although most states offer the same 10 Medicare Supplement insurance plans, the specific plans available in your location may vary, since insurance companies aren’t required to sell every plan.
Full Answer
Can I Keep my Medicare supplement plan if I move?
Feb 02, 2022 · When you switch Medicare Supplement Insurance plans, you generally are allowed 30 days to decide to keep it or not. This 30-day “free look” period starts when your new Medicare Supplement plan takes effect. To qualify, you need to pay the premiums for both your new plan and your old plan for one month.
Do I need to switch Medicare if I move to Minnesota?
Oct 03, 2019 · If you notify your plan after you move, you can switch plans the month you provided notice of the move and up to two months after that. You can switch to a new Medicare Advantage plan or Medicare Prescription Drug Plan during this period of moving to a different service area. If you prefer, you can return to Original Medicare.
What if I decide to change to a new Medicare supplement insurance plan?
As of January 1, 2020, Medigap plans sold to people new to Medicare can no longer cover the Part B deductible. Because of this, Plans C and F are no longer available to people new to Medicare on or after January 1, 2020.
How do I switch to a new Medicare Advantage plan?
Aug 25, 2016 · Changing Medicare Supplement (Medigap) Plans The best time for you to sign up for a Medicare Supplement plan, also called Medigap, is when you turn 65 and are covered under Medicare Part B. This six-month period, known as your Medigap Open Enrollment Period, typically starts on your 65th birthday if you’re already enrolled in Part B.
Can I keep my Medicare supplement if I move?
Can I change my Medicare supplemental plan anytime?
What happens to Medigap when you move?
How long do I have to change my Medicare plan after I move?
What states allow you to change Medicare supplement plans without underwriting?
Can I change Medicare supplement plans without underwriting?
Do I need to notify Medicare if I move?
Why do doctors not like Medicare Advantage plans?
Can I switch from Plan F to Plan G without underwriting?
When can I change Medicare Part D?
What qualifies as a life changing event for Medicare?
Can I switch back to Original Medicare?
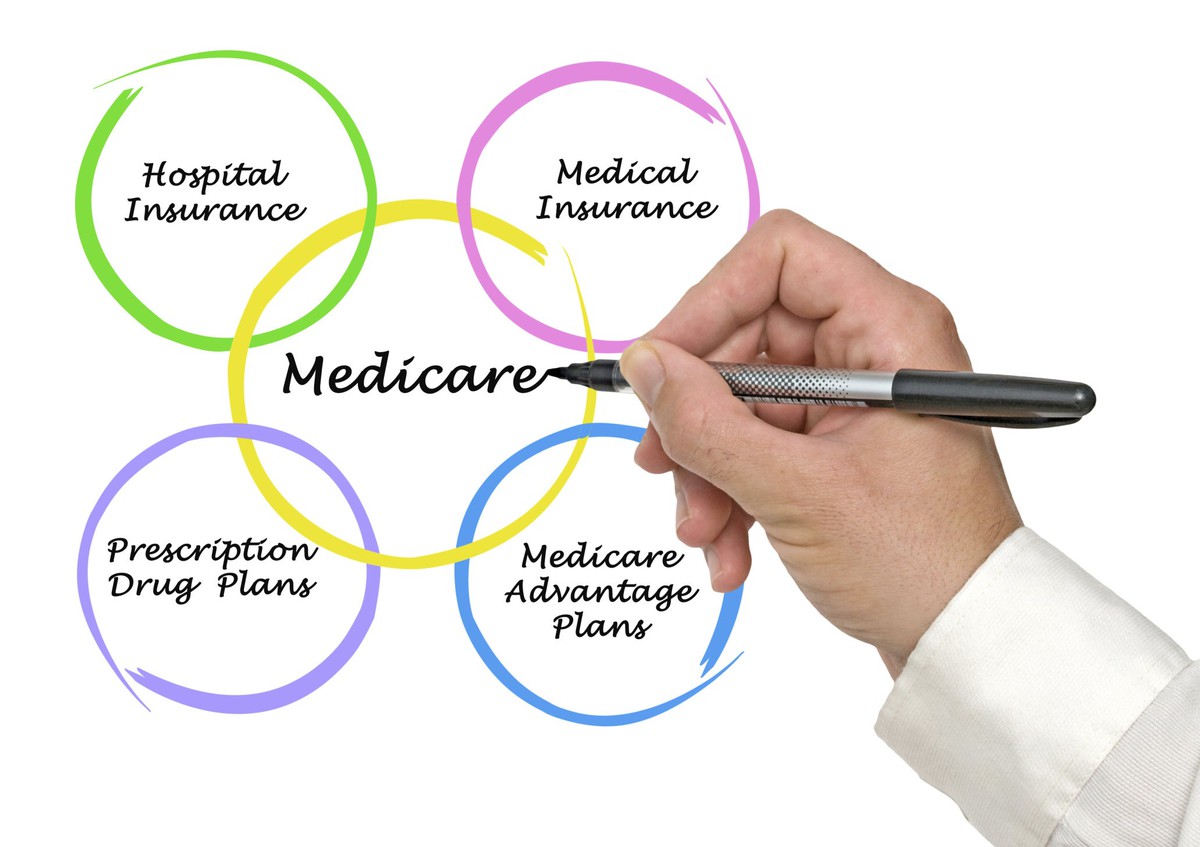
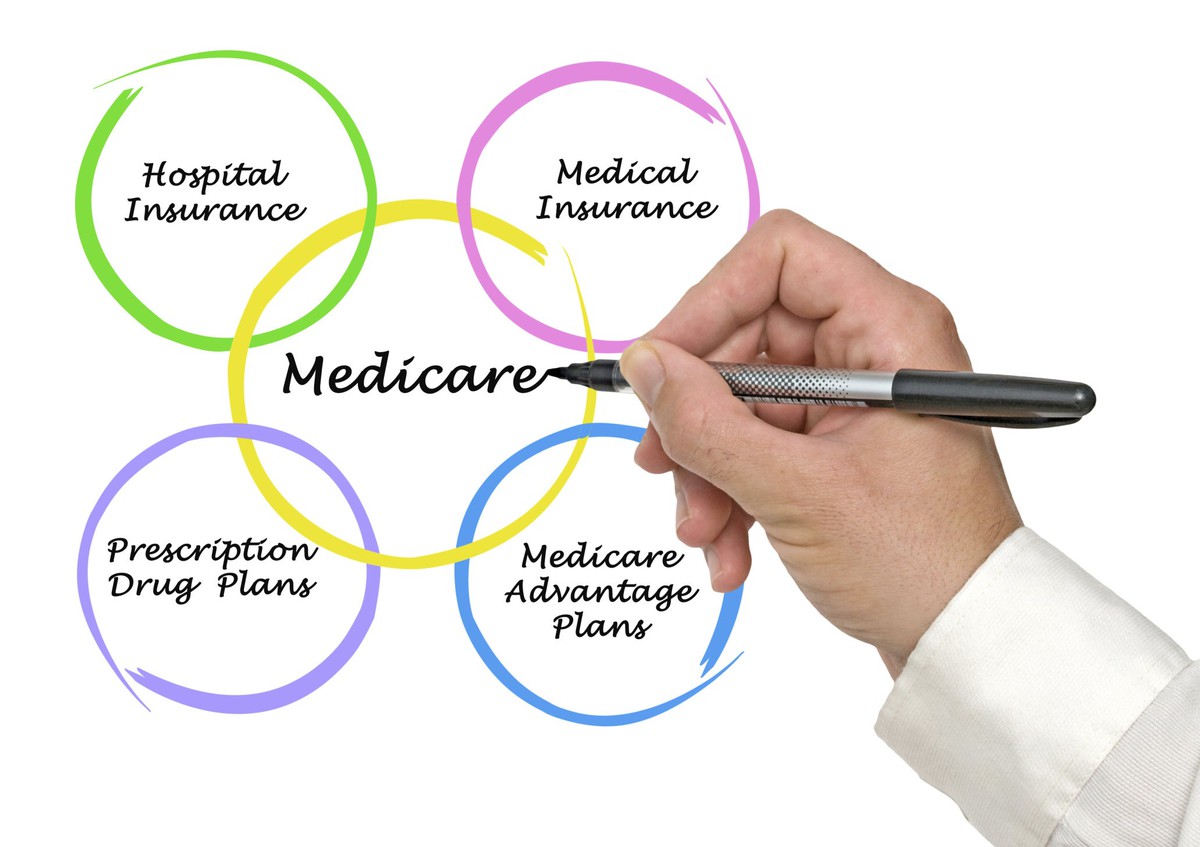
What Type of Medicare Coverage Do You have?
If you reside within the United States (including the District of Columbia, the U.S. Virgin Islands, Puerto Rico, Guam, and the Northern Mariana Is...
Do You Have A Medicare Supplement Plan? Here’S How to Handle Your Move to Another State.
If you’re enrolled in a Medicare Supplement plan (also known as Medigap) and move to another state, you may be able to keep the same policy. There...
Have You Notified Social Security About Your Address Change?
Make sure you notify Social Security of your change of address. The Social Security Administration handles Medicare enrollment. If you receive Soci...
Your Current Medigap Plan Provides More Coverage Than Necessary
Are you paying for benefits that you don’t need and never use? Perhaps you’re in good health and don’t use all of your Medigap benefits. A cheaper...
Out-Of-Pocket Costs Are Too High
Let’s say you’re in poor health, and there’s another Medigap plan that will help you save more money. Switching Medicare Supplement plans may be di...
Someone You Know Is Paying Less Than You Are For The Same Medigap Plan
Medicare Supplement plans are named with letters, such as Plan A, and standardized such that plans of the same letter name offer the same benefits....
You Have A Medicare Advantage Plan and Switch to Original Medicare With Medigap
Medigap and Medicare Advantage (Medicare Part C) plans don’t work together. If you drop your Medicare Advantage plan, and return to Original Medica...
You Have An Older Medigap Policy That’S No Longer Sold
You may wish to reconsider switching plans if this is your sole reason for changing plans. You don’t have to change plans just because the one you...
Other Points to Keep in Mind When Switching Medigap Plans
1. If you decide to change Medigap plans, you have a 30-day “free look” period where you can temporarily carry both plans to see which one you like...
What is a SEP in Medicare?
If you’re enrolled in a Medicare Advantage plan or a Medicare Part D Prescription Drug Plan, a change in residence, such as moving to another state, could qualify you for a Special Election Period (SEP). During your SEP, you’re allowed to enroll into a new plan that is offered in your new service area.
What happens if you don't enroll in Medicare Advantage?
If your current Medicare Advantage plan is not offered in your new service area, your Medicare Advantage plan is required by Medicare to disenroll you. If you don’t enroll in a new Medicare Advantage plan during your SEP, you’ll return to Original Medicare (Part A and Part B).
When do you have to sign up for Medicare Advantage after moving?
If you’d like to sign up for a new Medicare Advantage plan after you moved and your relocation-based SEP is over, you generally have to wait for the Annual Election Period (October 15 – December 7) .
Can you see a doctor on Medicare Supplement?
Most Medicare Supplement plans let you see any doctor who accepts Medicare assignment, but one type of Medigap plan – called Medicare SELECT – may require you to use providers within its network. If you have a Medicare SELECT policy and you move out of the plan’s service area:
How long do you have to have a select policy to get Medicare?
You won’t have to undergo medical underwriting if you’ve had your Medicare SELECT policy for more than six months. Otherwise, the insurance company may review your health history and may charge you more (or choose not to sell you a policy) if you have a health condition.
How long does a SEP last?
If you notify the plan before you move, your SEP timeframe is four months long. It begins one month before the month you move and lasts for three more months after that. If you notify your plan after you move, you can switch plans the month you provided notice of the move and up to two months after that.
How many states have Medigap?
There are 10 standardized Medigap plans available in 47 states (Minnesota, Massachusetts, and Wisconsin have their own standardized plans). Because the plans are standardized in most states, you may be able to remain with the same plan.
How to switch Medigap insurance?
How to switch Medigap policies. Call the new insurance company and arrange to apply for your new Medigap policy. If your application is accepted, call your current insurance company, and ask for your coverage to end. The insurance company can tell you how to submit a request to end your coverage.
How long can you have a select Medicare policy?
If you've had your Medicare SELECT policy for more than 6 months, you won't have to answer any medical questions. Use your guaranteed issue right to buy any Medigap Plan A, B, C, F, K, or L that's sold in most states by any insurance company.
Does Medicare cover Part B?
As of January 1, 2020, Medigap plans sold to new people with Medicare aren't allowed to cover the Part B deductible. Because of this, Plans C and F are not available to people new to Medicare starting on January 1, 2020.
What happens if you buy a Medigap policy before 2010?
If you bought your policy before 2010, it may offer coverage that isn't available in a newer policy. If you bought your policy before 1992, your policy: Might not be a Guaranteed renewable policy. May have a bigger Premium increase than newer, standardized Medigap policies currently being sold. expand.
Can you exclude pre-existing conditions from a new insurance policy?
The new insurance company can't exclude your Pre-existing condition. If you've had your Medigap policy less than 6 months: The number of months you've had your current Medigap policy must be subtracted from the time you must wait before your new Medigap policy covers your pre-existing condition.
How long do you have to pay for Medigap?
You have 30 days to decide if you want to keep the new Medigap policy. This is called your "free look period." The 30-day free look period starts when you get your new Medigap policy. You'll need to pay both premiums for one month.
How long is the free look period for Medigap?
Medigap free-look period. You have 30 days to decide if you want to keep the new Medigap policy. This is called your "free look period.". The 30- day free look period starts when you get your new Medigap policy. You'll need to pay both premiums for one month.
When to sign up for Medicare Supplement Plan?
The best time for you to sign up for a Medicare Supplement plan, also called Medigap, is when you turn 65 and are covered under Medicare Part B. This six-month period, known as your Medigap Open Enrollment Period, typically starts on your 65th birthday if you’re already enrolled in Part B. During this period, you’re guaranteed acceptance into any Medicare Supplement plan available in your area without submitting to a complete medical review or being denied coverage because of pre-existing conditions. If you choose not to get Medicare Part B right away, then your Medigap Open Enrollment Period may also be delayed and will start automatically once you’re at least 65 and have Part B.
When is the best time to sign up for Medicare Supplement?
The best time for you to sign up for a Medicare Supplement plan, also called Medigap, is when you turn 65 and are covered under Medicare Part B. This six-month period, known as your Medigap Open Enrollment Period, typically starts on your 65th birthday if you’re already enrolled in Part B. During this period, you’re guaranteed acceptance ...
Can you switch Medicare plans with guaranteed issue?
You may still be able to switch plans with guaranteed issue in certain situations . For example, if your Medigap company goes bankrupt or misled you, you may be able to change Medicare Supplement policies with guaranteed issue. But some states have laws that make sure certain Medigap policies are always available.
Can you change your Medicare Supplement if it goes bankrupt?
For example, if your Medigap company goes bankrupt or misled you, you may be able to change Medicare Supplement policies with guaranteed issue. But some states have laws that make sure certain Medigap policies are always available. Check your state’s insurance website to see what’s available in your area.
How many Medigap plans are there?
In most states, there are 10 Medigap plans — Plan A through Plan N (some plans, such as Plan E, are no longer sold).
How many states have Medigap?
In most states, there are 10 Medigap plans — Plan A through Plan N (some plans, such as Plan E, are no longer sold). Massachusetts, Minnesota, and Wisconsin have their own versions of Medigap.
How does Medigap set premiums?
Medigap insurers can set premiums in any of these ways: Attained-age rated –The premium is based on your current age and increases with your age. Entry-age-rated – The premium is set using your age when you first enroll. No-age rated – The premium is the same for everyone who has the same policy.
How does Medicare Supplement work?
How Your Medicare Supplement (Medigap) Insurance Plan Works If You’re Moving Out of State . If you’re enrolled in a Medicare Supplement (Medigap) insurance plan and moving out of state, you may be wondering if you need to take action to keep your current coverage. Medicare Supplement insurance plans help with certain out-of-pocket costs ...
Does Medicare Supplement cover out of pocket costs?
Medicare Supplement insurance plans help with certain out-of-pocket costs that Original Medicare doesn’t cover, and most states offer the same 10 standardized plans (Massachusetts, Wisconsin, and Minnesota have different plans available). However, because Medicare Supplement insurance plans can be used with any provider ...
Do you have to sell every Medicare Supplement plan?
Although most states offer the same 10 Medicare Supplement insurance plans, the specific plans available in your location may vary, since insurance companies aren’t required to sell every plan. If you’re moving to a different state, you may have other Medicare Supplement insurance plans available in your new location that weren’t offered previously.
How long before Medicare coverage ends can you move?
You can do so as early as 60 days before your coverage ends, or no later than 63 days after your coverage ends. Make sure to contact your Medicare SELECT company before you move to avoid a lapse in coverage. If you have any questions about how moving may affect your current Medicare Supplement insurance coverage, ...
What is a select plan?
Medicare SELECT plans are a type of Medicare Supplement insurance plan that requires you to use providers in the plan’s network to be covered. If you have a Medicare SELECT plan and move out of the plan’s service area, you have a guaranteed-issue right to buy any Medicare Supplement insurance Plan A, B, C, F, K, ...
How to switch to Medicare Advantage?
To switch to a new Medicare Advantage Plan, simply join the plan you choose during one of the enrollment periods. You'll be disenrolled automatically from your old plan when your new plan's coverage begins. To switch to Original Medicare, contact your current plan, or call us at 1-800-MEDICARE. Unless you have other drug coverage, you should ...
What happens if you lose Medicare coverage?
In other cases, you may still be able to use your employer or union coverage along with the Medicare Advantage plan you join.
What is Medicare Made Clear?
Medicare Made Clear is brought to you by UnitedHealthcare to help make understanding Medicare easier. Click here to take advantage of more helpful tools and resources from Medicare Made Clear including downloadable worksheets and guides.
Can you qualify for special enrollment period if you are moving?
Maybe you got a new job, or you’re retiring, or you wish to be closer to your family. No matter why, if you’re moving and have Medicare coverage, you may qualify for a unique Special Enrollment Period when you can make some changes.
What happens if you move to a new city?
If you move to a new city that is outside of your plan’s network, you will lose your Medicare Advantage or Part D plan. In this case, if you have a Medicare Advantage plan, you either have to enroll in a new plan or opt to return to Original Medicare and also enroll in a Part D plan. In this situation you have the following options:
What is dual eligible special needs?
And, if you are interested in a dual eligible special needs plan, which is a plan that combines the benefits of Medicare and Medicaid, as well as often including additional benefits such as dental or vision care. You’ll need to contact the private plan provider for information and availability of dual plans.
What is a special enrollment period?
Enrolling During A Special Enrollment Period. When you move, or experience another type of qualifying life event, you will get a two-month Special Enrollment Period (SEP)1. This kind of Special Enrollment Period allows you to join, change or drop a Medicare Advantage or Part D prescription drug plan. Open video transcript.
What is a SEP period?
When you move, or experience another type of qualifying life event, you will get a two-month Special Enrollment Period (SEP)1. This kind of Special Enrollment Period allows you to join, change or drop a Medicare Advantage or Part D prescription drug plan.
How long does a SEP last?
If you notify your plan provider before you move, your SEP begins the month before you move and lasts up to two full months after you move.
Can I keep my Medicare coverage in a new location?
In this unpredictable world, one thing is for certain: life happens. No matter what age you are, there is always some possibility that you will want to relocate. Perhaps you want to be closer to family as you age, or you’d just prefer a more accommodating climate.
When can you switch Medicare Advantage plans?
Due to its status as a government-regulated health insurance program, there are specific times throughout the calendar year during which you can make changes to your existing Medicare coverage or enroll in a new plan.
How can I get the Medicare Advantage coverage I need in my new area of residence?
The first step in making changes to your Medicare Advantage plan as a result of a move is to determine what plan options will be available to you in your new area of residence.
Do you need to change your Medicare plan when you move?
Generally speaking, if your plan requires that you use a set network for healthcare service providers, you will need to make more changes when you move . Because having continuous healthcare coverage is so important, you should have all the facts about how your Medicare benefits are affected by your move before you start packing.
Does Medicare require you to change your insurance?
Is Medicare coverage affected when you move to a different state? If you are enrolled in Original Medicare Part A (hospital insurance) and/or Part B (medical insurance), you do not need to make changes to your coverage. This is true if you move to a new state, or to a new area within the same state. Medicare does not require you to use healthcare ...
Does Medicare require you to use a hospital?
Medicare does not require you to use healthcare providers or hospitals in networks, as is the case with some Medicare Advantage plans. Once you have moved, you can choose any physician, hospital, or other healthcare provider as long as they accept Medicare assignment. Using healthcare providers who accept Medicare assignment ensures ...
Does moving affect Medicare?
Does moving affect your Medicare Advantage or Medicare Prescription Drug Plan? If you have a Medicare Advantage (Part C) or Prescription Drug (Part D) Plan, your coverage is likely restricted to a specific service area. If you are moving outside your current plan’s area, you must enroll in a new plan which includes the area where your new home is.
What is a SEP in Medicare?
You can take advantage of a Special Enrollment Period (SEP) to make changes to a Part C or D plan. SEPs are available for Medicare recipients who experience certain life events. If you are moving outside your plan’s area of service and need a new plan, or if you are moving within the plan’s area of service and wish to include new plan options ...
How to enroll in Medicare Supplement Plan?
1. Enroll in a Medicare Supplement Plan through your current Medigap provider if it covers the same, or fewer benefits than your current SELECT plan. 2. Enroll in a Medigap plan offered by any provider in your new area of service. Also, if you have a Medicare Advantage plan in your current state but there are no available Part C plans in the state ...
How long does a SEP last?
If you notify your provider before you move, your SEP begins the month before you move and continues for two months after the move. If you wait until after you move to notify your provider, your SEP begins the month of notification and ends after two months have passed. If you have a Medicare Advantage plan before you move ...
What is Medicare Supplement?
Having a Medicare Supplement health insurance plan, also known as Medigap, means having added financial assistance to pay for out of pocket expenses that may occur with Original Medicare benefits.
How long does it take to change Medicare Supplement?
If accepted into a new plan, you have a free look period which lasts 30 days. During this 30-day period, you can decide which plan you prefer.
Can you use Medigap Supplement with Original Medicare?
However, if you are not covered by guaranteed issue rights, you may have to go through medical examination, and you may not be accepted by the issuers of the policy. All Medigap Supplement insurance plans can be used with any health care provider that accepts Original Medicare assignment.
