Is COBRA primary over Medicare?
This is true even if your Part A benefits begin before you elect COBRA but you don’t sign up for Part B until later. In this situation, Medicare is always primary to COBRA coverage. If you become entitled to Medicare after you’ve signed up for COBRA, your COBRA benefits cease.
How does Cobra work with Medicare?
The parts of Medicare are:
- Medicare Part A (hospital insurance). Part A covers stays in the hospital, skilled nursing facilities, and other inpatient care settings.
- Medicare Part B (medical insurance). Part B covers doctor’s visits, ambulance rides, medical equipment, therapies, and other medical services.
- Medicare Part C (Medicare Advantage). ...
- Medicare Part D (drug coverage). ...
Is Cobra credible for Medicare?
Under current law, COBRA coverage does not count towards creditable prior coverage for Medicare Part B, which means that when your COBRA ends and you decide to sign up for Medicare Part B after the date you originally could have joined, you will face a 10% per year for life penalty on the cost of Part B.
Which is primary cobra or Medicare?
Please leave this field empty. In most cases, Medicare is primary and COBRA is secondary. But there are situations where your COBRA plan would be primary. If you are on Medicare as a result of ESRD (end stage renal disease) the role is reversed and COBRA is primary, Medicare secondary.
Is Medicare primary or secondary to COBRA?
If you have Medicare Part A or Part B when you become eligible for COBRA, you must be allowed to enroll in COBRA. Medicare is your primary insurance, and COBRA is secondary. You should keep Medicare because it is responsible for paying the majority of your health care costs.
Does Medicare pay primary to COBRA?
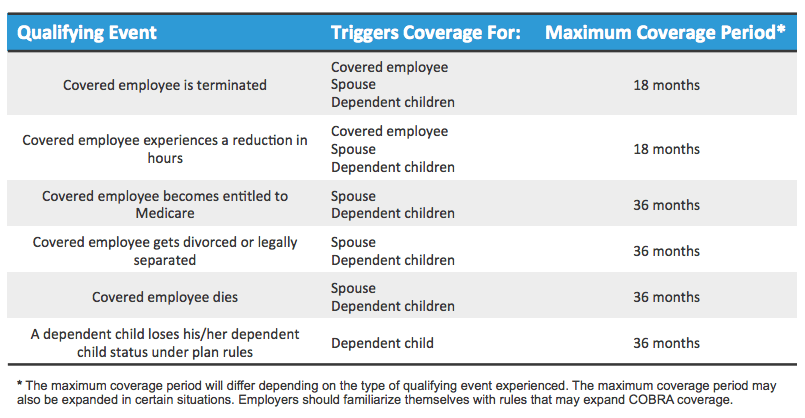
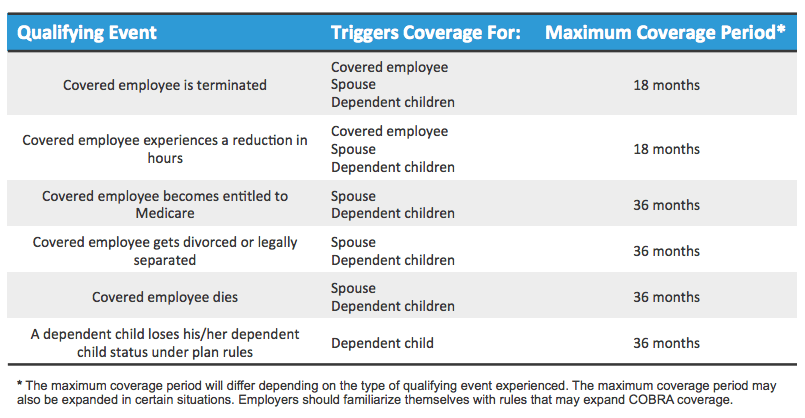
In this situation, Medicare is always primary to COBRA coverage. If you become entitled to Medicare after you've signed up for COBRA, your COBRA benefits cease. (But if COBRA covers your spouse and/or dependent children, their coverage may be extended for up to 36 months because you qualified for Medicare.)
Does COBRA end when Medicare begins?
If you have COBRA before signing up for Medicare, your COBRA will probably end once you sign up. You have 8 months to sign up for Part B without a penalty, whether or not you choose COBRA. If you miss this period, you'll have to wait until January 1 - March 31 to sign up, and your coverage will start July 1.
Can a person have COBRA and Medicare at the same time?
If you have Medicare first and then become eligible for COBRA, you can have both Medicare and COBRA. It is important to remember that Medicare pays first and COBRA pays second.
What does Medicare Part A pay for?
Part A covers inpatient hospital stays, care in a skilled nursing facility, hospice care, and some home health care. coverage if you or your spouse paid Medicare taxes for a certain amount of time while working. This is sometimes called "premium-free Part A." Most people get premium-free Part A.
What happens if I turn 65 while on COBRA?
The risks in electing COBRA at 65 or older include missing Medicare Part B enrollment deadlines and paying premium penalties, having a gap in medical coverage and being responsible for large medical bills you didn't anticipate.
Is Medicare entitlement A COBRA qualifying event?
Medicare entitlement of the employee is listed as a COBRA qualifying event; however, it is rarely a qualifying event. In situations where it is a qualifying event, it is only a qualifying event for the spouse or children that are covered under the group health plan.
Does Medicare coverage start the month you turn 65?
The date your coverage starts depends on which month you sign up during your Initial Enrollment Period. Coverage always starts on the first of the month. If you qualify for Premium-free Part A: Your Part A coverage starts the month you turn 65.
Can my spouse go on COBRA If I go on Medicare?
But if your spouse became eligible for Medicare and then left his or her employment (and thus lost access to employer-sponsored coverage) within 18 months of becoming eligible for Medicare, you can continue your spousal coverage with COBRA for up to 36 months from the date your spouse became eligible for COBRA.
Is COBRA creditable coverage for Medicare Part B?
Is COBRA creditable coverage for Medicare Part B? COBRA is NOT creditable coverage for Part B. If you delay enrollment, you'll face lifetime penalties.
How does COBRA work when you retire?
Under COBRA, a retired employee can receive the same health insurance coverage for up to 18 months. But you must pay the entire premium - part of which your employer probably previously covered. In some cases, people who opt to use COBRA also have to pay an extra 2% to cover administrative fees associated with it.
Why is COBRA not creditable coverage?
COBRA is not normally considered to be creditable coverage for Medicare major medical benefits, so people who are enrolled in COBRA and do not enroll in Medicare Part B within 8 months of turning 65 face substantial financial penalties for the rest of their lives, even if they have months or years left on their COBRA ...
How long do you have to take Cobra after leaving a job?
Once you leave your job, you have at least 60 days to decide whether to take COBRA coverage. If you’re not already enrolled in Medicare Part B, you’ll have 8 months after leaving your job to enroll. You can use this window of time to weigh your options.
How long can you keep Cobra insurance?
Under COBRA, you’re able to stay with your former employer’s health plan, even if you’re no longer employed. You can keep COBRA coverage for 18 or 36 months, depending on your situation.
How much is Medicare Part B in 2021?
Medicare Part B is medical coverage, and most people pay the standard premium amount for it. In 2021, this amount is $148.50. So, for most people, Medicare will be less expensive unless their COBRA coverage has a premium that’s lower than $148.50.
When does Cobra end?
So, if you leave your job at age 64 and enroll in COBRA, your COBRA coverage will end when you turn 65 years old and enroll in Medicare.
How long can you keep your cobra?
COBRA allows you to keep your former employer’s health insurance plan for up to 36 months after you leave a job.
What are the two types of reimbursement for healthcare professinoal?
If you have more than one type of insurance coverage, the reimbursement to healthcare professinoal is divided into two types: primary and secondary. This is based on which insurance pays first and which pays second.
Does Cobra include Medicare?
Your COBRA plan will likely include coverage for medications but you’ll be responsible for paying the entire premium amount. Medicare Part D plans are available at a wide variety of premiums. You can choose a plan that fits your needs and budget.
How many employees can you have with Cobra?
In general, COBRA only applies to employers with 20 or more employees. However, some states require insurers covering employers with fewer than 20 employees to let you keep your coverage for a limited time.
What is the phone number for Cobra?
If you have questions about Medicare and COBRA, call the Benefits Coordination & Recovery Center (BCRC) at 1-855-798-2627 (TTY: 1-855-797-2627).
How long does Cobra last?
COBRA coverage generally is offered for 18 months (36 months in some cases). Ask the employer's benefits administrator or group health plan about your COBRA rights if you find out your coverage has ended and you don't get a notice, or if you get divorced.
How long do you have to sign up for Part B?
If you’re eligible for Medicare, you don’t qualify for COBRA coverage without having to pay a premium. You have 8 months to sign up for Part B without a penalty, whether or not you choose COBRA.
What is the number to call for Medicare?
If your group health plan coverage was from a state or local government employer, call the Centers for Medicare & Medicaid Services (CMS) at 1-877-267-2323 extension 61565. If your coverage was with the federal government, visit the Office of Personnel Management.
Do you have to tell Cobra if you are divorced?
You or the covered employee needs to tell the plan administrator if you qualify for COBRA because you got divorced or legally separated (court-issued separation decree) from the covered employee, or you were a dependent child or dependent adult child who's no longer a dependent.
Do you have to tell your employer if you qualify for Cobra?
Once the plan administrator is notified, the plan must let you know you have the right to choose COBRA coverage.
How long do you have to be on Cobra to get Medicare?
You have ESRD and COBRA insurance and have been eligible for Medicare for at least 30 months. COBRA is the secondary payer in this situation, and Medicare pays first for qualified services. You are 65 or over – or you are under 65 and have a disability other than ESRD – and are covered by either COBRA insurance or a retiree group health plan.
Which pays first, Medicare or ESRD?
The group health plan pays first for qualified services, and Medicare is the secondary payer. You have ESRD and COBRA insurance and have been eligible for Medicare for 30 months or fewer. COBRA pays first in this situation.
What is a group health plan?
The group health plan is your secondary payer after Medicare pays first for your health care costs. You have End-Stage Renal Disease (ESRD), are covered by a group health plan and have been entitled to Medicare for at least 30 months. The group health plan pays second, after Medicare. You have ESRD and COBRA insurance and have been eligible ...
What is Medicare Advantage?
A Medicare Advantage plan replaces your Original Medicare coverage. In addition to those basic benefits, Medicare Advantage plans can also offer some additional coverage for things like prescription drugs, dental, vision, hearing aids, SilverSneakers programs and more.
What is the primary payer for a group health plan?
You are 65 or older and are covered by a group health plan because you or your spouse is still working and the employer has 20 or more employees. The group health plan is the primary payer, and Medicare pays second.
Is Medicare the primary payer for workers compensation?
If you are covered under workers’ compensation due to a job-related injury or illness and are entitled to Medicare benefits, the workers’ compensation insurance provider will be the primary payer. There typically is no secondary payer in such cases, but Medicare may make a payment in certain situations.
Is Medicare Part A or Part B?
While you must remain enrolled in Medicare Part A and Part B (and pay the associated premiums), your Medicare Advantage plan serves as your Medicare coverage. Medicare Part D, which provides coverage for prescription drugs, is another type of private Medicare insurance.
What happens if you enroll in Cobra?
This means that if your employees enroll in COBRA instead of Medicare, once COBRA coverage ends, they will have to wait until the next annual enrollment period to enroll in Medicare, and they will have to pay late penalties. The late penalties are not minor, either. For Medicare Part B, for example, the monthly premium goes up 10 percent ...
What is the cobra law?
The Consolidated Omnibus Budget Reconciliation Act, or COBRA, is a federal law that requires employers to offer health care continuation to covered employees, their spouses and their dependents after a qualifying event. Enrollees can be required to pay 102 percent of premium costs, which includes the full premium and a 2 percent administrative fee.
How much does Medicare Part B premium go up?
For Medicare Part B, for example, the monthly premium goes up 10 percent for every 12-month period enrollment was delayed. Enrollees have to pay this penalty for the rest of their lives. If your employees are trying to decide between COBRA and Medicare, make sure they understand that they must enroll in Medicare if they want to avoid expensive ...
How to contact CMS about Medicare?
Your employees can contact the CMS Benefits Coordination & Recovery Center at 1-855-798-2627 with questions about Medicare and COBRA. As always, do your best!
Is Medicare the primary insurance?
If someone is enrolled in both COBRA and Medicare, Medicare is the primary insurance. In other words, Medicare pays first, and COBRA may pay some of the costs not covered by Medicare.
Is Medicare a qualifying event?
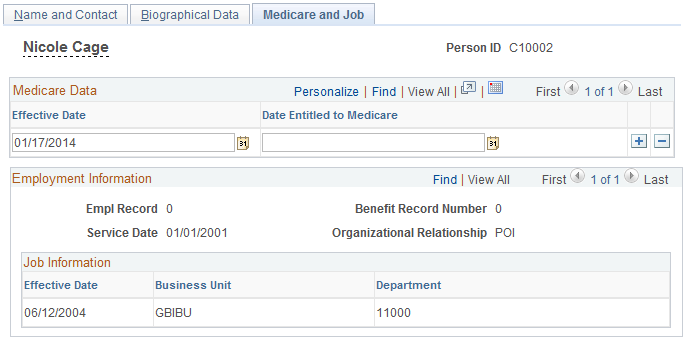
Yes. Employee enrollment in Medicare is considered a qualifying event under COBRA. Imagine this scenario: One of your employees turns 65 and ages into Medicare, but he’s not ready to retire yet. He keeps working. Now he has two health plan options: his group health plan and Medicare.
Is Cobra confusing?
COBRA administration can be confusing in the best of times. When you add complicating factors, it can seem downright baffling. Take COBRA and Medicare. Dealing with one can be a challenge – but what if your employees are dealing with both? Here’s how COBRA and Medicare interact.
Why does Bill have Medicare?
Bill has Medicare coverage because of permanent kidney failure.He also has group health plan coverage through his company.Bill’s group health plan coverage will be the primary payer forthe first 30 months after he becomes eligible for Medicare. After30 months, Medicare becomes the primary payer.
What is the original Medicare plan?
The Original Medicare Plan—This a fee-for-service plan . Thismeans you are usually charged a fee for each health care service orsupply you get. This plan, managed by the Federal Government, isavailable nationwide. You will stay in the Original Medicare Planunless you choose to join a Medicare Advantage Plan.
What does Medicare Part B cover?
Medicare Part B—Medical Insurance, helps pay fordoctors’services and outpatient care. It also covers some other medicalservices that Medicare Part A doesn’t cover, such as some of theservices of physical and occupational therapists, and some homehealth care. Medicare Part Bhelps pay for these covered services andsupplies when they are medically necessary.
Which Medicare plans cover more services?
Medicare Advantage Plans and Other Medicare HealthPlans—These plans, which include HMOs, PPOs, and PFFS plans,may cover more services and have lower out-of-pocket costs than theOriginal Medicare Plan. However, in some plans, like HMOs, youmay only be able to see certain doctors or go to certain hospitals.
Does Medicare know if you have other insurance?
Medicaredoesn’t automatically know if you have other insurance orcoverage. Medicare sends you a questionnaire called the “InitialEnrollment Questionnaire”about three months before you areentitled to Medicare. This questionnaire will ask you if you havegroup health plan insurance through your work or that of a familymember and if you plan to keep it. Your answers to thisquestionnaire are used to help Medicare set up your file, and makesure that your claimsare paid by the right insurance.
Who pays first, Medicare or Cobra?
Who pays first; COBRA, or Medicare? Medicare pays first, except when you have End-Stage Renal Disease. If you have End-Stage Renal Disease, then COBRA pays first. Medicare pays second to the extent COBRA coverage overlaps the first 30 months of Medicare eligibility.
When do you have to enroll in COBRA?
If you’re on COBRA and under 65, you must enroll in Part A and Part B during your Initial Enrollment Period. Your Initial Enrollment Period will begin three months before your 65th birthday. If you don’t join during the seven-month window, you’ll incur penalties.
How long does Cobra last?
COBRA extends group benefits for a set period of time – up to 18 months. It’s rare for COBRA to be the best option for a Medicare-eligible person. You can usually get better coverage for less money than COBRA.
Can you have cobra and Medicare at the same time?
It’s possible to have COBRA and Medicare coverage at the same time. However, they don’t coordinate the same way as employer coverage and Medicare. When you have COBRA, Medicare usually pays first, and COBRA pays second. However, it’s possible that your group insurance has special rules that will determine the primary payer.
Is Cobra a part of Medicare?
COBRA is NOT creditable coverage for Part B. If you delay enrollment you’ll face life-time penalties. You could choose to have Medicare Part A and B, alongside COBRA. But COBRA wasn’t made for Medicare.
Can you get a special enrollment period with Medicare?
Medicare allows you to qualify for a Special Enrollment Period if you lose your employer’s current health coverage, and you’re Medicare eligible . If you have COBRA when coverage ends, you won’t qualify for a Special Enrollment Period through Medicare.
Is Medicare a beast?
We know Medicare is a beast constantly unleashing new information. Luckily, you don't have to face this confusion alone. Our team of Medicare experts is ready to answer any additional questions you have. Give us a call at the number above to get your quote today. Or, fill out an online rate form to get your quote now!
How long does Cobra coverage last?
(But if COBRA covers your spouse and/or dependent children, their coverage may be extended for up to 36 months because you qualified for Medicare.) Return to Medicare Q&A Tool main page >>.
When does Cobra expire?
Therefore — regardless of how many months of COBRA coverage you’re offered — if you’re retiring before or at age 65, you should sign up for Medicare during your seven-month initial enrollment period (IEP), which expires three months after the month in which you turn 65.
How long is Cobra coverage?
In certain circumstances, if a disabled individual and non-disabled family members are qualified beneficiaries, they are eligible for up to an 11-month extension of COBRA continuation coverage, for a total of 29 months. The criteria for this 11-month disability extension is a complex area of COBRA law. We provide general information below, but if you have any questions regarding your disability and public sector COBRA, we encourage you to email us at [email protected].
What is the cobra?
The Consolidated Omnibus Budget Reconciliation Act of 1986 (COBRA) amended the Public Health Service Act, the Internal Revenue Code and the Employee Retirement Income Security Act (ERISA) to require employers with 20 or more employees to provide temporary continuation of group health coverage in certain situations where it would otherwise be terminated.
What is a Cobra notice?
A notice of COBRA rights generally includes the following information: A written explanation of the procedures for electing COBRA, The date by which the election must be made, How to notify the plan administrator of the election, The date COBRA coverage will begin, The maximum period of continuation coverage, The monthly premium amount,
How long does it take to get a Cobra notice?
Separate requirements apply to the employer and the group health plan administrator. An employer that is subject to COBRA requirements is required to notify its group health plan administrator within 30 days after an employee’s employment is terminated, or employment hours are reduced. Within 14 days of that notification, the plan administrator is required to notify the individual of his or her COBRA rights. If the employer also is the plan administrator and issues COBRA notices directly, the employer has the entire 44-day period in which to issue a COBRA election notice.
How long do you have to notify Cobra?
Qualified beneficiaries must be given an election period of at least 60 days during which each qualified beneficiary may choose whether to elect COBRA coverage.
What is the COBRA requirement?
Title XXII of the Public Health Service (PHS) Act, 42 U.S.C. §§ 300bb-1 through 300bb-8, applies COBRA requirements to group health plans that are sponsored by state or local government employers. It is sometimes referred to as “public sector” COBRA to distinguish it from the ERISA and Internal Revenue Code requirements ...
How long does an employer have to issue a Cobra election notice?
If the employer also is the plan administrator and issues COBRA notices directly, the employer has the entire 44-day period in which to issue a COBRA election notice.