Medicare covers certain supplies if a beneficiary has Medicare Part B and has diabetes. These supplies include: Blood glucose self-testing equipment and supplies Therapeutic shoes and inserts Insulin pumps
Insulin pump
An insulin pump is a medical device used for the administration of insulin in the treatment of diabetes mellitus, also known as continuous subcutaneous insulin therapy. The device configuration may vary depending on design.
Full Answer
How do I get my diabetic supplies through Medicare?
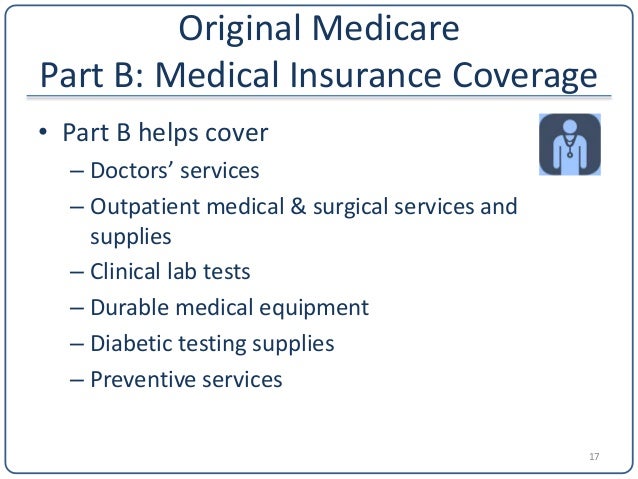
Aug 26, 2021 · You must have Part B to get services and supplies covered under Part B and you must be enrolled in a Medicare drug plan to get supplies covered under Part D. Part B covers glucose testing monitors and infusion pumps, as well as test strips, lancets, glucose sensors, therapeutic shoes or inserts, tubing, and insulin.
What supplies would a diabetic need?
supplies. 20% of the Medicare-approved amount after the yearly Part B deductible Diabetes supplies See page 16. Part D covers certain medical supplies to administer insulin (like syringes, needles, alcohol swabs, gauze, and inhaled insulin devices). Coinsurance or copayment Part D deductible may also apply
What diabetic supplies does Medicare pay for?
Aug 16, 2018 · professionals who provide diabetic supplies to Medicare beneficiaries. Medicare Part B Covered Diabetic Supplies . Medicare covers certain supplies if a beneficiary has Medicare Part B and has diabetes. These supplies include: • Blood glucose self-testing equipment and supplies • Therapeutic shoes and inserts
What are some essential diabetic supplies?
Diabetes Supplies This section provides information about Part B (Medical Insurance) and its coverage of diabetes supplies. Medicare covers certain supplies if you have diabetes and Part B, including: • Blood sugar self-testing equipment & supplies. See pages 20 – 21. • Insulin pumps. See page 26. • Therapeutic shoes or inserts.

Does Medicare cover diabetes?
This section provides information about Medicare drug coverage (Part D) for people with Medicare who have or are at risk for diabetes. To get Medicare drug coverage, you must join a Medicare drug plan. Medicare drug plans cover these diabetes drugs and supplies:
Does Part B cover insulin pumps?
Part B may cover insulin pumps worn outside the body (external), including the insulin used with the pump for some people with Part B who have diabetes and who meet certain conditions. Certain insulin pumps are considered durable medical equipment.
What is diabetes self management training?
Diabetes self-management training helps you learn how to successfully manage your diabetes. Your doctor or other health care provider must prescribe this training for Part B to cover it.
What is Part B for diabetes?
In addition to diabetes self-management training, Part B covers medical nutrition therapy services if you have diabetes or renal disease. To be eligible for these services, your fasting blood sugar has to meet certain criteria. Also, your doctor or other health care provider must prescribe these services for you.
What is part B?
Part B covers a once-per-lifetime health behavior change program to help you prevent type 2 diabetes. The program begins with weekly core sessions in a group setting over a 6-month period. In these sessions, you’ll get:
What is the A1C test?
A hemoglobin A1c test is a lab test that measures how well your blood sugar has been controlled over the past 3 months. If you have diabetes, Part B covers this test if your doctor orders it.
How often do you have to have your eyes checked for glaucoma?
Part B will pay for you to have your eyes checked for glaucoma once every 12 months if you’re at increased risk of glaucoma. You’re considered high risk for glaucoma if you have:
Does Medicare cover therapeutic shoes?
If a beneficiary has Medicare Part B, has diabetes, and meets certain conditions (see below), Medicare will cover therapeutic shoes if they need them. The types of shoes that are covered each year include one of the following:
What is CMS in healthcare?
The Centers for Medicare & Medicaid Services (CMS) has developed a variety of educational resources for use by health care professionals and their staff as part of a broad outreach campaign to promote awareness and increase utilization of preventive services covered by Medicare. For more information about coverage, coding, billing, and reimbursement of Medicare-covered preventive services and screenings, visit
Does Medicare cover DME equipment?
You may be able to choose whether to rent or buy the equipment. Medicare will only cover your DME if your doctors and DME suppliers are enrolled in Medicare. Doctors and suppliers have to meet strict standards to enroll and stay enrolled in Medicare.
What is Medicare approved amount?
Medicare-Approved Amount. In Original Medicare, this is the amount a doctor or supplier that accepts assignment can be paid. It may be less than the actual amount a doctor or supplier charges. Medicare pays part of this amount and you’re responsible for the difference. , and the Part B.
What percentage of Medicare payment does a supplier pay for assignment?
If your supplier accepts Assignment you pay 20% of the Medicare-approved amount, and the Part B Deductible applies. Medicare pays for different kinds of DME in different ways. Depending on the type of equipment:
What is original Medicare?
Your costs in Original Medicare. An agreement by your doctor, provider, or supplier to be paid directly by Medicare, to accept the payment amount Medicare approves for the service, and not to bill you for any more than the Medicare deductible and coinsurance.
What is Medicare assignment?
assignment. An agreement by your doctor, provider, or supplier to be paid directly by Medicare, to accept the payment amount Medicare approves for the service, and not to bill you for any more than the Medicare deductible and coinsurance. you pay 20% of the. Medicare-Approved Amount.
How to find out how much a test is?
To find out how much your test, item, or service will cost, talk to your doctor or health care provider. The specific amount you’ll owe may depend on several things, like: 1 Other insurance you may have 2 How much your doctor charges 3 Whether your doctor accepts assignment 4 The type of facility 5 Where you get your test, item, or service
Does Medicare cover diabetes?
Get prescriptions from your doctor for any medication, supply, or service you’ll want Medicare to cover. Check that your pharmacy or device supplier accepts Medicare set payment rates to avoid overpaying. Diabetes is a metabolic condition that leads to high blood sugar levels.
Do you have to be enrolled in Medicare to get Part D?
You must be enrolled in original Medicare (parts A and B) to be eligible for Part D. Medicare Part D covers medications you take at home, insulin you self-inject andsupplies for insulin like needles and syringes. Check with the individual planon specific medications and costs.
What are the challenges of diabetics?
Older adults with diabetes face unique challenges. Trusted Source. including hypoglycemia, brain and nervous system problems, and social support issues that require special monitoring to manage risks. There are many types of diabetic supplies needed for preventive screening, monitoring, and managing the condition.
What is Medicare Part D?
Medicare Part D plans are private plans that cover medications that treat diabetes, including insulin and supplies to inject insulin. You must be enrolled in original Medicare (parts A and B) to be eligible for Part D.
How much does Medicare Part B coinsurance cost?
Under Medicare Part B, you’ll pay coinsurance costs (typically 20 percent ). As long as the pharmacy you use accepts assignment, the costs will be lower than with a nonparticipating provider.
What are the parts of Medicare?
Medicare parts B, C, and D each covers different supplies, medications, and services needed to manage diabetes. Make sure you go to pharmacies or equipment providers that are enrolled in Medicare and accept the assignment prices set by Medicare.
Why is my blood sugar high?
Diabetes is a condition in which blood sugar levels are high because the body either doesn’t produce enough insulin ( type 1) or doesn’t use/produce the insulin effectively ( type 2 ), or develops temporary insulin resistance ( gestational diabetes) during pregnancy. Type 2 diabetes is the most common form.
Does Medicare cover diabetic supplies?
A Medicare Supplement (Medigap) plan can help cover your Medicare out-of-pocket costs for diabetic supplies. Medicare does cover certain diabetic supplies and treatments.
What supplies does Medicare cover?
HEALTH FEATURE ARCHIVE Diabetes Supplies: What Medicare Covers 1. Self-testing equipment and supplies: Medicare Part B covered diabetes supplies: Coverage for glucose monitors, test strips, and lancets. Who is covered: All people with Medicare who have diabetes (insulin users and non-users). Medicare covers the same supplies for people with diabetes whether or not they use insulin. These include glucose testing monitors, blood glucose test strips, lancet devices and lancets, and glucose control solutions. There may be some limits on supplies or how often you get them. For more information about diabetic supplies, call your Durable Medical Equipment Regional Carrier. How to get your diabetes equipment and supplies: To get your diabetes equipment and supplies under Medicare, you need a prescription from your doctor. The prescription should say: You have been diagnosed with diabetes. How many test strips and lancets you need in a month. What kind of meter you need. For example, if you need a special meter for vision problems, the doctor should say that and state the medical reason why you need a special meter. Whether you use insulin or not. How often you should test your blood sugar. Points to remember: Ask your doctor or health care provider if regular blood sugar testing is right for you. You need a prescription from your doctor to get your diabetes equipment and supplies under Medicare. Learn the correct way to use your blood sugar meter properly. Your pharmacist, doctor, diabetes educator, or another health care provider can help you. Keep track of your blood sugar readings and share them with your doctor or health care provider at regular visits. Do not accept shipments of diabetes equipment and supplies that you did not ask for. 2. Therapeutic shoes: Medicare also c Continue reading >>
Does Medicare accept assignment?
Non-Mail-Order supplier, Medicare enrolled and accepts Assignment Non-Mail-Order supplier, Medicare enrolled and does not accept Assignment Non-Mail-Order supplier, not Medicare enrolled and does not accept Assignment A Mail-Order supplier must accept assignment and must be enrolled in Medicare. [21] . A beneficiary who purchases supplies ...
Does Medicare pay for blood glucose testing?
Blood glucose testing is an important part of diabetes management. Most insurance companies and Medicare/Medicaid will pay for blood glucose testing supplies. With private insurance or managed care, patients will most likely be asked to pay a co-pay to cover part of the cost of the supplies.
How much does Medicare cover?
If your doctors and suppliers are enrolled in and participate in Medicare, and if the supplies are considered medically necessary, Medicare typically covers 80% of the Medicare-approved amount, and you pay the remaining 20% (after you pay your yearly Part B deductible).
Does Medicare cover insulin?
Who is covered: All people with Medicare who have diabetes (insulin users and non-users). Medicare covers the same supplies for people with diabetes whether or not they use insulin. These include glucose testing monitors, blood glucose test strips, lancet devices and lancets, and glucose control solutions.
What is DTS in Medicare?
As a component of the Center of Medicare & Medicaid Services (CMS) Competitive Bidding Program, diabetes testing supplies (DTS) are provided through mail order at asubstantial discount for people with diabetes (PWD). PWD must be enlisted in Medicare Part B to qualify for mail order service. Covered DTS include blood glucose meters, replacement batteries for blood glucose meters, control solution, test strips, lancet devices, and lancets. Medicare recipients who want to have DTS shipped directly to their home must utilize one of nine authorized mail order suppliers. Select the option Mail-Order Diabetic Supplies. Most suppliers will offer a link showing which brands they cover. Although, PWD should be directed to get a hold of the mail order program to confirm brand coverage and to place their order as well. For people requiring insulin, Medicare will cover 300 test strips and lancets (~3 per day) every 3 MONTHS and 1 lancet device every 6 MONTHS. For people who do not require insulin, Medicare covers 100 test strips and lancets (~1 per day) every 3 MONTHS and 1 lancet device every 6 MONTHS. Additional test strips may be requested by the prescriber stating medical necessity. What if the mail order suppliers do not carry the meter brand and strips I use? You have some options, request your medical professional to provide you with a prescription that includes the meters brand name along with the words: NO SUBSTITUTION. They must also indicate in your medical record the reason this particular brand is required. If the mail order supplier doesnt carry that brand, they will help you determine someone who does, or assist you in finding a brand that you and your medical professional believe is ideal for you. Purchase your preferred diabetes testing supplies at your local pharm Continue reading >>
