How has Medicare enrollment changed over time?
The total number of Medicare beneficiaries has been steadily growing as well, but the growth in Medicare Advantage enrollment has far outpaced overall Medicare enrollment growth. In 2004, just 13% of Medicare beneficiaries had Medicare Advantage plans. That had grown to more than 43% by 2021.
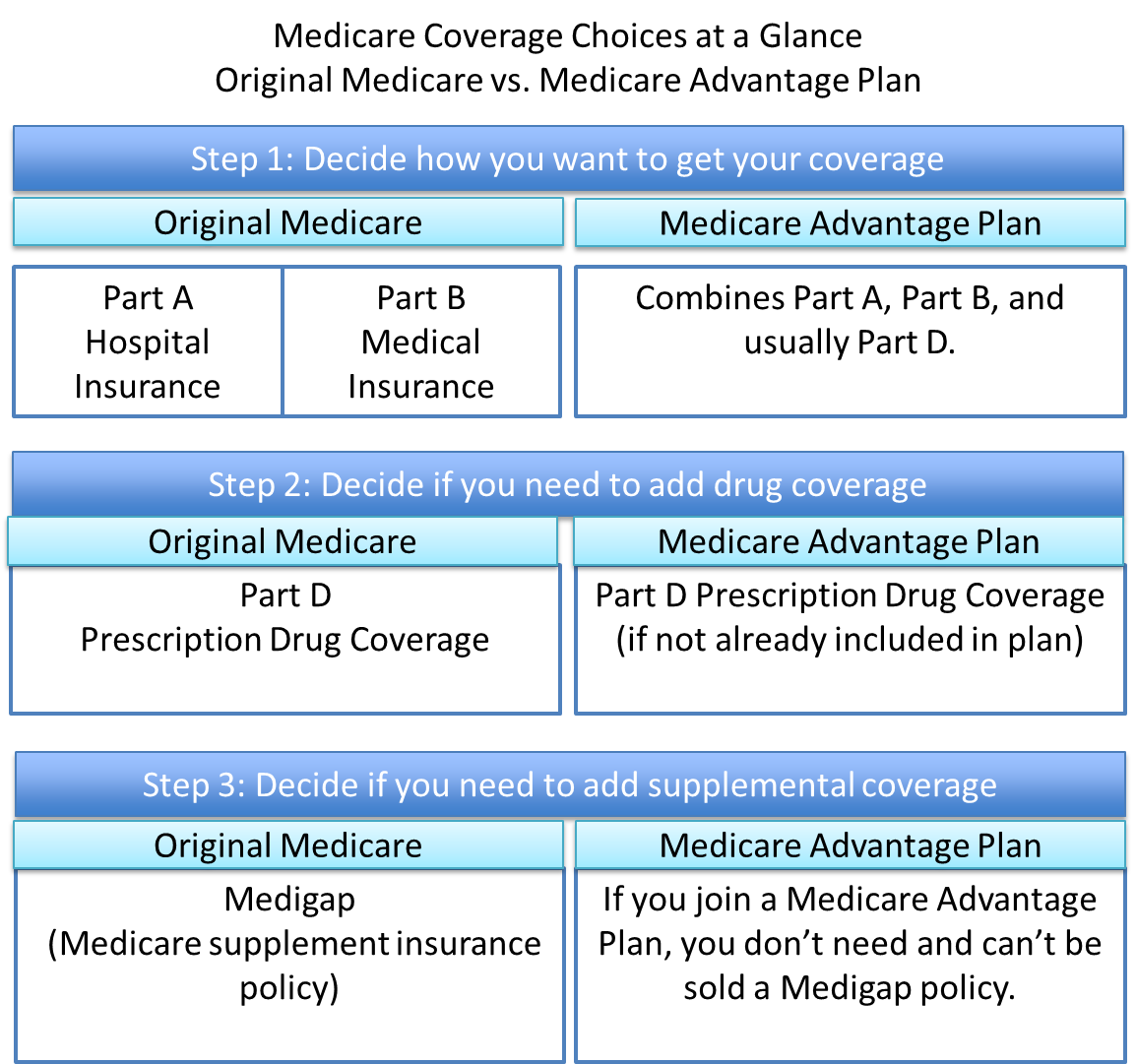
How to choose or change your Medicare coverage?
Choosing or Changing your Medicare Coverage 8 ways of Choosing or Changing your Medicare coverage. They include Coverage, Your other coverage, Costs, Doctor and hospital choice, Prescription drugs, Quality of care, Convenience, Travel. Skip Navigation
How long does it take to change your Medicaid eligibility status?
This is because circumstances, such as an increase in income or an inheritance, can result in one being ineligible for Medicaid. Most states allow between 10 and 30 days to report any such changes.
When does Medicare coverage start?
The start of your Medicare depends on your specific situation and when you enrolled. Below, we’ll go over what you need to know about when Medicare coverage starts. When Does Medicare Start? For most people, Medicare coverage starts the first day of the month you turn 65.

Do Medicaid and Medicare cover the same things?
Medicaid programs vary from state to state, but most health care costs are covered if you qualify for both Medicare and Medicaid. pays second. Medicaid never pays first for services covered by Medicare. It only pays after Medicare, employer group health plans, and/or Medicare Supplement (Medigap) Insurance have paid.
When can Medicare coverage be changed?
Medicare provides certain time periods when you can change Medicare plans. The main one is the Medicare Annual Enrollment Period, which runs from October 15 to December 7 each year. Anyone on Medicare can make coverage changes during this time that then go into effect the following year.
When can a patient have both Medicare and Medicaid?
Some people qualify for both Medicare and Medicaid and are called “dual eligibles.” If you have Medicare and full Medicaid coverage, most of your health care costs are likely covered.
What are the disadvantages of Medicaid?
Disadvantages of Medicaid They will have a decreased financial ability to opt for elective treatments, and they may not be able to pay for top brand drugs or other medical aids. Another financial concern is that medical practices cannot charge a fee when Medicaid patients miss appointments.
What are the negatives of a Medicare Advantage plan?
Medicare Advantage can become expensive if you're sick, due to uncovered copays. Additionally, a plan may offer only a limited network of doctors, which can interfere with a patient's choice. It's not easy to change to another plan. If you decide to switch to a Medigap policy, there often are lifetime penalties.
Can you switch back to Medicare from Medicare Advantage?
Yes, you can elect to switch to traditional Medicare from your Medicare Advantage plan during the Medicare Open Enrollment period, which runs from October 15 to December 7 each year. Your coverage under traditional Medicare will begin January 1 of the following year.
What is the highest income to qualify for Medicaid?
Federal Poverty Level thresholds to qualify for Medicaid The Federal Poverty Level is determined by the size of a family for the lower 48 states and the District of Columbia. For example, in 2022 it is $13,590 for a single adult person, $27,750 for a family of four and $46,630 for a family of eight.
Does Medicaid pay Medicare premiums?
Medicaid pays Part A (if any) and Part B premiums. Medicaid is liable for Medicare deductibles, coinsurance, and copayments for Medicare-covered items and services. Even if Medicaid doesn't fully cover these charges, the QMB isn't liable for them.
When a patient is covered through Medicare and Medicaid which coverage is primary?
Medicaid can provide secondary insurance: For services covered by Medicare and Medicaid (such as doctors' visits, hospital care, home care, and skilled nursing facility care), Medicare is the primary payer. Medicaid is the payer of last resort, meaning it always pays last.
Which state has best Medicaid program?
New YorkStates with the Best Medicaid Benefit ProgramsRankStateTotal Spending Per Person1New York$12,5912New Hampshire$11,5963Wisconsin$10,0904Minnesota$11,63346 more rows•Jun 16, 2020
Is Medicare better than Medicaid?
Medicaid and Original Medicare both cover hospitalizations, doctors and medical care. But Medicaid's coverage is usually more comprehensive, including prescription drugs, long-term care and other add-ons determined by the state such as dental care for adults.
Does Medicaid cover surgery?
Medicaid does cover surgery as long as the procedure is ordered by a Medicaid-approved physician and is deemed medically necessary. Additionally, the facility providing the surgery must be approved by Medicaid barring emergency surgery to preserve life.
Q: What are the changes to Medicare benefits for 2022?
A: There are several changes for Medicare enrollees in 2022. Some of them apply to Medicare Advantage and Medicare Part D, which are the plans that...
How much will the Part B deductible increase for 2022?
The Part B deductible for 2022 is $233. That’s an increase from $203 in 2021, and a much more significant increase than normal.
Are Part A premiums increasing in 2022?
Roughly 1% of Medicare Part A enrollees pay premiums; the rest get it for free based on their work history or a spouse’s work history. Part A premi...
Is the Medicare Part A deductible increasing for 2022?
Part A has a deductible that applies to each benefit period (rather than a calendar year deductible like Part B or private insurance plans). The de...
How much is the Medicare Part A coinsurance for 2022?
The Part A deductible covers the enrollee’s first 60 inpatient days during a benefit period. If the person needs additional inpatient coverage duri...
Can I still buy Medigap Plans C and F?
As a result of the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA), Medigap plans C and F (including the high-deductible Plan F) are n...
Are there inflation adjustments for Medicare beneficiaries in high-income brackets?
Medicare beneficiaries with high incomes pay more for Part B and Part D. But what exactly does “high income” mean? The high-income brackets were in...
How are Medicare Advantage premiums changing for 2021?
According to CMS, the average Medicare Advantage (Medicare Part C) premiums for 2022 is about $19/month (in addition to the cost of Part B), which...
Is the Medicare Advantage out-of-pocket maximum changing for 2022?
Medicare Advantage plans are required to cap enrollees’ out-of-pocket costs for Part A and Part B services (unlike Original Medicare, which does no...
How is Medicare Part D prescription drug coverage changing for 2022?
For stand-alone Part D prescription drug plans, the maximum allowable deductible for standard Part D plans is $480 in 2022, up from $445 in 2021. A...
The Initial Enrollment Period (IEP)
The Initial Enrollment Period is the first opportunity (and often the best time) to enroll in Medicare. This is a seven-month window during which you can sign up for Medicare Parts A, B, C and D. The seven months are aligned with your date of birth:
Medicare Coverage When Automatically Enrolled
If you are already receiving Social Security or Railroad Retirement Board benefits before your 65th birthday, you will be automatically enrolled in Medicare Parts A and B when you turn 65. In such a case, your Medicare coverage will begin on the first day of the month you turn 65.
Medicare Coverage for General Enrollment Period (GEP)
If you miss out on the seven-month window of IEP, and you are not automatically enrolled in Medicare, you can sign up during the General Enrollment Period. General Enrollment runs every year, starting from January 1st to March 31st. In this case, your Medicare coverage starts on July 1 of the same year you enroll.
Special Enrollment Period (SEP)
In some cases, you might be eligible for special enrollment depending on circumstances that affect your current health insurance coverage. For instance, you may have moved (plan options can vary by region) or lost creditable coverage – such as when you or your spouse retire and lose employment coverage benefits.
Your other coverage
Do you have, or are you eligible for, other types of health or prescription drug coverage (like from a former or current employer or union)? If so, read the materials from your insurer or plan, or call them to find out how the coverage works with, or is affected by, Medicare.
Cost
How much are your premiums, deductibles, and other costs? How much do you pay for services like hospital stays or doctor visits? What’s the yearly limit on what you pay out-of-pocket? Your costs vary and may be different if you don’t follow the coverage rules.
Doctor and hospital choice
Do your doctors and other health care providers accept the coverage? Are the doctors you want to see accepting new patients? Do you have to choose your hospital and health care providers from a network? Do you need to get referrals?
Prescription drugs
Do you need to join a Medicare drug plan? Do you already have creditable prescription drug coverag e? Will you pay a penalty if you join a drug plan later? What will your prescription drugs cost under each plan? Are your drugs covered under the plan’s formulary? Are there any coverage rules that apply to your prescriptions?
Quality of care
Are you satisfied with your medical care? The quality of care and services given by plans and other health care providers can vary. Get help comparing plans and providers
Convenience
Where are the doctors’ offices? What are their hours? Which pharmacies can you use? Can you get your prescriptions by mail? Do the doctors use electronic health records prescribe electronically?
When does Medicare start?
For most people, Medicare coverage starts the first day of the month you turn 65. Some people delay enrollment and remain on an employer plan. Others may take premium-free Part A and delay Part B. If someone is on Social Security Disability for 24 months, they qualify for Medicare. Those with End-Stage Renal Disease will be immediately eligiblee ...
Is group coverage better than Medicare?
In this scenario, delaying enrollment would make sense, especially if the coverage is better than Medicare. Although, group coverage better than Medicare isn’t the typical scenario. Many people work for small employers;
Can you get Medicare if you have ALS?
Those with End-Stage Renal Disease will be immediately eligiblee for Medicare with a diagnosis. When Medicare starts is different for each beneficiary. People with disabilities, ALS, or End-Stage Renal Disease may be eligible for Medicare before they’re 65. If you qualify for Medicare because of a disability, there is no minimum age ...
Can you have Cobra if you don't have Medicare?
So, if you don’t have Medicare, and you only have the group plan, the employer plan won’t pay until your Medicare is active. Further, COBRA is NOT creditable coverage for Medicare. When you delay Part B without creditable coverage, a late enrollment penalty could be coming your way.
When will Medicare Part D change to Advantage?
Some of them apply to Medicare Advantage and Medicare Part D, which are the plans that beneficiaries can change during the annual fall enrollment period that runs from October 15 to December 7.
When will Medicare stop allowing C and F?
As a result of the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA), Medigap plans C and F (including the high-deductible Plan F) are no longer available for purchase by people who become newly-eligible for Medicare on or after January 1, 2020.
What is the maximum out of pocket limit for Medicare Advantage?
The maximum out-of-pocket limit for Medicare Advantage plans is increasing to $7,550 for 2021. Part D donut hole no longer exists, but a standard plan’s maximum deductible is increasing to $445 in 2021, and the threshold for entering the catastrophic coverage phase (where out-of-pocket spending decreases significantly) is increasing to $6,550.
What is the Medicare premium for 2021?
The standard premium for Medicare Part B is $148.50/month in 2021. This is an increase of less than $4/month over the standard 2020 premium of $144.60/month. It had been projected to increase more significantly, but in October 2020, the federal government enacted a short-term spending bill that included a provision to limit ...
How much is the Medicare coinsurance for 2021?
For 2021, it’s $371 per day for the 61st through 90th day of inpatient care (up from $352 per day in 2020). The coinsurance for lifetime reserve days is $742 per day in 2021, up from $704 per day in 2020.
How many people will have Medicare Advantage in 2020?
People who enroll in Medicare Advantage pay their Part B premium and whatever the premium is for their Medicare Advantage plan, and the private insurer wraps all of the coverage into one plan.) About 24 million people had Medicare Advantage plans in 2020, and CMS projects that it will grow to 26 million in 2021.
What is the income bracket for Medicare Part B and D?
The income brackets for high-income premium adjustments for Medicare Part B and D will start at $88,000 for a single person, and the high-income surcharges for Part D and Part B will increase in 2021. Medicare Advantage enrollment is expected to continue to increase to a projected 26 million. Medicare Advantage plans are available ...
When does Medicare enrollment end?
includes the month you turn age 65. ends three months after that birthday. If you don’t enroll in Medicare Part B duringyour initial enrollment period, there is a general enrollment period every ...
When does Medicare start paying for dialysis?
You have end stage renal disease (also known as ESRD or end-stage kidney disease). Your Medicare coverage starts on the 4th month of dialysis treatments. If you participate in a home dialysis training program, your coverage could potentially start on the first month of dialysis.
How long does it take to get insurance after turning 65?
If you sign up in the month after you turn 65, your coverage will start 2 months after you sign up. If you sign up 2 months after you turn 65, your coverage will start 3 months after you sign up. If you sign up 3 months after you turn 65, your coverage will start 3 months after you sign up.
What is the Medicare Part A and B?
You have amyotrophic lateral sclerosis (also known as ALS or Lou Gehrig’s disease). You will be automatically enrolled in Medicare Part A and B the first month your Social Security and Railroad Retirement disability benefits begin. You have end stage renal disease (also known as ESRD or end-stage kidney disease).
How long do you have to wait to enroll in Medicare after dropping it?
There are rules for re-enrolling in Medicare after you’ve dropped it for an employer-sponsored health plan. You’ll have an 8-month Special Enrollment Period in which to re-enroll in Medicare Part A and Part B. If you miss this window, you’ll have to wait to enroll in the Medicare General Enrollment Period (January 1 – March 31) ...
What happens if you drop Medicare?
If you drop Medicare and don’t have creditable employer coverage, you’ll face penalties when getting Medicare back. Before you decide to drop any part of Medicare, there are some things you’ll want to think about, especially as some choices could end up being costly.
How long do you have to enroll in Medicare after you lose your employer?
NOTE: While you have eight months for Parts A & B, you only get two months after losing the employer coverage or leaving work to re-enroll in a Medicare Part D prescription drug plan or a Medicare Advantage (Part C) plan. If you enroll later, you’ll face late enrollment penalties for Part D.
What is Medicare Made Clear?
Medicare Made Clear is brought to you by UnitedHealthcare to help make understanding Medicare easier. Click here to take advantage of more helpful tools and resources from Medicare Made Clear including downloadable worksheets and guides.
How long does it take for Medicaid to report changes?
Most states require Medicaid beneficiaries to report any change in income or assets within 30 days.
What happens if you don't renew your medicaid?
Failure to renew can result in loss of benefits. If a Medicaid beneficiary does not complete the redetermination process in time, Medicaid benefits will cease and there will be a lack of coverage.
How often does Medicaid redetermination happen?
However, generally speaking, Medicaid redetermination is limited to once every 12 months. To be clear, adults aged 65 and over, persons eligible for Home and Community Based Services, those eligible for SSI, and institutionalized individuals in nursing homes all fall must renew their Medicaid.
What is Medicaid renewal?
Medicaid renewal, also called Medicaid redetermination or recertification, is a necessary part of being a Medicaid beneficiary, regardless of if you receive benefits through the regular state plan, get long-term home and community based services (HCBS) via a Medicaid waiver, or are on nursing home Medicaid. The Medicaid redetermination process ...
Can you still receive medicaid if you are disabled?
The Medicaid redetermination process ensures one is still eligible to receive Medicaid benefits, and in the case of many seniors and disabled persons, continue to receive Medicaid-funded long-term services and supports.
Can Medicaid recipients be verified electronically?
For example, in some situations, the Medicaid recipient’s income and / or assets may not be able to be verified electronically. As an example, rental income and self-employment are two types of income that cannot be verified via electronic databases.
Can a public benefits counselor assist a Medicaid recipient?
However, if a Medicaid recipient no longer meets the eligibility criteria, a public benefits counselor cannot assist. For example, if the beneficiary receives an inheritance and now have assets valued above the Medicaid limit, they will not receive assistance from a public benefits counselor.