Modifier 58 appropriate for example; hardware removal was planned as part of therapeutic approach involving multiple, staged procedures to the surgical intervention Physicians in the same specialty, same group are to bill and are reimbursed as a single physician
Full Answer
What diagnosis codes are covered by Medicare?
Aug 26, 2010 · Modifier 58 appropriate for example; hardware removal was planned as part of therapeutic approach involving multiple, staged procedures to the surgical intervention Physicians in the same specialty, same group are to bill and are reimbursed as a single physician Use modifier 78 for treatment problems unplanned requiring return trip to operating room
What is Code 58?
Report condition code 58. Interrupted Stay The patient is discharged from a Part A-covered stay and subsequently resumes SNF care in the same SNF for a Medicare Part A-covered stay during a 3-day period, starting with the calendar day of Part A discharge and including the 2 immediately following calendar days, which is referred to as an interruption window.
What is CPT code 58?
Dec 20, 2020 · D6. Use when canceling a claim for reasons other than the Medicare ID or provider number. Use when canceling a claim to repay a payment. Condition code only applicable to a xx8 type of bill. D1. If one of the above condition codes does not apply and there is a change to the COVERED charges this code should be used.
What are codes for Medicare OB?
Polling questions to help code claim examples MSP Resources Questions and Answers. 6. Part A. Recap: MSP Billing and Claim ... Condition codes; 20–28; 2300.HI (BG) Page 01. Occurrence codes and dates; 31–34. 2300.HI (BH) ... A primary payer name as first payer and Medicare as second • FLs 50, 58, 60, 61 and 62 (or electronic equivalent ...
What are condition codes used for?
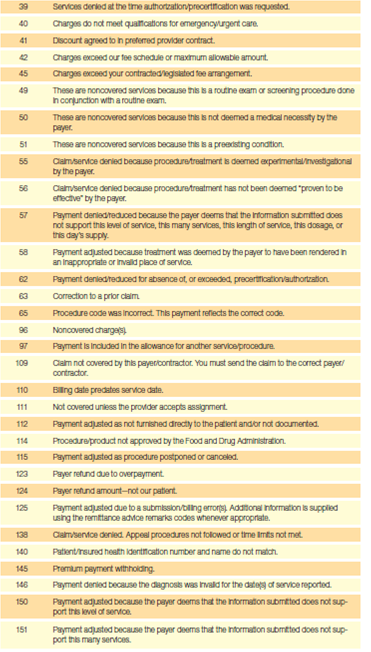
Currently, Condition Codes are designed to allow the collection of information related to the patient, particular services, service venue and billing parameters which impact the processing of an Institutional claim.
What is a condition code for Medicare?
Condition codes refer to specific form locators in the UB-04 form that demand to describe the conditions applicable to the billing period. It is important to note that condition codes are situational. These codes should be entered in an alphanumeric sequence.Dec 17, 2021
Where does a condition code go on CMS 1500?
The Condition Codes may be reported in field 10D of the 1500 Claim Form. However, entities reporting these codes should refer to the most current instructions for any federal, state, or individual payment specific instructions that may be applicable to the 1500 Claim Form.
What condition code is for not hospice related?
Hospice services covered under the Medicare hospice benefit are billed by the Medicare hospice. Institutional providers may submit claims to Medicare with the condition code "07" when services provided are not related to the treatment of the terminal condition.Mar 11, 2022
What are condition codes list the different condition codes?
Condition codesconditional control flow (branching)evaluation of boolean expressions.overflow detection.multiprecision arithmetic.
What is condition code F?
Condition CodesCondition CodeShort DescriptionDServiceable (Test/Modification)EUnserviceable (Limited Restoration)FUnserviceable (Reparable)GUnserviceable (Incomplete)3 more rows
What goes in box 22 on a CMS 1500?
Complete box 22 (Resubmission Code) to include a 7 (the "Replace" billing code) to notify us of a corrected or replacement claim, or insert an 8 (the “Void” billing code) to let us know you are voiding a previously submitted claim.Apr 8, 2015
What is condition code go?
Hospitals should report condition code G0 on FLs 24-30 when multiple medical visits occurred on the same day in the same revenue center but the visits were distinct and constituted independent visits.Jan 10, 2019
What goes in box 19 on a CMS 1500?
Services rendered to an infant may be billed with the mother's ID for the month of birth and the month after only. Enter “Newborn using Mother's ID”/ “(twin a) or (twin b)” in the Reserved for Local Use field (Box 19). 3 Required Patient's Birth date - Enter member's date of birth and check the box for male or female.
What is an A6 condition code for Medicare?
Special ProgramCodeDescriptionA6Pneumococcal pneumonia and influenza vaccines paid at 100%.A9Second opinion for surgery.AJPayer responsible for co-payment.ANPreadmission screening not required.11 more rows•Dec 21, 2020
What is condition code W2 for Medicare?
By using the "W2" condition code, the hospital attests that there is no pending appeal with respect to a previously submitted Part A claim, and that any previous appeal of the Part A claim is final or binding or has been dismissed, and that no further appeals shall be filed on the Part A claim.Mar 22, 2013
What are the hospice modifiers for Medicare?
Hospice Modifier GV Claims from the attending physician for services provided to hospice-enrolled patients may be submitted to Palmetto GBA with Healthcare Common Procedure Coding System (HCPCS) modifier GV. This is true regardless whether the care is related to the patient's terminal illness.Mar 19, 2021
What is SNF in Medicare?
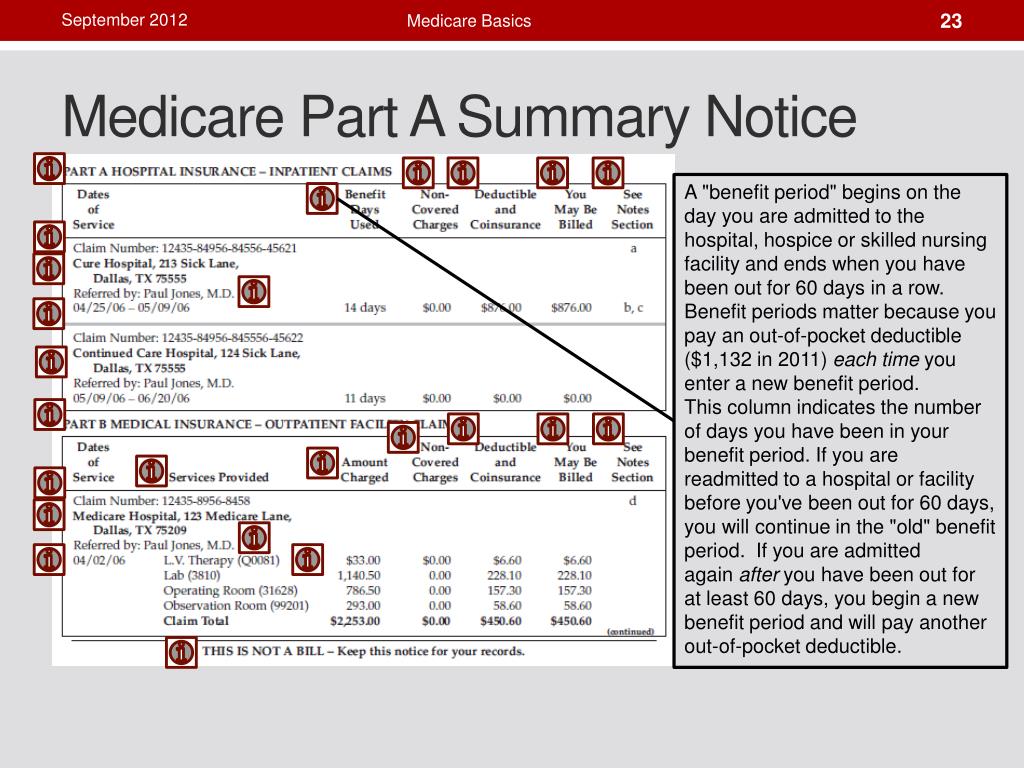
For more information about patient coverage, costs, and care in a SNF, refer to Section 2, pages 97–98 of Your Medicare Benefits. Benefit Period. Medicare measures SNF coverage in benefit periods (sometimes called “spells of illness”), beginning the day the patient admits to a hospital or SNF as an inpatient.
How long does SNF last?
The SNF benefit covers 100 days of care per episode of illness with an additional 60-day lifetime reserve. After 100 days, the SNF coverage during that benefit period “exhausts.” The next benefit period begins after patient hospital or SNF discharge for 60 consecutive days.
When does the SNF benefit period end?
The benefit period ends after the patient discharges from the hospital or has had 60 consecutive days of SNF skilled care. Once the benefit period ends, a new benefit period begins when the patient admits to a hospital or SNF. New benefit periods don’t begin with a change in diagnosis, condition, or calendar year.
Does Medicare cover SNF?
If the SNF care isn’t medically reasonable and necessary, or considered custodial care, Medicare Part A may not cover the SNF care and give them a Fee-for-Service (FFS) Skilled Nursing Facility Advance Beneficiary Notice (SNF ABN), Form CMS-10055.
What is Medicare Administrative Contractor?
The Medicare Administrative contractor is hereby advised that this constitutes technical direction as defined in your contract. CMS does not construe this as a change to the MAC statement of Work. The contractor is not obliged to incur costs in excess of the amounts allotted in your contract unless and until specifically authorized by the Contracting Officer. If the contractor considers anything provided, as described above, to be outside the current scope of work, the contractor shall withhold performance on the part(s) in question and immediately notify the Contracting Officer, in writing or by e-mail, and request formal directions regarding continued performance requirements.
Does the revision date apply to red italicized material?
Disclaimer for manual changes only: The revision date and transmittal number apply only to red italicized material. Any other material was previously published and remains unchanged. However, if this revision contains a table of contents, you will receive the new/revised information only, and not the entire table of contents.
What is a 36N general care patient?
36#N#General Care Patient in a Special Unit#N#(Not used by hospitals under PPS.) The hospital temporarily placed the patient in a special care unit because no general care beds were available.#N#Accommodation charges for this period are at the prevalent semi-private rate.
Is Medicare a secondary insurance?
Medicare may be a secondary insurer if the patient is also covered by employer group health insurance during the patient’s first 30 months of end stage renal disease entitlement. 07. Treatment of Non-terminal Condition for Hospice Patient.