Post-acute care simply refers to medical services that you receive after a more serious illness or injury. The Medicare guidelines for inpatient rehabilitation and outpatient care include coverage for medically necessary post-acute services.
Does Medicare cover post-acute care after a hospital stay?
An estimated 40 percent of people with Medicare require post-acute care after a hospital stay – for example, at a skilled nursing facility. Coinsurance costs work a little differently when you’re admitted to a skilled nursing facility.
When does Medicare cover inpatient hospital care?
Inpatient hospital care. covers inpatient hospital care when all of these are true: You’re admitted to the hospital as an inpatient after an official doctor’s order, which says you need inpatient hospital care to treat your illness or injury. The hospital accepts Medicare.
What does Medicare Part a hospital insurance cover?
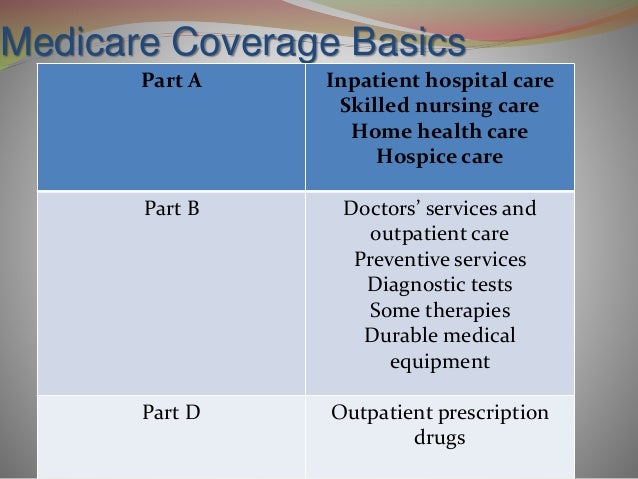
Medicare Part A hospital insurance covers inpatient hospital care, skilled nursing facility, hospice, lab tests, surgery, home health care. What Part B covers Learn about what Medicare Part B (Medical Insurance) covers, including doctor and other health care providers' services and outpatient care.
What's covered by Medicare Advantage plans?
What's covered? If you're in a Medicare Advantage Plan or other Medicare plan, your plan may have different rules. But, your plan must give you at least the same coverage as Original Medicare. Some services may only be covered in certain facilities or for patients with certain conditions.

Which part of Medicare reimburses for post acute care services?
Medicare Part AInformation on services and procedures provided to Medicare Part A (Hospital Insurance) beneficiaries by home health agencies, hospices, skilled nursing facilities, inpatient rehabilitation facilities, and long-term care hospitals.
Does Medicare cover post op?
Summary: Medicare may cover both inpatient and outpatient rehabilitation after an operation, as well as in-home care. Your recovery time is influenced by your age, health, and the complexity of the operation.
What happens when Medicare hospital days run out?
Medicare will stop paying for your inpatient-related hospital costs (such as room and board) if you run out of days during your benefit period. To be eligible for a new benefit period, and additional days of inpatient coverage, you must remain out of the hospital or SNF for 60 days in a row.
What is Medicare acute?
Acute care hospitals that provide treatment for patients who stay, on average, more than 25 days. Most patients are transferred from an intensive or critical care unit. Services provided include comprehensive rehabilitation, respiratory therapy, head trauma treatment, and pain management.
Does Medicare pay 100 percent of hospital bills?
According to the Centers for Medicare and Medicaid Services (CMS), more than 60 million people are covered by Medicare. Although Medicare covers most medically necessary inpatient and outpatient health expenses, Medicare reimbursement sometimes does not pay 100% of your medical costs.
How many times will Medicare pay for rehab?
Medicare pays for rehabilitation deemed reasonable and necessary for treatment of your diagnosis or condition. Medicare will pay for inpatient rehab for up to 100 days in each benefit period, as long as you have been in a hospital for at least three days prior.
How many days will Medicare pay for hospital stay?
90 daysDoes the length of a stay affect coverage? Medicare covers a hospital stay of up to 90 days, though a person may still need to pay coinsurance during this time. While Medicare does help fund longer stays, it may take the extra time from an individual's reserve days. Medicare provides 60 lifetime reserve days.
What is the 3 day rule for Medicare?
The 3-day rule requires the patient have a medically necessary 3-consecutive-day inpatient hospital stay. The 3-consecutive-day count doesn't include the discharge day or pre-admission time spent in the Emergency Room (ER) or outpatient observation.
Is there a maximum amount Medicare will pay?
In general, there's no upper dollar limit on Medicare benefits. As long as you're using medical services that Medicare covers—and provided that they're medically necessary—you can continue to use as many as you need, regardless of how much they cost, in any given year or over the rest of your lifetime.
What is the difference between acute care and long-term care?
Most people who need inpatient hospital services are admitted to an “acute‑care” hospital for a relatively short stay. But some people may need a longer hospital stay. Long‑term care hospitals (LTCHs) are certified as acute‑care hospitals, but LTCHs focus on patients who, on average, stay more than 25 days.
What is an acute care episode?
Background. The goal of the Acute Care Episode (ACE) demonstration was to use a bundled payment to better align the incentives for both hospitals and physicians, leading to better quality and greater efficiency in the care that is delivered.
What is a criterion for a patient to be admitted to the long-term acute care hospital?
Long-Term Acute Care Hospital (LTACH) Care provided by an LTACH is hospital-based care, and, as such, admission requires documentation that patients have a complicated course of recovery that requires prolonged hospitalization.
What does Medicare Part B cover?
Part B also covers durable medical equipment, home health care, and some preventive services.
Does Medicare cover tests?
Medicare coverage for many tests, items, and services depends on where you live . This list includes tests, items, and services (covered and non-covered) if coverage is the same no matter where you live.
What is Medicare Part A?
Medicare Part A (Hospital Insurance) Part A covers inpatient hospital stays, care in a skilled nursing facility, hospice care, and some home health care. covers the cost of long-term care in a. long-term care hospital. Acute care hospitals that provide treatment for patients who stay, on average, more than 25 days.
How long does an acute care hospital stay?
Acute care hospitals that provide treatment for patients who stay, on average, more than 25 days. Most patients are transferred from an intensive or critical care unit. Services provided include comprehensive rehabilitation, respiratory therapy, head trauma treatment, and pain management. .
How long does it take to get discharged from a long term care hospital?
You’re transferred to a long-term care hospital directly from an acute care hospital. You’re admitted to a long-term care hospital within 60 days of being discharged from a hospital.
Do you have to pay a deductible for long term care?
Each day after the lifetime reserve days: All costs. *You don’t have to pay a deductible for care you get in the long-term care hospital if you were already charged a deductible for care you got in a prior hospitalization within the same benefit period.
What is national coverage?
National coverage decisions made by Medicare about whether something is covered. Local coverage decisions made by companies in each state that process claims for Medicare. These companies decide whether something is medically necessary and should be covered in their area.
Is Medicare Advantage the same as Original Medicare?
What's covered? Note. If you're in a Medicare Advantage Plan or other Medicare plan, your plan may have different rules. But, your plan must give you at least the same coverage as Original Medicare. Some services may only be covered in certain settings or for patients with certain conditions.
What are Medicare covered services?
Medicare-covered hospital services include: Semi-private rooms. Meals. General nursing. Drugs as part of your inpatient treatment (including methadone to treat an opioid use disorder) Other hospital services and supplies as part of your inpatient treatment.
What does Medicare Part B cover?
If you also have Part B, it generally covers 80% of the Medicare-approved amount for doctor’s services you get while you’re in a hospital. This doesn't include: Private-duty nursing. Private room (unless Medically necessary ) Television and phone in your room (if there's a separate charge for these items)
What is an inpatient hospital?
Inpatient hospital care. You’re admitted to the hospital as an inpatient after an official doctor’s order, which says you need inpatient hospital care to treat your illness or injury. The hospital accepts Medicare.
How many days in a lifetime is mental health care?
Things to know. Inpatient mental health care in a psychiatric hospital is limited to 190 days in a lifetime.
What facilities does Medicare Part A cover?
Some of the facilities that Medicare Part A benefits apply to include: hospital. acute care or inpatient rehabilitation facility. skilled nursing facility. hospice. If you have Medicare Advantage (Part C) instead of original Medicare, your benefit periods may differ from those in Medicare Part A.
How long does Medicare Advantage last?
Takeaway. Medicare benefit periods usually involve Part A (hospital care). A period begins with an inpatient stay and ends after you’ve been out of the facility for at least 60 days.
How much coinsurance do you pay for inpatient care?
Days 1 through 60. For the first 60 days that you’re an inpatient, you’ll pay $0 coinsurance during this benefit period. Days 61 through 90. During this period, you’ll pay a $371 daily coinsurance cost for your care. Day 91 and up. After 90 days, you’ll start to use your lifetime reserve days.
How long does Medicare benefit last after discharge?
Then, when you haven’t been in the hospital or a skilled nursing facility for at least 60 days after being discharged, the benefit period ends. Keep reading to learn more about Medicare benefit periods and how they affect the amount you’ll pay for inpatient care. Share on Pinterest.
What is Medicare benefit period?
Medicare benefit periods mostly pertain to Part A , which is the part of original Medicare that covers hospital and skilled nursing facility care. Medicare defines benefit periods to help you identify your portion of the costs. This amount is based on the length of your stay.
How much is Medicare deductible for 2021?
Here’s what you’ll pay in 2021: Initial deductible. Your deductible during each benefit period is $1,484. After you pay this amount, Medicare starts covering the costs. Days 1 through 60.
How long can you be out of an inpatient facility?
When you’ve been out of an inpatient facility for at least 60 days , you’ll start a new benefit period. An unlimited number of benefit periods can occur within a year and within your lifetime. Medicare Advantage policies have different rules entirely for their benefit periods and costs.
What is subacute care?
The goal of subacute care is to get you back to functioning at the level you did before entering care. You might still need more therapy or home health care when you are done with SAR. Examples of issues that might call for subacute care are: Hip replacement. Fall.
How long does a hospital stay in Part A?
A benefit period in Part A begins the day you’re admitted into the hospital and ends when you haven’t had any inpatient hospital or skilled nursing facility care for 60 days in a row.
How much is Medicare deductible for mental health?
After 90 days, the coinsurance rate is $742 per day. The same cost plan goes for mental health inpatient stays, while you will also pay 20% of the Medicare-approved amount for mental health services while an inpatient. For mental health inpatient stays, there’s no limit to the number of benefit periods you can have, but there is a lifetime limit of 190 days.
How long does a diabetic stay in a hospital?
Subacute care usually provides around three hours of therapy in a day, and the stay can last for a few days up to 100 days.
How long can you stay in a mental hospital?
For mental health inpatient stays, there’s no limit to the number of benefit periods you can have, but there is a lifetime limit of 190 days.
Does long term care insurance cover SNF?
Long-term care insurance may help pay for SNF stay after your coverage period has ended. After you’ve been out of the facility for 60 days, a new coverage period begins and you’ll be covered for 100 more days of care if needed after a three-day qualifying inpatient stay.
