If you qualify for Extra Help, you won't pay a late enrollment penalty when you join a Medicare drug plan. If you get Extra Help but you’re not sure if you're paying the right amount, call your drug plan. Your plan may ask you to give information to help them check the level of Extra Help you should get.
Full Answer
Do I have to pay a late enrollment penalty for Medicare?
If you qualify for Extra Help, you won't pay a late enrollment penalty when you join a Medicare drug plan. If you get Extra Help but you’re not sure if you're paying the right amount, call your drug plan.
How do I get extra help with Medicare extra help?
Your plan may ask you to give information to help them check the level of Extra Help you should get. Examples of documents you can send your plan include: A purple notice from Medicare that says you automatically qualify for Extra Help.
How does extra help work with Medicare Part D?
A program called Extra Help offsets the cost of prescriptions for Medicare beneficiaries with Part D. If you have limited resources, you might qualify. We’re here to help you understand how Extra Help works with Part D, who’s eligible, how to apply, and more.
Can I make changes to my Medicare plan after October 15?
You’ll have to wait for the next period to make another change. You can’t use this Special Enrollment Period from October–December. However, all people with Medicare can make changes to their coverage from October 15–December 7, and the changes will take effect on January 1.

How do I get rid of Medicare late enrollment penalty?
3 ways to avoid the Part D late enrollment penaltyEnroll in Medicare drug coverage when you're first eligible. ... Enroll in Medicare drug coverage if you lose other creditable coverage. ... Keep records showing when you had other creditable drug coverage, and tell your plan when they ask about it.
How do you qualify to get $144 back from Medicare?
How do I qualify for the giveback?Are enrolled in Part A and Part B.Do not rely on government or other assistance for your Part B premium.Live in the zip code service area of a plan that offers this program.Enroll in an MA plan that provides a giveback benefit.
What happens if I miss the Medicare enrollment deadline?
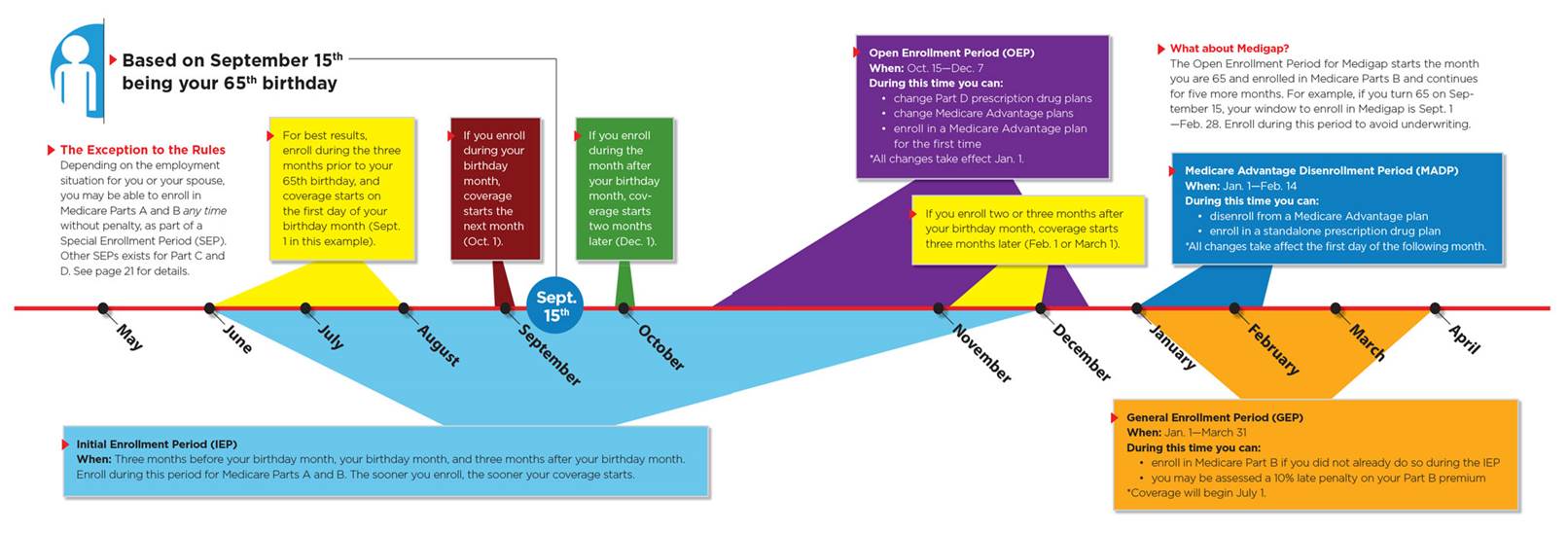
If you missed your Initial Enrollment Period (IEP) and need to enroll in Medicare, you likely will have to enroll during either a Special Enrollment Period (SEP) or the General Enrollment Period (GEP).
Can I be charged extra if I don't enroll in Medicare?
Medicare Part A late-enrollment penalty If you don't enroll when you're first eligible for Medicare, you can be subject to a late-enrollment penalty, which is added to the Medicare Part A premium. The penalty is 10% of your monthly premium, and it applies regardless of the length of the delay.
Who is eligible for Medicare Part B reimbursement?
1. How do I know if I am eligible for Part B reimbursement? You must be a retired member or qualified survivor who is receiving a pension and is eligible for a health subsidy, and enrolled in both Medicare Parts A and B.
What is the Medicare Give Back Program?
The Medicare Part B give back is a benefit specific to some Medicare Advantage Plans. This benefit covers up to the entire Medicare Part B premium amount for the policyholder. The give back benefit can be a great way for beneficiaries to save, as the premium is deducted from their Social Security checks each month.
What happens if someone misses their opportunity to enroll in Medicare during their initial enrollment period or special enrollment period?
A Special Enrollment Period is only available for a limited time. If you don't sign up during your Special Enrollment Period, you'll have to wait for the next General Enrollment Period and you might have to pay a monthly late enrollment penalty.
Can you add Medicare Part B at any time?
You can sign up for Medicare Part B at any time that you have coverage through current or active employment. Or you can sign up for Medicare during the eight-month Special Enrollment Period that starts when your employer or union group coverage ends or you stop working (whichever happens first).
What is the Part B late enrollment penalty?
If you didn't get Part B when you're first eligible, your monthly premium may go up 10% for each 12-month period you could've had Part B, but didn't sign up. In most cases, you'll have to pay this penalty each time you pay your premiums, for as long as you have Part B.
Is there a grace period for Medicare premiums?
Under rules issued by the Centers for Medicare and Medicaid Services (CMS), consumers will get a 90-day grace period to pay their outstanding premiums before insurers are permitted to drop their coverage.
Can you add Medicare Part D at any time?
Keep in mind, you can enroll only during certain times: Initial enrollment period, the seven-month period that begins on the first day of the month three months before the month you turn 65 and lasts for three months after the birthday month.
How is the Medicare Part B penalty calculated?
The Medicare Part B penalty increases your monthly Medicare Part B premium by 10% for each full 12-month period you did not have creditable coverage. The penalty is based on the standard Medicare Part B premium, regardless of the premium amount you actually pay.
When does Medicare take effect?
January–March. April–June. July–September. If you make a change, it will take effect on the first day of the following month. You’ll have to wait for the next period to make another change. You can’t use this Special Enrollment Period from October–December. However, all people with Medicare can make changes to their coverage from October ...
How often can you change your medicaid?
If you have Medicaid or receive Extra Help, you may be able to make changes to your coverage one time during each of these periods: If you make a change, it will begin the first day of the following month. You’ll have to wait for the next period to make another change.
What are the benefits of Medicare Part D Extra Help?
Recipients who qualify for this low-income assistance can expect the following benefits: Monthly premium payment. Part D plans are carried by private insurers and the monthly premium can be different depending on the level of coverage the plan offers. You state may set a limit on the portion of ...
What are the resources that are measured against program limits?
Assets. Resources with cash value, such as savings and investment accounts or certain types of property may be measured against program limits. Some states may not have an asset limit for certain demographics.
What are the eligibility criteria for medicaid?
Medicaid eligibility criteria will typically consider the following: 1 Income. Both earned and unearned income is considered when an applicant applies for Medicaid services. There may be qualifying deductions subtracted from the total amount of income that can lower the measurable amount below any program limit. 2 Assets. Resources with cash value, such as savings and investment accounts or certain types of property may be measured against program limits. Some states may not have an asset limit for certain demographics. 3 Spend down. If an applicant’s income or resources exceed program limits, qualifying expenses may be subtracted from their measurable income or resources to bring them under their state’s program limits for eligibility.
Is there a penalty for late enrollment in Medicare?
No late enrollment penalty. Medicare recipients who delay enrollment in a Part D plan when they first become eligible may be charged a penalty for late enrollment. Extra Help eliminates this penalty. Separate Special Enrollment Period (SEP).
Do Medicare beneficiaries get extra help?
Many qualifying Medicare beneficiaries are automatically notified if they are eligible for Extra Help in their state. This is often the case for Medicare recipients who receive retirement benefits and are no longer working.
Is Medicaid a federal program?
Medicaid is a federally funded program, but each state is in charge of administering the program for its qualifying residents. Due to changes in the cost of living in each state, eligibility for Medicaid can be different in each state.
Is Extra Help a Part D plan?
Extra Help is not a prescription drug plan separate from Part D, it is simply a way that Medicare-Medical dual-eligibles can receive extra assistance in paying for their Part D plan and any prescription medications they require.
What to do if you disagree with Medicare decision?
If you disagree with the decision we made about your eligibility for Extra Help, complete an Appeal of Determination for Extra Help with Medicare Prescription Drug Plan Costs. We also provide Instructions for Completing the Appeal.
Do you have to review your eligibility for extra help?
If you are already receiving Extra Help, we must review your eligibility periodically. We’ll ask you to complete the Review of Your Eligibility for Extra Help (SSA-1026B) to ensure you’re still eligible for Extra Help and receiving all the benefits you deserve.
Can you get help with Medicare?
With the Medicare Savings Programs (MSP), you can get help, from your state, paying your Medicare premiums. In some cases, MSPs may also pay Medicare Part A (hospital insurance) and Medicare Part B (medical insurance) deductibles, coinsurance, and copayments if you meet certain conditions. If you qualify for certain MSPs, you automatically qualify ...
Can Medicare beneficiaries get extra help?
Table of Contents. Medicare beneficiaries can qualify for Extra Help paying for their monthly premiums, annual deductibles, and co-payments related to Medicare Part D (prescription drug coverage).
What is extra help?
Extra Help is a program to help people with limited income and resources pay Medicare prescription drug program costs, like premiums, deductibles, and coinsurance. If you get Extra Help but you’re not sure if you're paying the right amount, call your drug plan.
What are some examples of documents you can send to Medicare?
Examples of documents you can send your plan include: A purple notice from Medicare that says you automatically qualify for Extra Help. A yellow or green automatic enrollment notice from Medicare. An Extra Help "Notice of Award" from Social Security. An orange notice from Medicare that says your copayment amount will change next year.
How much does a prescription cost for 2021?
Make sure you pay no more than the LIS drug coverage cost limit. In 2021, prescription costs are no more than $3.70 for each generic/$9.20 for each brand-name covered drug for those enrolled in the program. Contact Medicare so we can get confirmation that you qualify, if it's available.
How long does Medicaid pay for stay?
Or, a copy of a state document showing Medicaid paid for your stay for at least a month. A print-out from your state’s Medicaid system showing you lived in the institution for at least a month. A document from your state that shows you have Medicaid and are getting home- and community-based services.
What is a bill from a nursing home?
A bill from an institution (like a nursing home). Or, a copy of a state document showing Medicaid paid for your stay for at least a month.
What is an orange notice from Medicare?
An orange notice from Medicare that says your copayment amount will change next year. If you have. Supplemental Security Income (Ssi) A monthly benefit paid by Social Security to people with limited income and resources who are disabled, blind, or age 65 or older.
What is a copy of a medicaid card?
A copy of your Medicaid card (if you have one). A copy of a state document that shows you have Medicaid. A print-out from a state electronic enrollment file that shows you have Medicaid. A screen print from your state's Medicaid systems that shows you have Medicaid.
What is the extra help program?
If you have difficulty paying for prescriptions, the Extra Help program – also known as the Low-Income Subsidy (LIS) – can make prescriptions and plan premiums more affordable than they would be with Medicare Part D alone.
How much will Social Security extra help be in 2021?
Enrollees who receive Extra Help in 2021 will pay no more than $3.70 for each generic drug and $9.20 for brand-name drugs. This is a valuable benefit that the Social Security Administration estimates is worth an average of about $5,000 per year.
Do you get extra help if you have Medicare?
Your income and resources determine the level of help you receive. You’ll automatically receive Extra Help if you have both Medicare and Medicaid, a Medicare Savings Program, or Supplemental Security Income, or Medicare only but also a limited income (note that the levels of Extra Help are different depending on your eligibility category).
Does Part D help with deductible?
Some beneficiaries, with income on the higher end of the eligible range, receive partial Extra Help, which reduces — but does not fully cover — the premiums and deductible for Part D. Partial Extra Help also reduces other out-of-pocket costs under Part D, but not as much as full Extra Help.
What is extra help for Medicare?
Are you a Medicare beneficiary struggling with the cost of prescription drugs? A program called Extra Help offsets the cost of prescriptions for Medicare beneficiaries with Part D . If you have limited resources, you might qualify. We’re here to help you understand how Extra Help works with Part D, who’s eligible, how to apply, and more.
How to apply for extra help?
To apply for Extra Help, you can fill out Form SSA-1020 on the Social Security website. You can also call Social Security to apply over the phone or visit your local Social Security office to apply in person.
How much does extra help save?
On average, Extra Help is estimated to save beneficiaries $5,000 in these costs per year. If you’re eligible for Medicaid or any of the following Medicare Savings Programs, you automatically qualify for Extra Help. Qualified Medicare Beneficiary (QMB)
What is extra help?
The Extra Help program assists people with limited resources and lower incomes in paying for Part D prescription drug coverage.
How much does a generic prescription cost?
For those enrolled in Extra Help, generic prescription costs are no more than $3.60 each, and brand-name prescription costs are no more than $8.95 each. If you didn’t enroll in Part D when you first became eligible, you won’t have to pay the late enrollment penalty if you have Extra Help.
What is the income limit for extra help in 2021?
What Are the Income and Resource Limits for Extra Help in 2021? In 2021, the annual income limit for Extra Help for an individual is $19,140. For a married couple who is living together, the limit is $25,860. When your income is calculated, governmental assistance such as food stamps, housing assistance, and home energy assistance aren’t counted.
How often is your unemployment eligibility reviewed?
Your eligibility will be reviewed automatically every year and you’ll receive a notice that states if you still qualify or not.