Certification is an optional process that allows providers to bill Medicare or Medicaid Medicaid in the United States is a federal and state program that helps with medical costs for some people with limited income and resources. Medicaid also offers benefits not normally covered by Medicare, including nursing home care and personal care services. The Health Insurance As…Medicaid
What are the requirements for Medicare certification?
- The date the plan of care being sent for certification becomes effective (the initial evaluation date is acceptable)
- Diagnoses
- Long term treatment goals
- Type, amount, duration and frequency of therapy services
- Signature, date and professional identity of the therapist who established the plan
What does it mean to be Medicare certified?
- Ambulatory Surgical Centers (ASC)
- Comprehensive Outpatient Rehabilitation Facilities (CORF)
- End-Stage Renal Dialysis (ESRD)
- Home Health Agencies (HHA) For more information about HHA Certification, please see Request Home Health Agency (HHA) Medicare certification
- Hospices
- Hospitals
- Laboratories (CLIA)
- Nursing Homes
How to get Medicare certified?
- Ambulatory surgery centers
- Community mental health centers
- Comprehensive outpatient rehabilitation facilities
- Critical access hospitals
- End-stage renal disease facilities
- Home health agencies
- Home infusion therapy suppliers
- Hospices
- Hospitals
- Intermediate care facilities for individuals with intellectual disabilities
How does Medicare impact certification?
Impact of Medicare on Licensure, Certification, or Accreditation The US medical system requires healthcare facilities and professionals to apply for licensing before offering medical services. The issuance of licenses depends on compliance with state laws and federal regulations (American Health Lawyer Association, 2013).
What is Medicare certified mean?
Medicare-certified means offering services at a level of quality approved by Medicare. Medicare will not pay for services received from a health care provider that is not Medicare-certified.
What is a CMS certificate?
The CMS Certification number (CCN) replaces the term Medicare Provider Number, Medicare Identification Number or OSCAR Number. The CCN is used to verify Medicare/Medicaid certification for survey and certification, assessment-related activities and communications. The RO assigns the CCN and maintains adequate controls.
How long is AHIP certification good for?
How long does my AHIP certification last? You must re-certify with AHIP each year. You can recertify via a carrier link for the discounted $125 rate as long as you are an agent in good standing.
Is accreditation mandatory for Medicare?
Accreditation by an AO is voluntary and is not required for Medicare certification or participation in the Medicare Program. A provider's or supplier's ability to bill Medicare for covered services is not impacted if it chooses to discontinue accreditation from a CMS-approved AO or change AOs.
Is NPI same as CMS certification number?
The NPI is the National Provider Identifier, and is a unique identification number provided to facilities and other medical entities. The Medicare Provider Number is also known as the CCN (CMS Certification Number). This is the six-digit Medicare certification number for a facility.
How do I find my CMS certification number?
Go to the CMS website. You can find all the resources needed to obtain your CMS Certification Number at this link: https://www.cms.gov/Medicare/Provider-Enrollment-and-Certification/MedicareProviderSupEnroll/EnrollmentApplications.html.
How difficult is the AHIP test?
Many returning Medicare agents say AHIP is easy — once you get the hang of it. Nobody's perfect, especially when learning something new! If you get more questions incorrect than you thought you would, or if you fail your first time taking the final AHIP exam, don't fret. Just study up on those areas a little more.
How much does AHIP cost?
We didn't mention it yet, but AHIP isn't free. Typically, the AHIP certification test costs $175, but many carriers offer a discounted rate of $125 if you take the exam through their agent portals.
What is the pass rate of AHIP?
What is the AHIP exam like? The AHIP exam is 50 questions. Brokers have two hours to complete it, and they may print the AHIP training modules to use for the test. A passing score is 90% or higher.
What are benefits of accreditation?
The 5 Top Benefits of AccreditationAccreditation improves patient outcomes and mitigates risks. ... Accreditation identifies strengths and gaps in your programs and processes. ... Accreditation promotes communication and staff empowerment across organizations. ... Accreditation fosters a culture of quality and safety.More items...•
Why is CMS accreditation important?
Achieving accreditation status from The Joint Commission ensures your facility also meets CMS standards. Both The Joint Commission and CMS adhere to requirements that continuously aim to improve health care for the public by assuring organizations are providing safe and effective care of the highest quality and value.
What is the accrediting and certifying organizations for acute care hospitals?
The Accreditation Commission for Health Care.
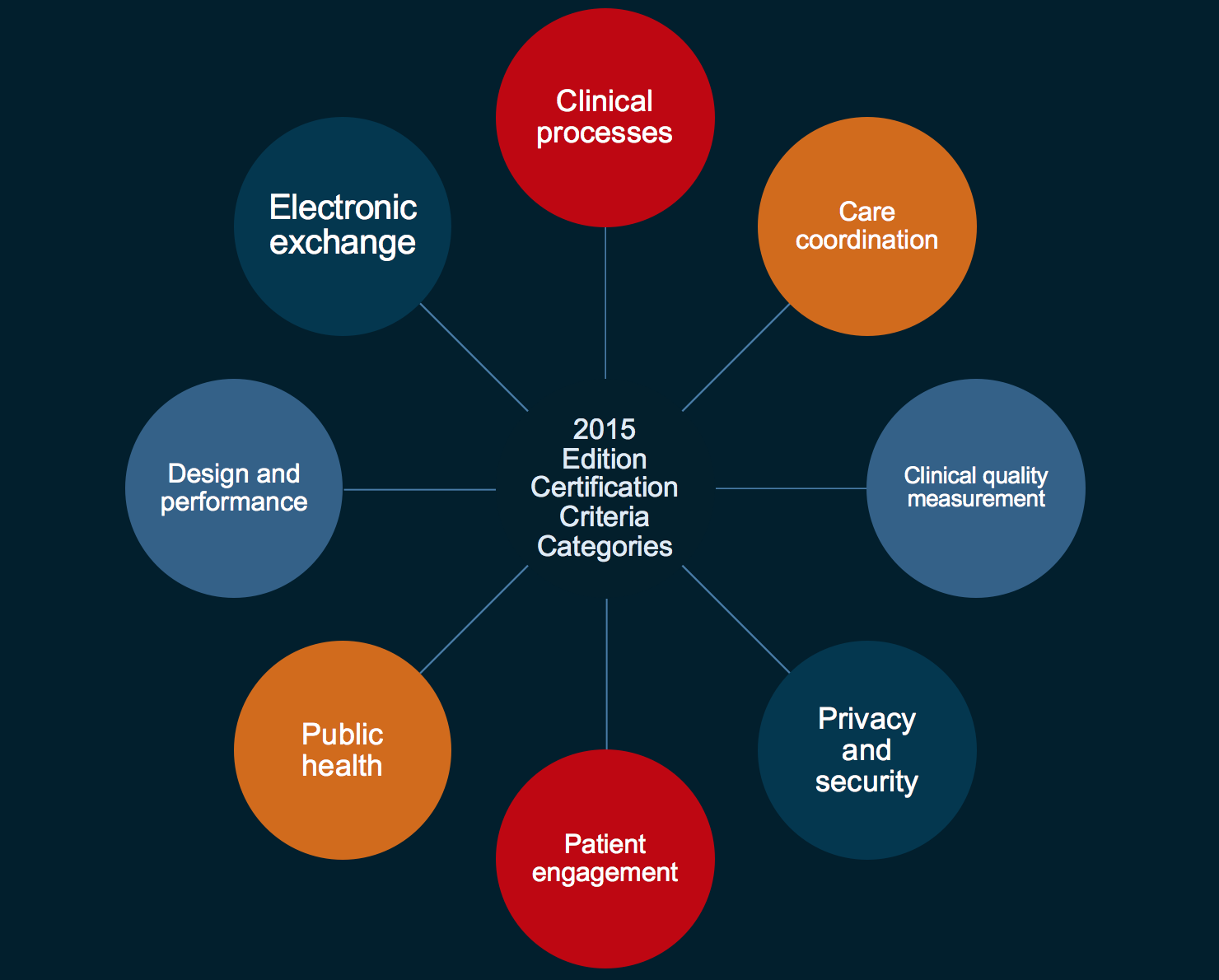
Health care facilities and programs
Health care facilities and programs must be certified to participate in the Medicare and Medicaid programs. The Division of Health Care Facility Licensure and Certification is the CMS State Survey Agency for the following provider programs:
Individual providers seeking medicare certification
If you are an individual provider such as a doctor or dentist that is operating as a practice rather than a licensed clinic, and are seeking Medicare certification, please contact the Medicare Provider Line at (877) 869-6504.
What is AO in Medicare?
Section 1865 (a) (1) of the Social Security Act (the Act) permits providers and suppliers "accredited" by an approved national accreditation organization (AO) to be exempt from routine surveys by State survey agencies to determine compliance with Medicare conditions.
Is AO required for Medicare?
Accreditation by an AO is voluntary and is not required for Medicare certification or participation in the Medicare Program. A provider’s or supplier’s ability to bill Medicare for covered services is not impacted if it chooses to discontinue accreditation from a CMS-approved AO or change AOs.
What is Medicare insurance?
Medicare is a Federal insurance program providing a wide range of benefits for specific periods of time through providers and suppliers participating in the program. The Act designates those providers and suppliers that are subject to Federal health care quality standards.
What is Medicare Code?
Medicare is a Federal insurance program providing a wide range of benefits for specific periods of time through providers ...
What is the Social Security Act?
The Social Security Act (the Act) mandates the establishment of minimum health and safety and CLIA standards that must be met by providers and suppliers participating in the Medicare and Medicaid programs. These standards are found in the 42 Code of Federal Regulations. The Secretary of the Department of Health and Human Services has designated CMS ...
What are the types of institutions that participate in Medicaid?
In general, the only types of institutions participating solely in Medicaid are (unskilled) Nursing Facilities, Psychiatric Residential Treatment Facilities, and Intermediate Care Facilities for the Mentally Retarded.
What is Medicaid in the US?
Medicaid is a State program that provides medical services to clients of the State public assistance program and, at the State's option, other needy individuals. When services are furnished through institutions that must be certified for Medicare, the institutional standards must be met for Medicaid as well.
When was the Clinical Laboratory Improvement Amendments passed?
Congress passed the Clinical Laboratory Improvement Amendments (CLIA) in 1988 establishing quality standards for all laboratories testing to ensure the accuracy, reliability, and timeliness of patient test results, regardless of where the test was performed.
Does Medicaid require nursing facilities to meet the same requirements as skilled nursing facilities?
Medicaid requires Nursing Facilities to meet virtually the same requirements that Skilled Nursing Facilities participating in Medicare must meet. Intermediate Care Facilities for the Mentally Retarded must comply with special Medicaid standards.
What is a certification for Medicare?
Certification is an optional process that allows providers to bill Medicare or Medicaid for re-imbursement. Most types of facilities are eligible for Medicare and Medicaid. Some are eligible for Medicaid only.The process can be confusing, and we are here to help.Certification starts with a letter of intent.
What is HCPF certification?
HCPF Medicaid certification requirements. Facilities subject to Medicaid certification through the state’s Department of Health Care Policy and Financing (HCPF) must meet that department's Volume 8 regulations. HCPF reimburses providers for Medicaid client services, but delegates the inspection/survey functions to us.
How long is a Medicare certification?
The length of the certification period is the duration of treatment, e.g. 2x/week for 8 weeks. In this example the end date of the certification period is 8 weeks, to the day, from the initial evaluation date. In 2008 Medicare changed the requirement for the maximum duration of each plan of care. The maximum length of time any certification period ...
How long can a Medicare plan of care be certified?
The maximum length of time any certification period used to be 30 days, however now it can run up to 90 days.
What happens if you don't comply with Medicare?
If, in the course of the audit, they find you do not have the Certifications/Re-certifications, if appropriate, included in the chart they can deem your care for that patient as not meeting the medical necessity or the requirement to be under a physician’s care. In that case Medicare can decide that all the care for these patients should not have been carried out and can ask for all payments plus interest and a penalty to be returned to them. This can come to a significant amount of money, especially if it occurs in a number of patient’s charts.
Can Medicare ask for all payments plus interest?
In that case Medicare can decide that all the care for these patients should not have been carried out and can ask for all payments plus interest and a penalty to be returned to them. This can come to a significant amount of money, especially if it occurs in a number of patient’s charts.
Does a referral count as a POC?
CMS considers a referral from a physician/non-physician provider (NPP) or the Plan of Care (POC) as the best ways to demonstrate physician involvement. However these are not interchangeable. A referral by itself from a physician may not meet the requirements of a certifiable Plan of Care. It can only count as the certification ...
What is a Medicare certification letter?
Medicare certification letter is issued by a central insurance program to provide great range of reimbursement for definite periods of time. In the terminology of Medicare, providers are normally patient care institutions such as medical centers, hospitals, nursing homes, and other health agencies providing services at home.
What is a supplier in Medicare?
Suppliers are diagnosis or therapy provides by pathology laboratori es, clinics, and ambulatory agencies. At the time of services furnished through these providers or suppliers, must be certified for Medicare. This certification letter is most likely written by a senior medical officer for a patient. It gives details of the patient’s condition.
What does a recertification statement indicate?
To meet requirements the certification or recertification statement must clearly indicate posthospital extended care services were required because of the individual's need for skilled care on a continuing basis for which he/she was receiving inpatient hospital services. The statement must be signed:
How long does it take to get a recertification?
Subsequent recertifications are required at intervals not to exceed 30 days. Delayed Certification/Recertifications. Delayed certifications and recertifications are allowed for an isolated oversight or lapse.
What is a PA in nursing?
A nurse practitioner (NP), clinic al nurse specialist (CNS) or a physician assistant (PA) who does not have a direct or indirect employment relationship with the facility, but who is working in collaboration with the physician. Timing of Certification/Recertifications.
What are the benefits of Medicare?
Here’s a short list on what will be covered: 1 The basics of Medicare fee-for-service eligibility and benefits 2 The different types of Medicare Advantage and Part D prescription drug plans 3 Eligibility and coverage 4 Nondiscrimination training 5 Marketing and enrollment under the Medicare Advantage and Part D program requirements
What is AHIP certification?
AHIP (stands for America’s Health Insurance Plans) certification is accepted by all and required by most carriers if you want to legally sell Medicare Advantage (MA) or Prescription Drug Plans (PDPs) for the current certification year. Be aware that while most carriers will require AHIP certification, it will only serve as a pre-requisite ...
