Overall, switching from Medicaid FFS to Medicaid MC was associated with a significant decrease in ambulatory visits and providers compared with changes over time in both control groups. The largest decreases in ambulatory visits and providers were seen in the subset of “switchers” with 5 or more chronic conditions.
Full Answer
What is the Centers for Medicare&Medicaid Services (CMS)?
The Centers for Medicare & Medicaid Services (CMS) administers Medicare and Medicaid along with other Federal health care programs and services. This booklet provides an overview of the Medicare and Medicaid Programs and some brief information on other types of health coverage.
Does Medicare Part B cover ambulance transportation?
Part B covers certain doctors' services, outpatient care, medical supplies, and preventive services. Medicare may pay for emergency ambulance transportation in an airplane or helicopter if you need immediate and rapid transport that ground transportation can’t provide.
Does Medicaid pay for ambulance services?
The patient must be transported in an appropriate vehicle that has been inspected and issued a permit by the state. Medicaid covers non-emergency ambulance services with a statement by a doctor that the service is required.
Do Medicare and Medicaid increase health care utilization?
But it is unclear whether the expansion of health care utilization in the first few years of Medicare and Medicaid could be attributed mostly to increasing access to and utilization of needed services or to unregulated overuse of health care.

Why is Centers for Medicare and Medicaid Services Important?
The Centers for Medicare and Medicaid Services (CMS) provides health coverage to more than 100 million people through Medicare, Medicaid, the Children's Health Insurance Program, and the Health Insurance Marketplace.
What impact did Medicare and Medicaid have on society?
Medicare and Medicaid have greatly reduced the number of uninsured Americans and have become the standard bearers for quality and innovation in American health care. Fifty years later, no other program has changed the lives of Americans more than Medicare and Medicaid.
What are three factors that impact your access to healthcare services?
They include poverty and its correlates, geographic area of residence, race and ethnicity, sex, age, language spoken, and disability status. The ability to access care—including whether it is available, timely and convenient, and affordable—affects health care utilization.
How does Medicare influence patient access to care?
February 03, 2021 - Medicare coverage increases seniors' access to care and reduces affordability barriers, a study published in Health Affairs discovered. “The Medicare program pays for roughly one of every four physician visits in the United States, and in 2019 it covered roughly 60 million people.
What role does Medicare and Medicaid play in meeting the health care needs of the American public?
Medicare and Medicaid are two government programs that provide medical and other health-related services to specific individuals in the United States. Medicaid is a social welfare or social protection program, while Medicare is a social insurance program.
How does Medicare impact health and wellbeing?
Medicare also helps with the cost of seeing a local doctor or specialist and with paying for medicine and other treatment. It also delivers free public hospital care. You can purchase health insurance to cover costs not refunded by Medicare or cover the costs of private hospitalisation.
How does service availability affect access to care?
Limited availability of health care resources is another barrier that may reduce access to health services3 and increase the risk of poor health outcomes. For example, physician shortages may mean that patients experience longer wait times and delayed care.
What are some key barriers to accessing health care?
Below, PatientEngagementHIT.com outlines some of the top obstacles to patient care access, as well as the ways some medical professionals are addressing them.Limited appointment availability, office hours.Geographic, clinician shortage issues.Transportation barriers.Limited education about care sites.More items...•
Why is Patient Access important in healthcare?
Patient access is the first point of contact for patients and the first time staff can get key information right for revenue cycle management success. May 06, 2021 - Patient access is generally the first encounter a patient will have with a healthcare organization, making it central to the patient experience.
How did the ACA improve access to healthcare?
Since then, the law has transformed the American health care system by expanding health coverage to 20 million Americans and saving thousands of lives. The ACA codified protections for people with preexisting conditions and eliminated patient cost sharing for high-value preventive services.
What groups of individuals traditionally lack access to health care in the United States and why?
Age Of The Uninsured Working-age adults made up a much larger share of the uninsured population than any other age group. In fact, most uninsured people (84.6 percent) were 19- to 64-year-olds. The two largest groups in that age range are 26- to 34-year-olds and 35- to 44-year-olds.
Does insurance affect quality care?
This study finds that overall, there is no significant difference in perceptions of quality of care between insured and uninsured patients. However, some indicators show significant differences in perceptions of quality of care, key among which is financial access to care.
Emergency Ambulance Services
Medicaid covers Emergency Ambulance services when provided by providers licensed by the state. The patient must be transported in an appropriate vehicle that has been inspected and issued a permit by the state.
Medical Transportation or Non-Emergency Ambulance Services
Medicaid covers non-emergency ambulance services with a statement by a doctor that the service is required.
What are the services covered by Medicare?
Physicians' and surgeons' services, including some covered services furnished by chiropractors, podiatrists, dentists, and optometrists. Also covered are the services provided by these Medicare-approved practitioners who are not physicians: certified registered nurse anesthetists, clinical psychologists, clinical social workers (other than in a hospital or SNF), physician assistants, and nurse practitioners and clinical nurse specialists in collaboration with a physician.
What is included in inpatient hospital care?
Inpatient hospitalcare coverage includes costs of a semi-private room, meals, regular nursing services, operating and recovery rooms, intensive care, inpatient prescription drugs, laboratory tests, X-rays, psychiatric hospitals, inpatient rehabilitation, and long-term care (LTC) hospitalization when medically necessary, as well as all other medically necessary services and supplies provided in the hospital. An initial deductible payment is required of beneficiaries who are admitted to a hospital, plus copayments for all hospital days following day 60 within a benefit period (described later).
When was Medicare and Medicaid established?
After lengthy national debate, Congress passed legislation in 1965 establishing the Medicare and Medicaid programs as Title XVIII and Title XIX, respectively, of the Social Security Act. Medicare was established in response to the specific medical care needs of the elderly (with coverage added in 1973 for certain disabled persons and certain persons with kidney disease). Medicaid was established in response to the widely perceived inadequacy of welfare medical care under public assistance. Responsibility for administering the Medicare and Medicaid programs was entrusted to the Department of Health, Education, and Welfare—the forerunner of the current DHHS. Until 1977, the Social Security Administration (SSA) managed the Medicare program, and the Social and Rehabilitation Service (SRS) managed the Medicaid program. The duties were then transferred from SSA and SRS to the newly formed HCFA.
What is an MSA plan?
Medical savings account (MSA) plans, which provide benefits after a single high deductible is met. Medicare makes an annual deposit to the MSA, and the beneficiary is expected to use the money in the MSA to pay for medical expenses below the annual deductible. MSAs are currently a test program for a limited number of eligible Medicare beneficiaries.
How is health care funded?
Health care is funded through a variety of private payers and public programs. Privately funded health care includes individuals' out-of-pocket expenditures, private health insurance, philanthropy, and non-patient revenues (such as gift shops and parking lots), as well as health services that are provided in industrial settings. For the years 1974-1991, these private funds paid for 58 to 60 percent of all health care costs. By 1997, however, the private share of health costs had declined to 53.8 percent of the country's total health care expenditures, rising slightly to 54.5 percent in 1998. The share of health care provided by public spending increased correspondingly during the 1992-1997 period, falling slightly in 1998.
Does Medicare pay for hospice care?
However, if a hospice patient requires treatment for a condition that is not related to the terminal illness, Medicare will pay for all covered services necessary for that condition. The Medicare beneficiary pays no deductible for the hospice program, but does pay small coinsurance amounts for drugs and inpatient respite care.
When was Medicare first implemented?
When first implemented in 1966, Medicare covered most persons age 65 or over. In 1973, the following groups also became eligible for Medicare benefits: persons entitled to Social Security or Railroad Retirement disability cash benefits for at least 24 months, most persons with end-stage renal disease (ESRD), and certain otherwise non-covered aged persons who elect to pay a premium for Medicare coverage.
How often do CMHCs update their assessments?
Removing a requirement for CMHCs to update the client comprehensive assessment every 30 days for all CMHC clients and only retain the minimum 30-day assessment update for those clients who receive partial hospitalization program services. We believe this will allow for an efficient use of CMHC clinician time, allowing for more time with their clients.
How often should a clinic conduct a patient care review?
Reducing the frequency of review of the patient care policies from annually to every two years, in order to allow these clinics to direct their limited resources to patient care. Facilities are always permitted to conduct reviews as they deem appropriate.
How to reduce burden on ASCs?
Reducing burden for ASCs by removing the provisions requiring ASCs to have a written transfer agreement with a hospital that meets certain Medicare requirements or ensuring that all physicians performing surgery in the ASC have admitting privileges in a hospital that meets certain Medicare requirements. This long standing requirement is now duplicative of other regulatory requirements and has been rendered obsolete by other patient protections; and
Why do we remove the requirement for transplant centers?
Removing requirements for transplant centers to re-submit clinical experience, outcomes, and other data in order to obtain Medicare approval. CMS proposes to remove this requirement in order to address unintended consequences of existing requirements , which have resulted in transplant programs potentially avoiding performing transplant procedures on certain patients and many organs going unused. We will continue to monitor and assess outcomes and quality of care in transplant programs after initial Medicare approval.
What is the purpose of updating the terminology and proposed nomenclature change used in the regulations?
Updating the terminology and proposed nomenclature change used in the regulations to conform to the terminology that is widely used and understood within the transplant community, thereby reducing provider confusion; and
How often should an emergency program be reviewed?
Emergency program: Give facilities the flexibility to review their emergency program every two years, or more often at their own discretion, in order to best address their individual needs. A comprehensive review of the program can involve an extensive process that may not yield significant change over the course of one year. Facilities may review the plan more frequently should significant changes become necessary as determined by the individual needs of the facility. The combination of all Emergency Preparedness requirements (policies and procedures, testing, communication plan) will continue to hold facilities accountable for their outcomes while allowing them more time to focus on their unique needs and specific circumstances
How often should a utilization review plan be implemented?
Implementing a proposed decrease in the frequency and implementation of a utilization review plan from four times per year to annually. This effort would allow for an entire year to collect and analyze data to inform changes to the facility and services it provides.
How did Medicare and Medicaid influence clinical medicine?
Medicare and Medicaid emerged from a fierce political process in 1965 with the charge to stay away from clinical medicine. Early on, however, Federal administrators recognized that Medicare and Medicaid could not control costs or ensure quality without regulation. As regulation developed, it took several years for the Federal Government to adopt the strategy of prospective quality improvement through partnership with the medical community. This strategy has much promise for improving medical care.
How does CMS influence medicine?
Notwithstanding what Congress wrote in 1965, the Medicare and Medicaid Programs have enormous influence over the practice of medicine. The evolution of medical care, its financing, and the expectations of the American population for high-quality care and rational use of public funds have linked, irreversibly, CMS to clinical medicine.1CMS finances health care for more Americans than any other single entity; the agency has a responsibility to its beneficiaries to ensure that they receive quality, effective, and efficient health care. As with other payers, CMS must answer to both the beneficiaries it serves and the investors (taxpayers); in addition, CMS must address the concerns of an array of political constituents, including Congress, presidential administrations, and groups representing the health care industry. To balance these competing interests and pursue evolving policy goals, CMS has had no choice but to become engaged in the practice of medicine and the delivery of health care services.
How can CMS help in clinical medicine?
First, CMS must successfully implement the Medicare Modernization Act (MMA). Second, CMS should devote more resources toward understanding the appropriate role for the Medicaid Program and how the Nation finances care for the most vulnerable segments of society. The States have conducted many experiments with payment and disease management, and CMS should facilitate sharing the lessons learned. Third, CMS should improve and develop close collaboration with other private insurers to enable the pooling of data and cooperative improvement of care. And fourth, CMS can lead by changing the paradigm of financing medical care based on acute care to one that pays for chronic illness care.
What was the role of CMS in the 1980s?
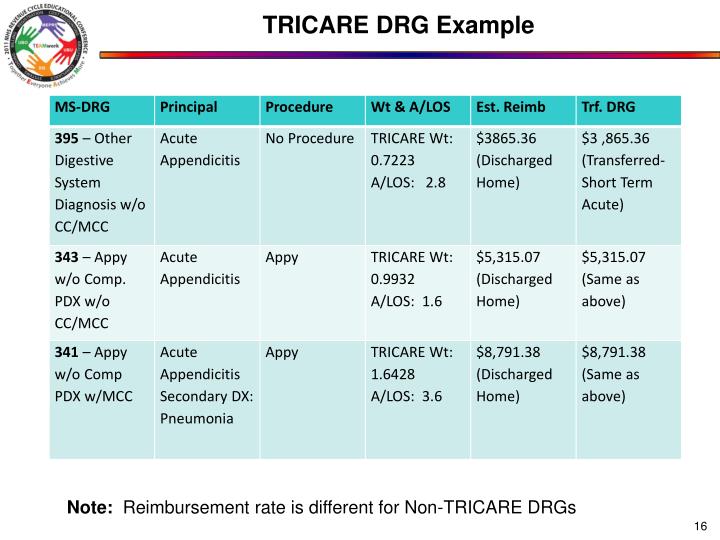
By the early 1980s, continued frustration with rising program costs led to the development of new payment and monitoring systems that expanded CMS' regulatory authority and influence. A key response to escalating costs was to change regulatory tools, both in terms of payment and clinical oversight. This change was spurred by congressional action in slowing Medicare spending in the context of rising budget deficits. The prospective payment system (PPS), enacted by Congress in 1983, sought to control hospitalization costs by paying hospitals a fixed rate based on the patient's diagnosis during admission (payment was based on diagnosis-related groups) (Social Security Amendments of 1983) (Public Law 98-21). Prior to prospective payment, hospitals and physicians did not have strong financial incentives to provide efficient care. By implementing this strategy, CMS attempted to relate clinical compensation to the resources needed for patient care. The PPS provided a strong incentive for hospitals to provide fewer services during an admission and shorten the length of stay. The role of CMS as regulatory agency became even more important: it had to monitor for both overuse and underuse of appropriate medical care. With the evolving role of these entities, the PSROs were remodeled into the peer review organizations (PROs) (Bhatia et al., 2000).
What is ESRD in Medicare?
The ESRD program is the only disease-specific coverage ever offered by Medicare . The medical procedure enabling chronic hemodialysis was invented in 1960 and pressure soon grew for Federal funding to insure access to the life-saving treatment; the National Kidney Foundation and a small group of physician kidney specialists spearheaded the lobbying campaign. ESRD was added to Medicare (along with eligibility for disabled persons) in 1972, part of congressional horse trading that gave Senator Long, (Democrat-Louisiana), ESRD in place of the Medicare drug benefit that he had sought to enact. Long advocated catastrophic health insurance as an alternative to comprehensive national health insurance, and saw ESRD as a demonstration of (and prelude to) a universal coverage system based on catastrophic insurance (Nissenson and Rettig, 1999; Schreiner, 2000; and Oberlander, 2003). When national health insurance, through catastrophic coverage or any other model, failed to materialize, ESRD remained in Medicare as the Federal Government's only universal, disease-specific coverage program.
What was the original intent of Medicare and Medicaid?
Despite the original intent, Medicare and Medicaid have had tremendous influence on medical practice. In this article, we focus on four policy areas that illustrate the influence of CMS (and its predecessor agencies) on medical practice. We discuss the implications of the relationship between CMS and clinical medicine and how this relationship has changed over time. We conclude with thoughts about potential future efforts at CMS.
How does CMS improve quality of care?
We anticipate that CMS will continue its role to improve health care quality by informing clinical care with data, taking a larger role in chronic disease management, and developing new systems that reward high quality care. Data technology will now allow analysis of close to real-time data and linkage of inpatient, outpatient, and pharmacy databases to facilitate more rapid cycles in quality improvement. CMS' most recent initiative for the QIOs will actively help physician practices to adopt electronic health records (Medicare News, 2005). In addition to the inpatient efforts noted, CMS also participates with the Ambulatory Care Quality Alliance, along with other insurers and major physician organizations, to advance quality in outpatient care settings. And CMS has embarked on large-scale demonstration projects to determine whether pay-for-performance and disease management programs can save money and improve quality. All these programs reflect the growing partnerships between CMS and hospitals and physician organizations. It has taken almost 40 years to develop these types of relationships across American health care, but such partnerships now have the potential to yield substantial benefits in the health care system.
Why is CMS important?
CMS is committed to ensuring consumers have the information they need to make fully informed decisions regarding their health care. Hospital price transparency helps Americans know what a hospital charges for the items and services it provides. CMS expects hospitals to comply with these legal requirements, and is enforcing these rules to ensure Americans know what a hospital charges for items and services.
How long is the hospital market basket update?
In the CY 2019 OPPS/ASC final rule with comment period, we finalized our proposal to apply the hospital market basket update to ASC payment system rates for an interim period of 5 years (CY 2019 through CY 2023). Using the proposed hospital market basket, CMS is updating the ASC rates for CY 2022 by 2.3 percent. The proposed update applies to ASCs meeting relevant quality reporting requirements. This change is based on the projected hospital market basket increase of 2.5 percent with a 0.2 percentage point productivity adjustment.
How many procedures are on the ASC CPL in 2021?
Using these revised criteria, CMS added 267 surgical procedures to the ASC CPL beginning in CY 2021.
What is 340B in Medicare?
Section 340B of the Public Health Service Act (340B) allows participating hospitals and other providers to purchase certain covered outpatient drugs from manufacturers at discounted prices. In the CY 2018 OPPS/ASC final rule, CMS reexamined the appropriateness of paying the Average Sale Price (ASP) plus 6 percent for drugs acquired through the 340B Program, given that 340B hospitals acquire these drugs at steep discounts. Beginning January 1, 2018, Medicare adopted a policy to pay an adjusted amount of ASP minus 22.5 percent for certain separately payable drugs or biologicals acquired through the 340B Program.
What is CMS's clarification?
Specifically, CMS is clarifying that an online price estimator tool must provide a cost estimate to an individual that takes the individual’s insurance information into account, and that the estimate reflects the amount the hospital anticipates will be paid by the individual for the shoppable service, absent unusual or unforeseeable circumstances .
What is CMS proposing to prohibit?
Proposing to Prohibit Additional Specific Barriers to Access to the Machine-Readable File: CMS proposes to update the list of activities that present barriers to access to the machine-readable file , specifically to require that the machine-readable file is accessible to automated searches and direct downloads.
How many pass through applications are there for CY 2022?
For CY 2022, CMS received eight applications for device pass-through payments. One of these applications (the Shockwave C2 Coronary Intravascular Lithotripsy (IVL) catheter) received preliminary approval for pass-through payment status through our quarterly review process. CMS is soliciting public comment on all eight of these applications and final determinations on these applications will be made in the CY 2022 OPPS/ASC final rule.
What is the role of CMS in healthcare?
CMS implements quality initiatives to assure quality health care for Medicare Beneficiaries through accountability and public disclosure. CMS uses quality measures in its various quality initiatives that include quality improvement, pay for reporting, and public reporting.
What is FMQAI in Medicare?
The Centers for Medicare & Medicaid Services (CMS) has contracted with FMQAI to provide services for the Medication Measures Special Innovation Project. The purpose of the project is to develop measures that can be used to support quality healthcare delivery to Medicare beneficiaries. The key objectives of the project are to:
Is CMS testing quality measures?
CMS is currently testing the submission of quality measures data from Electronic Health Records for physicians and other health care professionals and will soon be testing with hospitals. Click on the "Electronic Specification" link to the left for more information.