If you’re on Medicare, your doctors will usually bill Medicare for any care you obtain. Medicare will then pay its rate directly to your doctor. Your doctor will only charge you for any copay, deductible, or coinsurance you owe.
How much did Medicare pay your doctor?
On average, doctors get about 19% of their money treating Medicare patients through copayments, deductibles, and secondary-insurance. For a $70 evaluation visit, Medicare usually pays about $49 and the patient or their private insurer covers the rest.
How do doctors get paid from Medicaid?
Medicaid pays about 61% of what Medicare pays, nationally, for outpatient physician services. The payment rate varies from state to state, of course. But if 61% is average, you can imagine how ...
How much Medicare pays doctors?
Medicare reimburses office visits at around $85 per visit [1], though precise reimbursements vary by region. At $85 per visit, a primary care physician seeing nothing but Medicare patients could expect to receive $293,760 in annual reimbursements. Subtracting out the physician’s annual overhead provides an estimate of the physician’s salary.
What does Medicaid pay doctors?
Medicaid pays for emergency and medically necessary dental work across the country. Medicaid also pays for comprehensive dental care in more than 30 states. However, others may only cover certain categories of treatments.

How do doctors get reimbursed from Medicare?
Traditional Medicare reimbursements Instead, the law states that providers must send the claim directly to Medicare. Medicare then reimburses the medical costs directly to the service provider. Usually, the insured person will not have to pay the bill for medical services upfront and then file for reimbursement.
Do doctors make money on Medicare?
On average, doctors get about 19% of their money treating Medicare patients through copayments, deductibles, and secondary-insurance. For a $70 evaluation visit, Medicare usually pays about $49 and the patient or their private insurer covers the rest.
How does a physician bill Medicare?
Payment for Medicare-covered services is based on the Medicare Physicians' Fee Schedule, not the amount a provider chooses to bill for the service. Participating providers receive 100 percent of the Medicare Allowed Amount directly from Medicare.
What percentage of the allowable fee does Medicare pay a doctor?
80 percentUnder current law, when a patient sees a physician who is a “participating provider” and accepts assignment, as most do, Medicare pays 80 percent of the fee schedule amount and the patient is responsible for the remaining 20 percent.
Why do doctors opt out of Medicare?
There are several reasons doctors opt out of Medicare. The biggest are less stress, less risk of regulation and litigation trouble, more time with patients, more free time for themselves, greater efficiency, and ultimately, higher take home pay.
Do doctors treat Medicare patients differently?
So traditional Medicare (although not Medicare Advantage plans) will probably not impinge on doctors' medical decisions any more than in the past.
Why do doctors charge more than Medicare pays?
Why is this? A: It sounds as though your doctor has stopped participating with Medicare. This means that, while she still accepts patients with Medicare coverage, she no longer is accepting “assignment,” that is, the Medicare-approved amount.
Who pays Medicare claims?
Medicare claim payments at a glanceMedicare planWho pays?*ORIGINAL MEDICARE Coverage from the federal governmentMedicare Part A: Covers hospitalizationMedicare is primary payer for Part A services Member pays the rest6 more rows•Sep 1, 2016
Can a Medicare provider refuse to bill Medicare?
Can Doctors Refuse Medicare? The short answer is "yes." Thanks to the federal program's low reimbursement rates, stringent rules, and grueling paperwork process, many doctors are refusing to accept Medicare's payment for services. Medicare typically pays doctors only 80% of what private health insurance pays.
What percentage of doctors do not accept Medicare assignment?
In all states except for 3 [Alaska, Colorado, Wyoming], less than 2% of physicians in each state have opted-out of the Medicare program.
Does Medicare pay 100 percent of hospital bills?
According to the Centers for Medicare and Medicaid Services (CMS), more than 60 million people are covered by Medicare. Although Medicare covers most medically necessary inpatient and outpatient health expenses, Medicare reimbursement sometimes does not pay 100% of your medical costs.
Does Medicare only pay 80%?
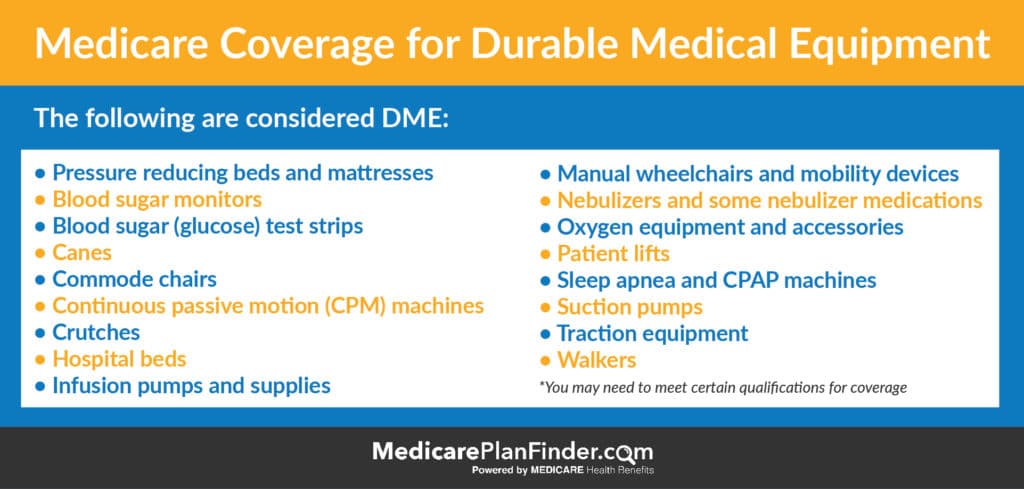
Original Medicare only covers 80% of Part B services, which can include everything from preventive care to clinical research, ambulance services, durable medical equipment, surgical second opinions, mental health services and limited outpatient prescription drugs.
Please give us your feedback!
What do you think about How much doctors are paid by Medicare? Write your comments.
Contact Us
For help finding the best Medicare or Individual Health Plan for you, please contact Liberty Medicare or call us at 877-657-7477.
What is pay for performance?
A pay-for-performance model where the physician’s training, skills and time expended to provide a given service are taken into account when establishing compensation. With this model, the actual care provided by the physician is the driving force of compensation more so than the number of visits.
What is fee for service?
Fee-for-service payment is also the basis of early forms of managed care payment, in what is called ‘discounted fee-for-service’ managed care . This simply means that providers agree to provide health services at prearranged discounts off their regular fee-for-service fees. This is the usual arrangement for PPOs (Preferred Provider Organizations), which are essentially a group of available providers joined together into a network.
What are the benefits of a payment model?
The primary benefit of this payment model is that without the constraint of fee codes, healthcare providers are given increased flexibility in deciding what the patient requires and the needed resources to deliver them. However, as a physician, the concern lies in how administrators manage under such a payment system.
What is concierge medicine?
An alternative to traditional payment models, where medical practices have a direct financial relationship with patients. They typically charge a monthly or annual fee so that the patient receives additional access and personalized care. These practices are known by a variety of names: concierge healthcare, direct primary care, direct care, direct practice medicine, retainer-based, membership medicine, cash-only medicine, cash-only practice, boutique medicine, personalized healthcare.
How many models of bundled payments are there?
With bundled payments, there are four models:
Is fee for service reimbursement going out?
Fee-for-service reimbursement is potentially on its way out, which means more complex payment models are continuing to emerge.
Can you get a single payment for surgery?
A quick example would be an outpatient surgery. Many surgeons will often receive a single payment for pre-op, post-op and the surgery. However, bundled payments can also be much broader, encompassing longer periods of time and multiple providers.
What is Medicare Reimbursement?
If you’re on Medicare, your doctors will usually bill Medicare for any care you obtain. Medicare will then pay its rate directly to your doctor. Your doctor will only charge you for any copay, deductible, or coinsurance you owe.
What if my doctor doesn't bill Medicare?
If your doctor doesn’t bill Medicare directly, you can file a claim asking Medicare to reimburse you for costs that you had to pay.
How long does it take for Medicare to process a claim?
Medicare claims to providers take about 30 days to process. The provider usually gets direct payment from Medicare. What is the Medicare Reimbursement fee schedule? The fee schedule is a list of how Medicare is going to pay doctors. The list goes over Medicare’s fee maximums for doctors, ambulance, and more.
How to get reimbursement for health insurance?
To get reimbursement, you must send in a completed claim form and an itemized bill that supports your claim. It includes detailed instructions for submitting your request. You can fill it out on your computer and print it out. You can print it and fill it out by hand. The form asks for information about you, your claim, and other health insurance you have.
What happens if you see a doctor in your insurance network?
If you see a doctor in your plan’s network, your doctor will handle the claims process. Your doctor will only charge you for deductibles, copayments, or coinsurance. However, the situation is different if you see a doctor who is not in your plan’s network.
Does Medicare cover out of network doctors?
Coverage for out-of-network doctors depends on your Medicare Advantage plan. Many HMO plans do not cover non-emergency out-of-network care, while PPO plans might. If you obtain out of network care, you may have to pay for it up-front and then submit a claim to your insurance company.
Do participating doctors accept Medicare?
Most healthcare doctors are “participating providers” that accept Medicare assignment. They have agreed to accept Medicare’s rates as full payment for their services. If you see a participating doctor, they handle Medicare billing, and you don’t have to file any claim forms.
Transparency And Informed Financial Consent
For medical costs, transparency means being able to understand the typical costs of a treatment or service.
Work Out Your Hospital Admission Costs
As a private patient your total out of pocket costs will be the sum of all hospital charges, doctors fees and fees from other providers, minus any Medicare or private health insurance payments.
Medicare Pays Most Of The Cost For Doctors Visits And Other Services With Some Limitations
Part B medical insurance is intended to cover basic medical services provided by doctors, clinics, and laboratories. The lists of services specifically covered and not covered are long, and do not always make a lot of common sense.
What Does Medicare Part A Cover
Medicare Part A covers the hospital charges and most of the services you receive when you’re in the hospital.
How To Lower Your Health Costs
Stay in the network. Ask your doctor to refer you to a specialist, hospital or surgical center that accepts your plan. Or log in to your secure member account to search our provider directory.
Original Medicare And Emergency Ambulance Transportation
Medicare covers emergency ambulance transportation if youve had a sudden medical emergency and your health is in danger.
Doctor Visits And Medicare Supplement Insurance
It may be useful to know that Medicare Supplement insurance plans may help pay for Medicare Part A and Part B out-of-pocket costs. Medicare Supplement insurance plans generally pay at least part of your coinsurance amounts for Medicare-covered doctor visits. Most standardized plans typically pay the full Part B coinsurance amount.
How much did doctors make in 2012?
The trove of billing records shows that thousands of physicians made more than $1 million each from Medicare in 2012. Dozens billed for more than $10 million. Billing for a large amount is not necessarily a sign of wrongdoing. Doctors may be unusually efficient, may perform procedures that require high overhead, ...
Can doctors perform high overhead?
Doctors may be unusually efficient, may perform procedures that require high overhead, or may treat an especially large number of Medicare patients. Government inspectors, however, have recommended greater scrutiny for high billers.
How much does Medicare pay?
Medicare pays about 70% of what private insurance does .
How much does a direct primary care physician pay?
It’s a sustainable model where a patient engages a physician who has opted out of Medicare and pays them $50–$100 a month to be their physician.
How much did insurance companies pay on the dollar?
All fees were agreed upon beforehand so the insurance companies were essentially given a discount of 30% but made 32 cents on the billed dollar.
What was the rate of acceptance between Medicare and private insurance in 2015?
And in 2015, the rate of acceptance between Medicare and private health insurance was very close, with each registering between 93–94 percent. However, it’s important to remember that Original Medicare does not restrict patients to networks the same way that private insurance does.
How many people are on Medicare in 2015?
In 2015, there were approximately 47.5 million Americans age 65 and over. As of 2014 there were nearly 57 million Americans on Medicare (and that number will only increase in coming years as the Baby Boomer generation enters the over-65 demographic). The remaining 9–10 million Americans who are under 65 and receive Medicare benefits do so by having a qualified disability.
Will doctors' salaries go down under Medicare?
Doctor salaries might go down under a Medicare for all or indeed any healthcare reform, which is why doctors tend to oppose reform. Humans generally, even very smart doctor-y humans, overestimate the pain and underestimate the
Does private insurance pay Medicare?
There is a wide swing from one procedure code (or exam code) to another, but it's said that private insurance pays roughly 120% of Medicare. Private insurance plans also vary code to code, but some pay better in general than others. I set my fee schedule to capture the highest payer for each code from an insurance plan we are contracted with (and see regularly). That means most insurance payments will process a write-off. That means a cash-pay customer will pay the highest rate. This is necessary for us to capture the highest contracted rate and to avoid breaching our contract with the insuran
What percentage of physicians didn't receive salary?
Being employed didn’t necessarily mean a salary. Twenty-three percent of employed physicians didn’t receive salaried payments at all. Productivity was a common payment method, with almost one-half receiving at least some pay based on productivity and 13.8 percent receiving payment exclusively based on their productivity.
Is productivity based pay still important?
In addition, despite the continued focus on alternative payment models, this report indicates that productivity-based pay is still an important factor in physician compensation.