How Does Medicare Insurance Pay Hospitals? Medicare payment systems have evolved over the past few decades, but they continue to use a pay-per-service payment model. This is known as the Inpatient Prospective Payment System, or IPPS. This system is based on diagnosis-related groups (DRGs).
How much Medicare pays hospitals?
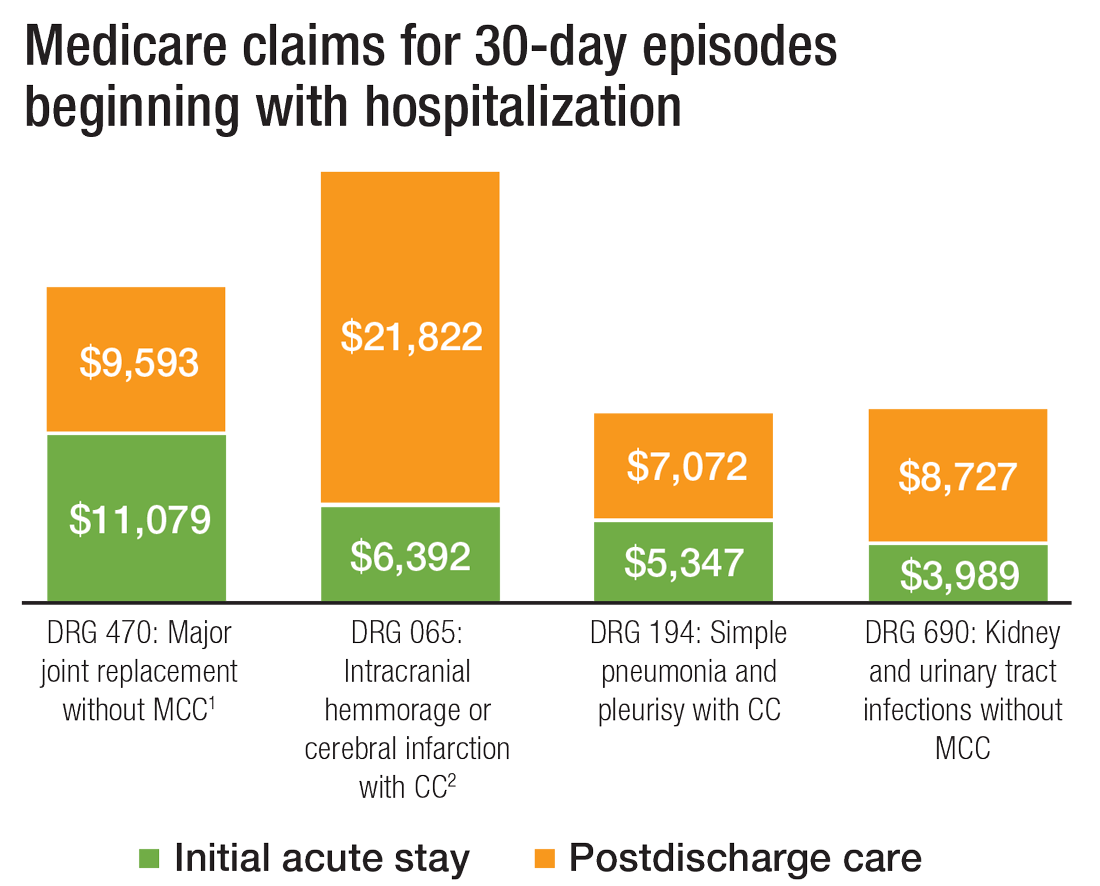
Mar 23, 2020 · Reimbursement is based on the DRGs and procedures that were assigned and performed during the patient’s hospital stay. Each DRG is assigned a cost based on the average cost based on previous visits. This assigned cost provides a simple method for Medicare to reimburse hospitals as it is only a simple flat rate based on the services provided.
How does Medicare reimburse hospitals?
How Does Medicare Insurance Pay Hospitals? Medicare payment systems have evolved over the past few decades, but they continue to use a pay-per-service payment model. This is known as the Inpatient Prospective Payment System, or IPPS. This …
How does Medicare rate hospitals and nursing homes?
Jun 11, 2018 · However, most of that literature has focused on the commercially insured population. 1,2 Although nearly one-third of Medicare beneficiaries are enrolled in a Medicare Advantage (MA) plan, little is known about the prices paid to hospitals by the private insurers that administer such plans. It might be expected that the prices paid to hospitals by MA plans …
How long will Medicare pay for a hospital stay?
In Original Medicare, these are additional days that Medicare will pay for when you're in a hospital for more than 90 days. You have a total of 60 reserve days that can be used during your lifetime. For each lifetime reserve day, Medicare pays all covered costs except for a daily coinsurance. : …

Does Medicare pay 100 percent of hospital bills?
Most medically necessary inpatient care is covered by Medicare Part A. If you have a covered hospital stay, hospice stay, or short-term stay in a skilled nursing facility, Medicare Part A pays 100% of allowable charges for the first 60 days after you meet your Part A deductible.
Do hospitals benefit from Medicare?
Medicare helps cover certain medical services and supplies in hospitals. If you have both Medicare Part A (Hospital Insurance) and Medicare Part B (Medical Insurance), you can get the full range of Medicare-covered services in a hospital.
How does Medicare work for hospital stays?
Medicare covers a hospital stay of up to 90 days, though a person may still need to pay coinsurance during this time. While Medicare does help fund longer stays, it may take the extra time from an individual's reserve days. Medicare provides 60 lifetime reserve days.May 29, 2020
Which part of Medicare pays for hospital expenses?
Medicare Part A hospitalMedicare Part A hospital insurance covers inpatient hospital care, skilled nursing facility, hospice, lab tests, surgery, home health care.
What happens when Medicare hospital days run out?
Medicare will stop paying for your inpatient-related hospital costs (such as room and board) if you run out of days during your benefit period. To be eligible for a new benefit period, and additional days of inpatient coverage, you must remain out of the hospital or SNF for 60 days in a row.
What part of Medicare pays for physician services and outpatient hospital care?
Part BPart B covers certain doctors' services, outpatient care, medical supplies, and preventive services.
What is the Medicare 2 midnight rule?
The Two-Midnight rule, adopted in October 2013 by the Centers for Medicare and Medicaid Services, states that more highly reimbursed inpatient payment is appropriate if care is expected to last at least two midnights; otherwise, observation stays should be used.Nov 1, 2021
What is not covered by Medicare?
Medicare does not cover: medical exams required when applying for a job, life insurance, superannuation, memberships, or government bodies. most dental examinations and treatment. most physiotherapy, occupational therapy, speech therapy, eye therapy, chiropractic services, podiatry, acupuncture and psychology services.Jun 24, 2021
What benefits fall under Medicare Part A?
Part A generally covers inpatient hospital stays, skilled nursing care, hospice care, and limited home health-care services. You typically pay a deductible and coinsurance and/or copayments.
Which of the following expenses would be paid by Medicare Part B?
Medicare Part B helps cover medically-necessary services like doctors' services and tests, outpatient care, home health services, durable medical equipment, and other medical services.Sep 11, 2014
What is the Medicare Part B deductible for 2021?
$203 inMedicare Part B Premiums/Deductibles The standard monthly premium for Medicare Part B enrollees will be $148.50 for 2021, an increase of $3.90 from $144.60 in 2020. The annual deductible for all Medicare Part B beneficiaries is $203 in 2021, an increase of $5 from the annual deductible of $198 in 2020.Nov 6, 2020
What is Medicare Part A deductible for 2021?
The Medicare Part A inpatient hospital deductible that beneficiaries pay if admitted to the hospital will be $1,556 in 2022, an increase of $72 from $1,484 in 2021.Nov 12, 2021
What is Medicare insurance?
Medicare insurance is one of the most popular options for those who qualify, and the number of people using this insurance continues to grow as life expectancy continues to increase. Medicare policies come available with many different parts, including Part A, Part B, Part C, and Part D.
What is the lowest level of severity?
The highest level of severity is labeled Major Complication or Comorbidity, the next level is known as Complication or Comorbidity, and the lowest severity level is known as Non-Complication. The lowest level has little impact on illness severity and uses minimal hospital resources.
Does Medicare cover inpatient care?
If you receive care as an inpatient in a hospital, Medicare Part A will help to provide coverage for care. Part A Medicare coverage is responsible for all inpatient care , which may include surgeries and their recovery, hospital stays due to illness or injury, certain tests and procedures, and more. As far as out-of-pocket costs, you will be ...
What is an inpatient hospital?
Inpatient hospital care. You’re admitted to the hospital as an inpatient after an official doctor’s order, which says you need inpatient hospital care to treat your illness or injury. The hospital accepts Medicare.
What is a critical access hospital?
Critical access hospitals. Inpatient rehabilitation facilities. Inpatient psychiatric facilities. Long-term care hospitals. Inpatient care as part of a qualifying clinical research study. If you also have Part B, it generally covers 80% of the Medicare-approved amount for doctor’s services you get while you’re in a hospital.
What is general nursing?
General nursing. Drugs as part of your inpatient treatment (including methadone to treat an opioid use disorder) Other hospital services and supplies as part of your inpatient treatment.
What Does DRG Mean?
DRG stands for diagnosis-related group. Medicare's DRG system is called the Medicare severity diagnosis-related group, or MS-DRG, which is used to determine hospital payments under the inpatient prospective payment system (IPPS).
Figuring Out How Much Money a Hospital Gets Paid for a Given DRG
In order to figure out how much a hospital gets paid for any particular hospitalization, you must first know what DRG was assigned for that hospitalization.
Are Hospitals Making or Losing Money?
After the MS-DRG system was implemented in 2008, Medicare determined that hospitals' based payment rates had increased by 5.4% as a result of improved coding (i.e., not as a result of anything having to do with the severity of patients' medical issues).
The claim: Hospitals get paid more if patients are listed as COVID-19, and on ventilators
Sen. Scott Jensen, R-Minn., a physician in Minnesota, was interviewed by "The Ingraham Angle" host Laura Ingraham on April 8 on Fox News and claimed hospitals get paid more if Medicare patients are listed as having COVID-19 and get three times as much money if they need a ventilator.
Provision in the relief act
The coronavirus relief legislation created a 20% premium, or add-on, for COVID-19 Medicare patients.
How does Medicare pay?
Snopes investigated the claim, finding it's plausible Medicare pays in the range Jensen mentions but doesn't have a "one-size-fits-all" payment to hospitals for COVID-19 patients.
Our ruling: True
We rate the claim that hospitals get paid more if patients are listed as COVID-19 and on ventilators as TRUE.
What percentage of PFS does Medicare pay?
When a teaching anesthesiologist is located in an Optional Payment Method CAH and reassigns their outpatient services billing, Medicare pays 115 percent of the PFS if the anesthesiologist is involved in one of these cases:
Does Medicare pay for ambulance transport?
Medicare pays CAH-furnished (or an entity owned and operated by a CAH) ambulance transport services based on 101 percent of reasonable costs if the CAH is the only ambulance transport provider or supplier (or entity) providing services within a 35-mile drive.
When does NCTAP end?
The NCTAP, designed to mitigate potential financial disincentives for hospitals to provide new COVID-19 treatments, is effective from November 2, 2020, until the end of the COVID-19 public health emergency (PHE). Through the NCTAP, the Medicare Program will provide an enhanced payment for eligible inpatient cases that use certain new products ...
When was Remdesivir approved?
On October 22, 2020, the FDA approved remdesivir (Veklury) for the treatment of COVID-19 for adults and certain pediatric patients requiring hospitalization. On November 19, 2020, the FDA issued an EUA for the use of baricitinib (Olumiant), in combination with remdesivir (Veklury), for the treatment of suspected or laboratory confirmed COVID-19 in ...
