However, if the beneficiary injects their insulin with a needle (syringe), Medicare Part B does not cover the cost of the insulin, but the Medicare prescription drug benefit (Part D) covers the insulin and the supplies necessary to inject it.
Which Medicare plan covers insulin?
and gauze. The Medicare Part D plan will cover the insulin and any other medications to treat diabetes at home as long as the beneficiary is on the Medicare Part D plan’s formulary. Coverage for diabetes-related durable medical equipment (DME) is provided as a Medicare Part B benefit. The Medicare Part B deductible and coinsurance or copayment applies after the yearly Medicare part B deductible is met.
Does Medicare cover EpiPens?
Most Medicare prescription drug plans, including those bundled with Medicare Advantage policies, cover either EpiPen or a generic alternative. Medicare Part C and D drug plans typically provide coverage for a wide range of name brand and generic prescription medications.
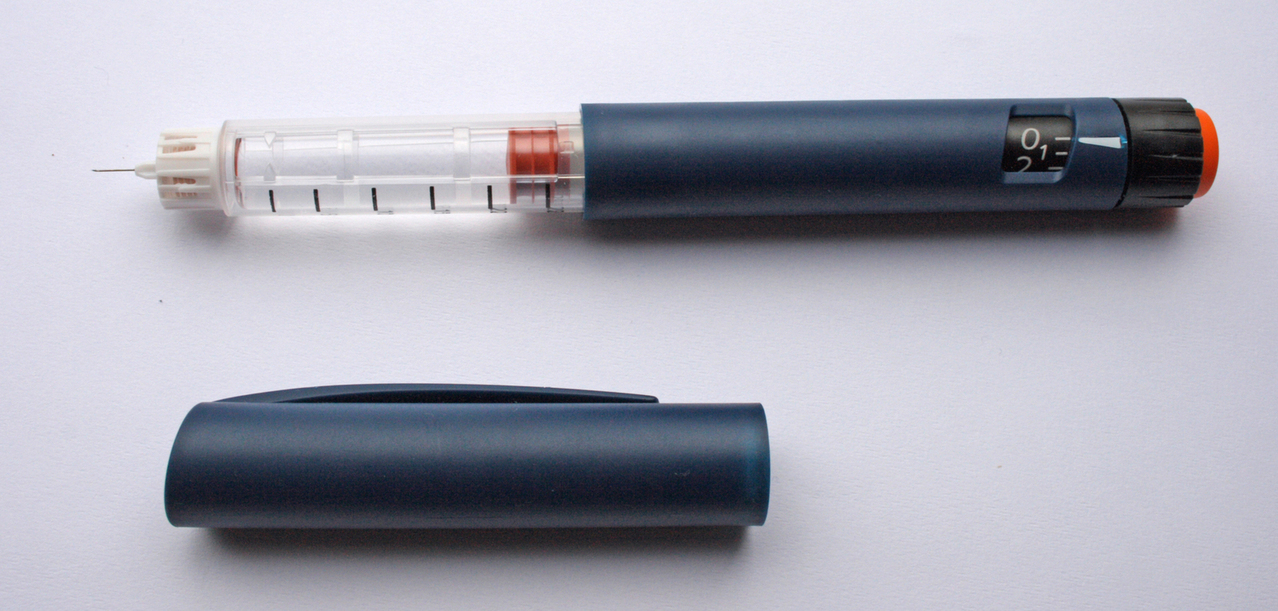
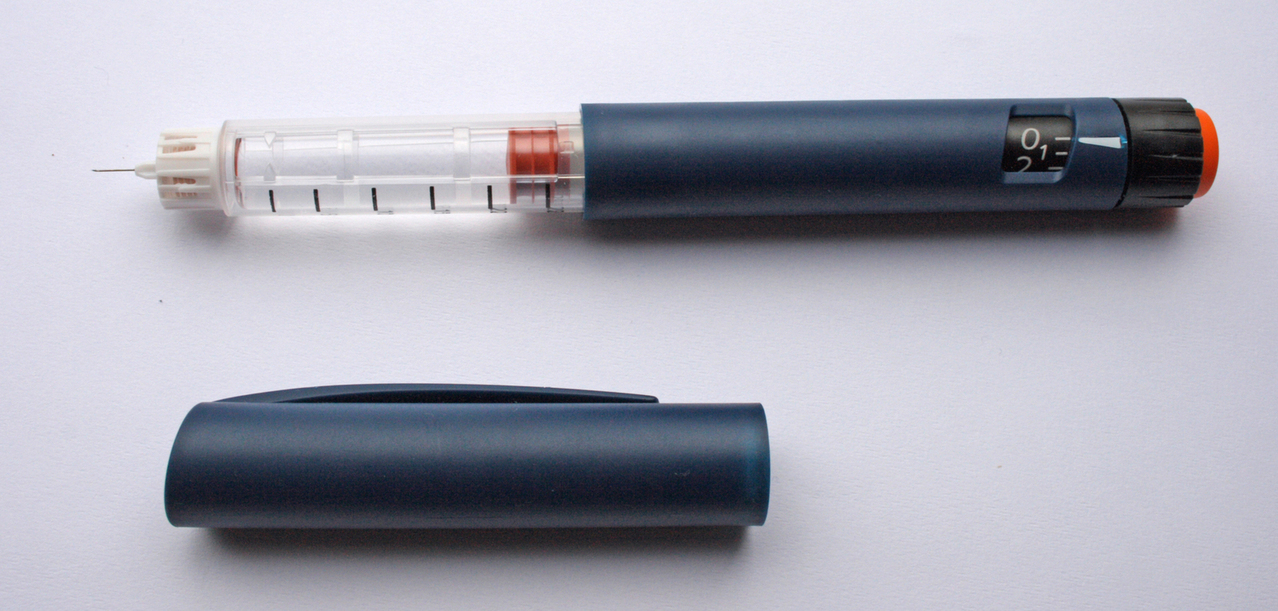
Does Medicare Part D cover Lantus?
Medicare coverage through a Part D prescription drug plan may cover certain brands of insulin and the supplies necessary to administer it, such as the pen-style syringe used for Lantus. Additionally, gauze and alcohol swabs may be covered underneath a Part D plan.
Are insulin needles covered by Medicare?
Your Medicare Part D prescription drug plan may cover supplies you need to inhale or inject insulin. These include alcohol swabs, gauze, inhaled insulin devices and syringes and needles. Insulin Pump Insulin pumps worn outside the body and the insulin they use may be covered by Part B if you meet certain criteria.
Does Medicare pay for insulin syringes?
The amount you must pay for health care or prescriptions before Original Medicare, your Medicare Advantage Plan, your Medicare drug plan, or your other insurance begins to pay. ). You pay 100% for syringes, needles, alcohol swabs, and gauze, unless you have Part D.
Does Medicare cover the cost of syringes?
Part D covers certain medical supplies to administer insulin, including syringes, needles, alcohol swabs, gauze, and inhaled insulin devices.
Which Medicare level is for medicine insulin and syringes?
If you're diagnosed with diabetes, you will need certain medical supplies to administer the insulin. Supplies may include syringes, needles, alcohol swabs, gauze, and inhaled insulin devices. Medicare Part D covers these medical supplies for diabetes.
Does Medicare Part B pay for syringes?
Original Medicare Part B does not cover these diabetic supplies: Insulin (unless used with an insulin pump) Insulin pens, syringes, or needles. Alcohol swabs or gauze.
Are insulin needles considered DME?
Since that time, newer insulin delivery devices in the form of both mechanical and electronic insulin pumps have become available that are not coverable under the Medicare Part B durable medical equipment (DME) benefit.
Will insurance cover syringes?
If your health insurance covers durable medical equipment, it may pay for a blood glucose meter, a finger-stick device, pens, pen needles, syringes, a pump, infusion sets, a continuous glucose monitor and/or an insulin injector.
What tier does insulin fall under?
A large number of plans placed insulin products on Tier 3, the preferred drug tier, with a $47 copayment per prescription during the initial coverage phase; more plans used this combination of tier placement and cost-sharing requirement for coverage of insulin than any other combination in 2019 (Table 3, Table 4).
Does Medicare Part B cover insulin pens?
Part B covers some equipment used by people with diabetes as DME. This includes blood sugar monitors, continuous glucose monitors, therapeutic shoes, lancet devices, blood glucose test strips, and insulin pumps. However, insulin pens are not covered.
What is the insulin senior savings program?
A: The Part D Senior Savings Model allows participating Part D prescription drug plans to offer a broad set of formulary insulins at a maximum $35.00 copayment per month's supply, throughout the deductible, initial coverage, and coverage gap phases of their Part D drug coverage.
Does Part D cover insulin needles?
If a beneficiary injects their insulin with a needle (syringe), Medicare Part B does not cover the cost of the insulin, but the Medicare prescription drug benefit (Part D) covers the insulin and the supplies necessary to inject it. This includes syringes, needles, alcohol swabs and gauze.
What items are covered under Medicare Part B for diabetic patients?
Part B covers blood sugar (also called blood glucose) self-testing equipment and supplies as durable medical equipment, even if you don't use insulin. Part B covers the same type of blood sugar testing supplies listed above for people with diabetes whether or not they use insulin.
Is insulin covered under Medicare Part B or D?
Most Medicare Advantage plans include prescription drug coverage (Part D), which covers insulin.
What is the donut hole in Medicare?
Many diabetes patients requiring insulin will end up in the Medicare coverage gap known as the “donut hole,” where they’re responsible for a greater share of the drugs’ costs. When this happens, a patient’s out-of-pocket costs at the pharmacy spike dramatically — for example, from a $40-per-month co-pay to $350 a month. Even worse, some patients struggling with the expenses will drop or stop dosages or switch brands — decisions that can be dangerous to their health if not overseen by their doctor and can actually keep them in the donut hole, costing even more. These erratic costs can be a financial and emotional rollercoaster. Understanding how Medicare Part D Prescription Drug coverage works in regard to insulin can help you plan for price increases and the likelihood that you’ll enter the donut hole coverage gap. To help you, we’ll take you — chronologically — through a calendar year of expenses that a typical patient with diabetes on two forms of insulin may pay, so you can see real-world examples of how the four coverage phases can impact finances. But keep in mind that everyone’s situation can vary greatly, depending on their individual drug plans, other prescriptions and multiple other factors. The four Part D coverage phases First, it’s important to understand how your coverage works. Medicare Part B (medical insurance) does not cover insulin — unless use of an insulin pump is medically necessary. (If you use an external insulin pump, Part B may cover the insulin and the pump.) So having Part D — supplemental prescription drug coverage — is critical for many people to afford injectable insulin. Medicare Part D Prescription Drug coverage has four phases: The deductible phase — you pay the full drug cost until you hit your deductib Continue reading >>
What supplies does Medicare cover?
HEALTH FEATURE ARCHIVE Diabetes Supplies: What Medicare Covers 1. Self-testing equipment and supplies: Medicare Part B covered diabetes supplies: Coverage for glucose monitors, test strips, and lancets. Who is covered: All people with Medicare who have diabetes (insulin users and non-users). Medicare covers the same supplies for people with diabetes whether or not they use insulin. These include glucose testing monitors, blood glucose test strips, lancet devices and lancets, and glucose control solutions. There may be some limits on supplies or how often you get them. For more information about diabetic supplies, call your Durable Medical Equipment Regional Carrier. How to get your diabetes equipment and supplies: To get your diabetes equipment and supplies under Medicare, you need a prescription from your doctor. The prescription should say: You have been diagnosed with diabetes. How many test strips and lancets you need in a month. What kind of meter you need. For example, if you need a special meter for vision problems, the doctor should say that and state the medical reason why you need a special meter. Whether you use insulin or not. How often you should test your blood sugar. Points to remember: Ask your doctor or health care provider if regular blood sugar testing is right for you. You need a prescription from your doctor to get your diabetes equipment and supplies under Medicare. Learn the correct way to use your blood sugar meter properly. Your pharmacist, doctor, diabetes educator, or another health care provider can help you. Keep track of your blood sugar readings and share them with your doctor or health care provider at regular visits. Do not accept shipments of diabetes equipment and supplies that you did not ask for. 2. Therapeutic shoes: Medicare also c Continue reading >>
Does Medicare cover insulin?
"The Part D part of a Medicare Advantage with a Prescription Drug Plan covers insulin and other diabetic medications," said Sen. "The member's cost share depends on the formulary." A formulary is the list of all medications approved for use under the plan. According to the New York Department of Health, there is no standard formulary for Medicare Part D plans. While they must meet basic standards set forth by the federal government, each plan is free to set its own management regulations and fee structure within those guidelines. Selecting the right Medicare plan for insulin coverage Medicare Part D plans are offered by private health insurance companies, and benefits and costs may vary significantly between plans. Andrea Gary from the Florida State Health Insurance Assistance Program, known as SHINE, advises beneficiaries to carefully review their out-of-pocket costs as well as any limitations on their benefits. "The beneficiary would be responsible for any coinsurance or copayment as well as the any applicable Part D deductible," said Gary. Before signing up for a specific plan, patients should check to see if the policy limits the number of needles or syringes that will be covered each month. In addition, some Medicare Part D plans may impose restrictions on which pharmacies a beneficiary can use or require prior authorization or step therapy before paying for certain medications. "To save money on drugs, insulin-dependent diabetics should consider purchasing a prescription drug plan along with their Medicare coverage," said Sen. "They can compare the plans available in their area on Medicare.gov to check the different drug lists and member cost shares." Interview with Andrea Gary | SHINE, Interview with Ami Sen | WellPoint, Medicare.gov You will receive your first Continue reading >>
Can I order diabetes supplies through mail order?
The Medicare rules for ordering diabetes supplies through a mail-order pharmacy have changed. Here is the information you need to know to make this transition smoothly. On July 1, a Medicare rule took effect that impacts beneficiaries who get their diabetes testing supplies via mail order. It’s referred to as the Medicare National Mail-Order Program. Under the new ruling, beneficiaries must buy their diabetes supplies, including blood glucose trips, lancets, lancet devices, batteries and control solution, through a list of designated vendors, or Medicare national mail-order contract suppliers. Beneficiaries who pick up their testing supplies from a local pharmacy can still do so, but they need to make sure that the store accepts Medicare "assignment" to avoid higher charges for the supplies. At Joslin Diabetes Center, we are closely monitoring this new program which is intended to be a cost-cutting measure. If you have questions or difficulties navigating the new system, we provided you with additional details to ensure the program is not a disruption to your diabetes care. Who is affected? Medicare beneficiaries in all 50 states, D.C., Puerto Rico, the U.S. Virgin Islands, Guam, and American Samoa, who have Original Medicare, are impacted. These changes do not apply to Medicare Advantage plans (like an HMO or PPO). If you are enrolled in a private plan through Medicare, you can contact your plan to find out which suppliers you can use. How can I get my supplies? If you want diabetes testing supplies delivered to your home, you must use an approved Medicare national mail-order contract supplier in order for Medicare to help pay for the supplies. To find a contract supplier, you can call 1-800-MEDICARE (1-800-633-4227) or visit www.medicare.gov/supplier. Alternatively, Continue reading >>
Does Medicare cover Omnipod insulin pump?
Medicare Part D to Cover Omnipod Insulin Delivery System The Omnipodinsulin management system (Insulet Corporation) may be covered now under the Medicare Part D (prescription drug) program, according to the Centers for Medicare and Medicaid Services (CMS). Omnipod performs the same functions as a traditional insulin pump, but with a different design. Rather than a pump that attaches via tubing connected to an infusion site on the body, the insulin-containing "pods" are worn directly on the body and insulin infusion is controlled wirelessly by a "personal diabetes manager [PDM]" that also houses a glucose meter. Because of its unique design the PDM is nondisposable, but the pods that delivers the insulin are replaced every 3 days the system does not meet the criteria for durable medical equipment under Medicare Part B, the way other insulin pumps are covered. Instead, CMS has deemed the system reimbursable under Part D as a medical supply "associated with the injection of insulin," a category that also includes syringes and pens, needles, and alcohol swabs. Another insulin delivery device, the V-Go (Valeritas), is also covered under Medicare Part D. "We expect that technology will continue to advance and 'medical supplies associated with the injection of insulin' will become significantly more sophisticated. Part D sponsors may include such supplies in their benefit," Jennifer R Shapiro, Acting Director of the Medicare Drug Benefit and C&D Data Group, Baltimore, Maryland, wrote in a letter to Part D Plan carriers. But coverage isn't mandatory, she said. "While CMS recognizes such products as medical supplies that are alternatives to insulin syringes, CMS does not require Part D sponsors to include them on their formularies, and sponsors may apply utilization management Continue reading >>
Is NovoLog a contraindication?
NovoLog® is contraindicated during episodes of hypoglycemia and in patients hypersensitive to NovoLog® or one of its excipients. Never Share a NovoLog® FlexPen, NovoLog® FlexTouch®, PenFill® Cartridge, or PenFill® Cartridge Device Between Patients, even if the needle is changed. Patients using NovoLog® vials must never share needles or syringes with another person. Sharing poses a risk for transmission of blood-borne pathogens. Changes in insulin strength, manufacturer, type, or method of administration may affect glycemic control and predispose to hypoglycemia or hyperglycemia. These changes should be made cautiously under close medical supervision and the frequency of blood glucose monitoring should be increased. NovoLog® (insulin aspart injection) 100 U/mL is an insulin analog indicated to improve glycemic control in adults and children with diabetes mellitus. NovoLog® is contraindicated during episodes of hypoglycemia and in patients hypersensitive to NovoLog® or one of its excipients. Never Share a NovoLog® FlexPen, NovoLog® FlexTouch®, PenFill® Cartridge, or PenFill® Cartridge Device Between Patients, even if the needle is changed. Patients using NovoLog® vials must never share needles or syringes with another person. Sharing poses a risk for transmission of blood-borne pathogens. Changes in insulin strength, manufacturer, type, or method of administration may affect glycemic control and predispose to hypoglycemia or hyperglycemia. These changes should be made cautiously under close medical supervision and the frequency of blood glucose monitoring should be increased. Hypoglycemia is the most common adverse effect of insulin therapy. The timing of hypoglycemia may reflect the time-action profile of the insulin formulation. Glucose monitoring is re Continue reading >>
What Does Medicare Cover For People With Diabetes?
For people with diabetes, Medicare Part B will cover blood glucose monitors, test strips, lancet devices, and lancets. In addition, glucose management solutions for those with diabetes are covered whether someone uses insulin or not. Also covered are, medical nutrition therapy and a number of hours for diabetes self-management training. Some people with diabetes may qualify for therapeutic shoe coverage and foot exams are covered once every six month as long as you haven’t seen a foot care specialist between visits. Medicare Part B also covers insulin pumps and pump supplies as well as the insulin used specifically in the pump as long as certain requirements are met. Under Medicare Part B, those with diabetes who are on insulin may get up to 300 test strips and 300 lancets every three months and those who have diabetes but don’t use insulin may get up to 100 test strips and 100 lancets every three months. You may be able to get more if your doctor says it is medically necessary and documents this need. As part of prevention care, within the first year of Part B coverage, you get coverage for a “Welcome to Medicare” physical exam. Then after that, an “Annual Wellness visit” is covered each year. During these visits, a personalized prevention plan is created and used. When you need to find out if a test, item, or service is covered, you can search it at Medicare.gov. Compare Medicare Plans now. How to Get the Brands You Need Covered by Medicare The rules of Medicare states your doctor can prescribe the specific item or brand of diabetes testing supplies you need. Your doctor must put this in writing and also make a note in your medical record indicating that you need this exact item or brand in order to avoid an adverse medical outcome. Once your doctor does t Continue reading >>
What Medical Services Are Not Covered By Health Insurance, Medicaid, Medicare?
Medicaid, Medicare and most private insurers will not cover any non-allopathic services. These include Vedic Medicine, Chinese Medicine, Chiropractic, Naturopathy, etc. They also usually do not cover allied health services like fitness training, nutrition counseling, therapeutic massage, etc. Most will also not cover dental or vision services. Some also do not cover podiatry. Most have a list of procedures they designate as “elective.” This usually includes procedures like rhinoplasty and breast augmentation. There is sometimes an argument over whether certain orthopedic procedures are necessary or elective. Continue reading >>
Is The Lantus Insulin No Longer Covered By Health Insurance?
My understanding is soon Lantus will no longer be produced and everyone needs to be switched to the biosimilar insulin Basalar. Insurances are not covering Lantus because they want you switched before Lantus goes out of production. It is a 1:1 conversion. You will use the same dose of Basalar as you use with Lantus. My suspicion for this change is because the patent for Lantus has expired. Insulin falls into a different category of medication. Generics are not AB rated, they are instead called a biosimilar. As pharmacists in the United States we cannot legally substitute one biosimilar for another, we need a new prescription for the different medication. A current example is with the EpiPen. There is a generic version available but because it is a biosimilar we cannot automatically substitute it. We need to get permission (basically, get a new Rx) from your prescriber. There is a lawsuit currently making its way through the US courts which would change the law and allow us to substitute one biosimilar for another. If it gets ok’d we could automatically substitute biosimilar generics equivalents when they exist. But that won't work if everyone is on a new insulin that does “not” have a generic equivalent, something called, oh, I don't know, let's call it Basalar. Now to switch to the generic biosimilar of Lantus, your pharmacist once again has to get a new prescription for the new-to-market generic insulin- exactly the same way we need to currently get a new Rx for Basalar. Many pharmacists won't make the phone call unless you ask because, frankly, it takes extra time and there is already a processed insurance claim. (For proof of this statement, I reference the Epipen. Pharmacists often don't make the time to call for a new Rx with the biosimilar generic on that m Continue reading >>
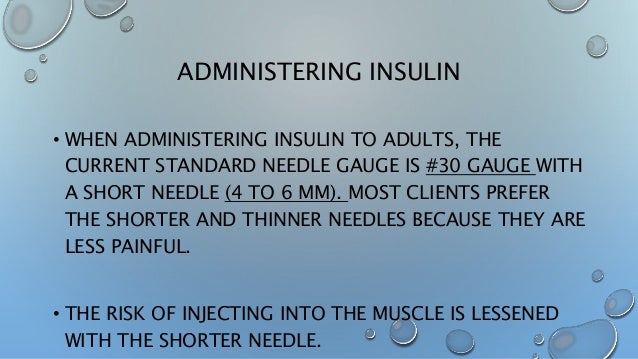
Are Syringes And Needles Covered Under Medicare?
Are syringes and needles covered under Medicare? Around 9 million Americans use syringes and needles to help stabilize their medical conditions from home, amounting to over 3 billion total used each year. Injection devices are commonly used to administer insulin for diabetes patients, but can also be used for a variety of medical conditions such as allergies, hepatitis, arthritis, HIV/AIDS and cancer. These medical supplies typically range in sizes depending on the volumes and lengths needed to treat a diagnosed ailment. 6 millimeters, 8 millimeters and 12.7 millimeters are mainly used for at-home injections, however it’s important to consult with your doctor regarding which variety is necessary for your condition. Does Medicare cover syringes and needles? Normally Medicare Part B covers durable medical equipment, or DME needed for treatment, but it does not cover hypodermic objects needed for insulin or other medical usage. However, Medicare Part D – prescription drug coverage – insures any injectable objects along with other insulin supplies needed for diabetes, such as alcohol swabs, gauze and inhalant devices. Payments may vary depending on your private insurance plan and monthly Medicare Part D premium, but you’ll pay no more than five percent of your prescription costs after spending a certain amount out of pocket each year. How do I qualify for coverage? Anyone enrolled in the Medicare program with either Part A or B can obtain drug coverage with Part D, regardless of income. There are no physical exams necessary, and you cannot be denied enrollment due to health reasons or previous drug prescriptions. Other people included are: Ages 65 and older and are United States Citizens or permanent residents Under 65 years old with certain disabilities People with Continue reading >>
Does Medicare Cover Insulin Pumps And Other Supplies?
Original Medicare’s benefits (Medicare Part A and Part B) are broad and it offers coverage for some medical devices. However, Original Medicare does not cover insulin pens. If you have diabetes and use insulin pens, you’ll either have to pay out of pocket for the devices, or you can enroll in a Medicare Part D prescription drug plan, which may pay for the insulin pens. The population of diabetic people around the world is expected to grow, with a projected 366 million people with diabetes by 2030. One form of treatment involves the use of insulin pens, which can deliver doses of insulin in a disposable and discreet container. Original Medicare does not cover the use of insulin pens. In fact, Medicare doesn't pay for a variety of insulin-delivering tools: insulin pens, gauze, needles or alcohol swabs. Medicare Part B does have one exception: insulin pumps. If a doctor states that it is medically necessary for you to use an insulin pump, the pump and the insulin supply may be covered as durable medical equipment under Medicare Part B. In this situation, you’d pay 20 percent of Medicare’s approved amount for the cost of the insulin and pump. You'd also be responsible for paying your Part B deductible. Does Medicare Part D Cover Insulin? A Medicare Part D prescription drug plan could potentially cover your use of insulin pens and other diabetic supplies such as syringes. Medicare Part D plans are sold by private insurers, so the exact medical supplies, prescriptions and other health care services they cover will vary based on your Part D plan provider. Part D plans can be used in conjunction with Original Medicare and with Medigap plans (Medicare Supplement Insurance). To find out if a Medicare Part D plan covers insulin pens, be sure to inquire with the plan provid Continue reading >>
Are Hearing Aids Covered By Medicare?
In general, Original Medicare (Parts A and B) and most Medicare Supplement (or Medigap) plans do not cover the cost of hearing aids, routine hearing exams, or audiological device fittings. There are some Medicare Advantage plans (Medicare Part C) which cover hearing exams and hearing aids. Check with your insurance provider to learn if your Medicare Advantage plan includes coverage for hearing aids and care for hearing loss. Continue reading >>
Does Medicare In Australia Cover Supplies For Insulin Pumps For Type 1 Diabetics?
TID 51 years, 5 of them on a pump. As Samantha Scanlon mentioned in her answer, insulin pumps can be covered in part or whole by private health insurance in Australia, provided certain criteria are satisfied. The re-provision and funding of pumps once they exceed warranty varies between private insurance companies also. There is a Government Insulin Pump Program ( commenced in 2008) which provides an insulin pump to suitable applicants without private health insurance and total family income less than AUD $ 107, 548. Cost of insulin pumps in Australia varies between about AUD 6,500 and 9,000. The program was previously dogged by the duplication of pump supply subsidy through Insulin Pump subsidy and the National Diabetes Supply Scheme (NDSS). The up shot was that money for insulin pumps was siphoned off into paying for consumables by this duplication. The fact that it took from 2008 to 2017 to sort this out is no laughing matter amongst diabetics, health professionals and peak health bodies. Inconsistencies and inefficiencies between sections of the Department of Health here , plus the ogre of economic measures, is an all too familiar sight. The adage, ‘A stitch in time saves nine’, in relation to better diabetes control lowering the risk of complications from diabetes, seems to take an inordinate time to filter through the machinations and minds of a Government Departments. So all consumables for insulin pumps are now via NDSS, as of 1st July 2017. ( including subsidy of CGM for type 1 diabetics under age 21, BUT NOT FOR PREGNANT WOMEN WITH DIABETES, Doh !!!) The Australian Government says it can fund 90 pumps per year. ( instead of the previous 63 per year). Experts say this is a far cry from meeting the need of the type 1 diabetic population and favours those type Continue reading >>
Why is insulin important?
Insulin plays a vital role in our health but when imbalances in insulin production or absorption occur, conditions like diabetes can develop and lead to serious health concerns. Detecting and treating diabetes and other insulin-related conditions can affect your well-being and quality of life for years to come.
Why is screening for diabetes important?
Mobility issues and dietary habits can lead to obesity, a major contributing factor in the development of diabetes. Screening for diabetes is an important part of preventive care as we age, especially if a patient is overweight, has a family history of diabetes or has experienced high cholesterol or blood pressure.
Does Medicare cover insulin?
If your physician prescribes insulin, your Medicare coverage may help you cover the costs of your treatment. Individuals who qualify for Medicare because they are 65 or older or under 65 with certain disabilities may get help paying for their insulin, but your coverage may depend on your specific circumstances.
Is a pump covered by Medicare?
These devices may be covered by Medicare Part B when ordered by a physician. Even if a pump is an available benefit, there may be specific qualifications for your selected device in order for it to be considered a covered expense. Medicare Advantage Coverage for Diabetes Management.
What is Part B for diabetes?
In addition to diabetes self-management training, Part B covers medical nutrition therapy services if you have diabetes or renal disease. To be eligible for these services, your fasting blood sugar has to meet certain criteria. Also, your doctor or other health care provider must prescribe these services for you.
How long can you have Medicare Part B?
If you’ve had Medicare Part B for longer than 12 months , you can get a yearly “Wellness” visit to develop or update a personalized prevention plan based on your current health and risk factors. This includes:
What is the A1C test?
A hemoglobin A1c test is a lab test that measures how well your blood sugar has been controlled over the past 3 months. If you have diabetes, Part B covers this test if your doctor orders it.
What is diabetes self management training?
Diabetes self-management training helps you learn how to successfully manage your diabetes. Your doctor or other health care provider must prescribe this training for Part B to cover it.
Does Medicare cover diabetes?
This section provides information about Medicare drug coverage (Part D) for people with Medicare who have or are at risk for diabetes. To get Medicare drug coverage, you must join a Medicare drug plan. Medicare drug plans cover these diabetes drugs and supplies:
Does Part B cover insulin pumps?
Part B may cover insulin pumps worn outside the body (external), including the insulin used with the pump for some people with Part B who have diabetes and who meet certain conditions. Certain insulin pumps are considered durable medical equipment.
Does Medicare cover diabetic foot care?
Medicare may cover more frequent visits if you’ve had a non-traumatic ( not because of an injury ) amputation of all or part of your foot, or your feet have changed in appearance which may indicate you have serious foot disease. Remember, you should be under the care of your primary care doctor or diabetes specialist when getting foot care.
What Medicare Plans Cover Diabetes?
Fortunately, the answer to “Does Medicare cover diabetes?” is yes. Both Original Medicare and Medicare Advantage plans will cover diabetes testing, treatment, and prevention programs.
What Are Your Costs for Diabetes with Medicare?
Your costs with Original Medicare will depend on the treatment or medical service. Also, you’ll need to make sure your provider participates in Medicare and accepts assignments so that Medicare coverage will apply.
What is CMS in healthcare?
The Centers for Medicare & Medicaid Services (CMS) has developed a variety of educational resources for use by health care professionals and their staff as part of a broad outreach campaign to promote awareness and increase utilization of preventive services covered by Medicare. For more information about coverage, coding, billing, and reimbursement of Medicare-covered preventive services and screenings, visit
Does Medicare cover therapeutic shoes?
If a beneficiary has Medicare Part B, has diabetes, and meets certain conditions (see below), Medicare will cover therapeutic shoes if they need them. The types of shoes that are covered each year include one of the following:
Does Medicare pay for insulin pumps?
In the Original Medicare Plan, the beneficiary pays 20 percent of the Medicare-approved amount after the yearly Part B deductible. Medicare will pay 80 percent of the cost of the insulin pump. Medicare will also pay for the insulin that is used with the insulin pump.
Tracking Information
This is a longstanding national coverage determination. The effective date of this version has not been posted.
Description Information
Please Note: This may not be an exhaustive list of all applicable Medicare benefit categories for this item or service.
Transmittal Information
5/1989 - Added statutory authority citation. Effective date NA. (TN 36)