Medicare Advantage, a health plan provided by private insurance companies, is paid for by federal funding, subscriber premiums and co-payments. It includes the same coverage as the federal government’s Original Medicare program as well as additional supplemental benefits. What is Medicare Advantage?
Full Answer
How much does Medicare pay Advantage plans?
Medicare Advantage plans have a cap on what the member must pay each year for health care services. Once the cap is met (anywhere from $3,500 to $6,000), the plan covers the remainder of the claims at 100%. Second, Medicare Advantage plans have set copayments for a variety of health care services such as office visits, labs, imaging, and ...
Why Advantage plans are bad?
disadvantage of medicare advantage plans
- Networks
- Referrals
- Prior Authorizations
- Frequent Expenses
- Out-of-Pocket Maximums
- Plan Changes
- Medicare is no longer managing your healthcare
How do I choose the best Medicare Advantage plan?
- Do your important physicians participate in any Medicare Advantage plans or do they only accept Original Medicare?
- What insurance is accepted by your preferred hospitals?
- Do you travel out of the area frequently? ...
- What is your risk tolerance? ...
- How about peace of mind? ...
What do you need to know about Medicare Advantage plans?
Excellus BlueCross/BlueShield Medicare Sales Representative Elisa Brescia is an expert in all things Medicare, and she spoke with News10NBC's Emily Putnam about what you need to know if you're consdiering making a change. Emily Putnam: Who do you think ...
See more

Where does the money come from for Medicare Advantage plans?
Three sources of revenue for Advantage plans include general revenues, Medicare premiums, and payroll taxes. The government sets a pre-determined amount every year to private insurers for each Advantage member. These funds come from both the HI and the SMI trust funds.
What is monthly payment for Medicare Advantage?
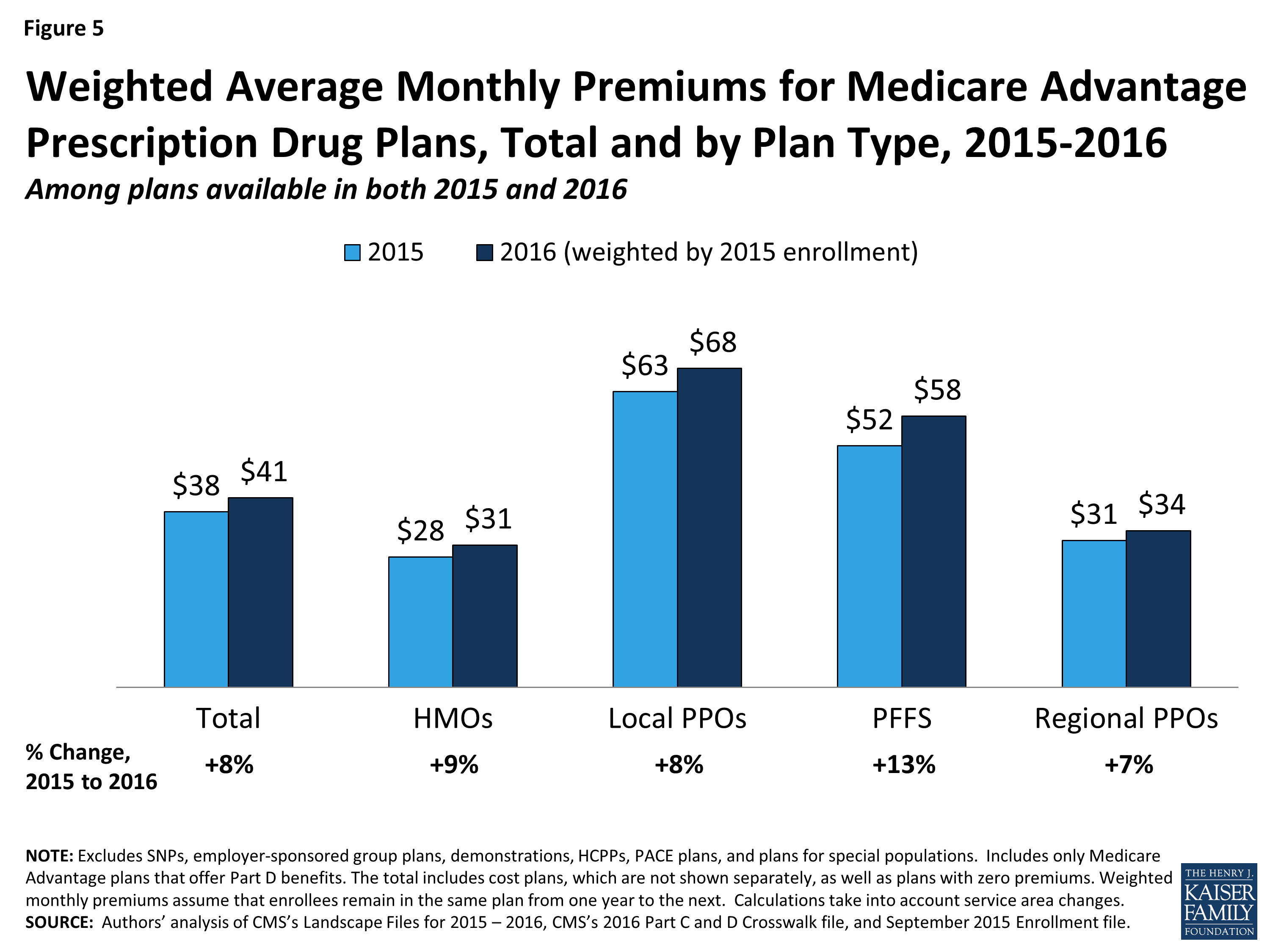
The average premium for a Medicare Advantage plan in 2021 was $21.22 per month. For 2022 it will be $19 per month. Although this is the average, some premiums cost $0, and others cost well over $100.
Are Medicare Advantage premiums deducted from Social Security?
Medicare Part B premiums must be deducted from Social Security benefits if the monthly benefit covers the deduction. If the monthly benefit does not cover the full deduction, the beneficiary is billed. Beneficiaries may elect deduction of Medicare Part C (Medicare Advantage) from their Social Security benefit.
What are the negatives to a Medicare Advantage plan?
The takeaway There are some disadvantages as well, including provider limitations, additional costs, and lack of coverage while traveling. Whether you choose original Medicare or Medicare Advantage, it's important to review healthcare needs and Medicare options before choosing your coverage.
Why is Medicare Advantage being pushed so hard?
Advantage plans are heavily advertised because of how they are funded. These plans' premiums are low or nonexistent because Medicare pays the carrier whenever someone enrolls. It benefits insurance companies to encourage enrollment in Advantage plans because of the money they receive from Medicare.
How do I get my $144 back from Medicare?
Even though you're paying less for the monthly premium, you don't technically get money back. Instead, you just pay the reduced amount and are saving the amount you'd normally pay. If your premium comes out of your Social Security check, your payment will reflect the lower amount.
How do you pay Medicare premiums?
4 ways to pay your Medicare premium bill:Pay online through your secure Medicare account (fastest way to pay). ... Sign up for Medicare Easy Pay. ... Pay directly from your savings or checking account through your bank's online bill payment service. ... Mail your payment to Medicare.
How much is taken out of your Social Security check for Medicare?
Medicare Part B (medical insurance) premiums are normally deducted from any Social Security or RRB benefits you receive. Your Part B premiums will be automatically deducted from your total benefit check in this case. You'll typically pay the standard Part B premium, which is $170.10 in 2022.
What is the $16 728 Social Security secret?
1:266:46My Review: Motley Fool's $16,728 Social Security Bonus - YouTubeYouTubeStart of suggested clipEnd of suggested clipIf you've read any of their articles you've probably seen this it says the sixteen thousand sevenMoreIf you've read any of their articles you've probably seen this it says the sixteen thousand seven hundred and twenty eight dollar social security bonus most retirees completely overlook.
How does Boomer benefits get paid?
Medicare brokers such as Boomer Benefits get paid by the insurance companies they represent. And you pay exactly the same rate for your insurance if you use a Medicare consultant (broker). There is no extra fee or cost for enrolling through a broker.
Can you switch back to Medicare from Medicare Advantage?
Yes, you can elect to switch to traditional Medicare from your Medicare Advantage plan during the Medicare Open Enrollment period, which runs from October 15 to December 7 each year. Your coverage under traditional Medicare will begin January 1 of the following year.
Do Medicare Advantage plan premiums increase with age?
The way they set the price affects how much you pay now and in the future. Generally the same monthly premium is charged to everyone who has the Medigap policy, regardless of age. Your premium isn't based on your age. Premiums may go up because of inflation and other factors, but not because of your age.
What is Medicare Advantage Plan?
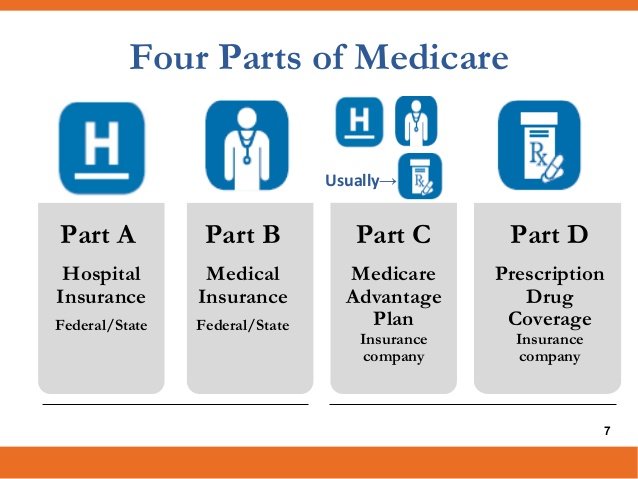
Medicare Advantage Plan (Part C) A type of Medicare health plan offered by a private company that contracts with Medicare. Medicare Advantage Plans provide all of your Part A and Part B benefits, excluding hospice. Medicare Advantage Plans include: Health Maintenance Organizations. Preferred Provider Organizations.
What is Medicare premium?
premium. The periodic payment to Medicare, an insurance company, or a health care plan for health or prescription drug coverage. . Many Medicare Advantage Plans have a $0 premium. If you enroll in a plan that does charge a premium, you pay this in addition to the Part B premium. Whether the plan pays any of your monthly.
What is out of network Medicare?
out-of-network. A benefit that may be provided by your Medicare Advantage plan. Generally, this benefit gives you the choice to get plan services from outside of the plan's network of health care providers. In some cases, your out-of-pocket costs may be higher for an out-of-network benefit. .
What is the difference between Medicare and Original Medicare?
Original Medicare. Original Medicare is a fee-for-service health plan that has two parts: Part A (Hospital Insurance) and Part B (Medical Insurance). After you pay a deductible, Medicare pays its share of the Medicare-approved amount, and you pay your share (coinsurance and deductibles). .
What is a medicaid?
Whether you have. Medicaid. A joint federal and state program that helps with medical costs for some people with limited income and resources. Medicaid programs vary from state to state, but most health care costs are covered if you qualify for both Medicare and Medicaid.
What is covered benefits?
benefits. The health care items or services covered under a health insurance plan. Covered benefits and excluded services are defined in the health insurance plan's coverage documents. and if the plan charges for it. The plan's yearly limit on your out-of-pocket costs for all medical services. Whether you have.
What is a copayment?
A copayment is usually a set amount, rather than a percentage. For example, you might pay $10 or $20 for a doctor's visit or prescription drug. An amount you may be required to pay as your share of the cost for services after you pay any deductibles. Coinsurance is usually a percentage (for example, 20%).
Medicare Advantage by the percentages
Required minimum medical-loss ratio (share of revenue spent on member benefits; any excess must be refunded to CMS)
2020 foresight: an MA payment timeline
As this magazine is published, the process that will determine the amounts of monthly capitated payments to Medicare Advantage (MA) plans next year, in 2020, has already begun. Here are highlights:
What is Medicare Advantage?
Medicare Advantage plans are managed care, which means you might need prior authorization for a medication, you may need a referral to see a specialist, and you may have to try a cheaper treatment plan before your plan will approve a more expensive one. That’s how Medicare Advantage plans manage their costs.
Is Medicare Advantage a low premium?
Most Medicare Advantage plans are paid enough by the government to offer very low – sometimes even $0 premium plans – in addition to extra benefits that go above and beyond what Medicare regularly covers. For example, you might get some dental, vision, and fitness benefits.
What is Medicare Advantage?
The amount you are required to pay for each health care visit or service. Medicare Advantage plans typically include cost-sharing measures such as copayments and coinsurance, and the amounts of these costs can correlate with that of the premium. The type of plan.
What is a Medicare Savings Account?
A Medicare Savings Account (MSA) is a type of Medicare Advantage plan that deposits money into a savings account that can be used to pay for out-of-pocket expenses prior to meeting your deductible.
What to look for when shopping for Medicare Advantage?
When you are shopping for a Medicare Advantage plan, you may consider features such as a plan’s range of benefits and possible network rules. But above all else, perhaps the biggest thing you might consider is the cost of a plan. When it comes to Original Medicare (Medicare Part A and Part B), the cost of premiums is standardized across the board.
How to save money on medicaid?
Saving money with Medicare Advantage 1 If you qualify for Medicaid, your Medicaid benefits can be used to help pay your Medicare Advantage premiums. 2 A Medicare Savings Account (MSA) is a type of Medicare Advantage plan that deposits money into a savings account that can be used to pay for out-of-pocket expenses prior to meeting your deductible. 3 If your Medicare Advantage plan includes a doctor and/or pharmacy network, you can save a considerable amount of money by staying within that network when receiving services. 4 Some Medicare Advantage plans may include extra health perks such as gym memberships. There is even the possibility of Medicare Advantage plans soon covering expenses like the cost of air conditioners, home-delivered meals and transportation.
How much does vision insurance cost?
Vision insurance can typically cost around $20 per month or less. 3. Hearing plans. Unlike dental and vision insurance, hearing insurance plans are not a common insurance product. Some hearing aid companies may offer extended warranties, but the warranties apply only to the hearing aid product itself.
Which state has the lowest Medicare premium?
A closer look at 2021 data also reveals: Nevada has the lowest average monthly premium for Medicare Advantage Prescription Drug (MAPD) plans at $11.58 per month. The highest average MAPD monthly premium is in North Dakota, at $76.33 per month.
Does Medicare Advantage cover dental?
While a Medicare Advantage plan by law must cover the same benefits as Medicare Part A and Medicare Part B , benefits like prescription drugs, dental, vision and hearing can be covered at varying degrees (or not at all).
What is an HMO plan?
Health Maintenance Organization (HMO) plan is a type of Medicare Advantage Plan that generally provides health care coverage from doctors, other health care providers, or hospitals in the plan’s network (except emergency care, out-of-area urgent care, or out-of-area dialysis). A network is a group of doctors, hospitals, and medical facilities that contract with a plan to provide services. Most HMOs also require you to get a referral from your primary care doctor for specialist care, so that your care is coordinated.
What happens if you get a health care provider out of network?
If you get health care outside the plan’s network, you may have to pay the full cost. It’s important that you follow the plan’s rules, like getting prior approval for a certain service when needed. In most cases, you need to choose a primary care doctor. Certain services, like yearly screening mammograms, don’t require a referral. If your doctor or other health care provider leaves the plan’s network, your plan will notify you. You may choose another doctor in the plan’s network. HMO Point-of-Service (HMOPOS) plans are HMO plans that may allow you to get some services out-of-network for a higher copayment or coinsurance. It’s important that you follow the plan’s rules, like getting prior approval for a certain service when needed.
Do providers have to follow the terms and conditions of a health insurance plan?
The provider must follow the plan’s terms and conditions for payment, and bill the plan for the services they provide for you. However, the provider can decide at every visit whether to accept the plan and agree to treat you.
Can a provider bill you for PFFS?
The provider shouldn’t provide services to you except in emergencies, and you’ll need to find another provider that will accept the PFFS plan .However, if the provider chooses to treat you, then they can only bill you for plan-allowed cost sharing. They must bill the plan for your covered services. You’re only required to pay the copayment or coinsurance the plan allows for the types of services you get at the time of the service. You may have to pay an additional amount (up to 15% more) if the plan allows providers to “balance bill” (when a provider bills you for the difference between the provider’s charge and the allowed amount).
Where does Medicare Advantage money come from?
The money that the government pays to Medicare Advantage providers for capitation comes from two U.S. Treasury funds.
What is Medicare Advantage Reimbursement?
Understanding Medicare Advantage Reimbursement. The amount the insurance company receives from the government for you as a beneficiary is dependent upon your individual circumstances. As a beneficiary of a Medicare Advantage plan, if your monthly health care costs are less than what your insurance carrier receives as your capitation amount, ...
What is the second fund in Medicare?
The second fund is the Supplementary Medical Insurance Trust which pays for what is covered in Part B, Part D, and more. As a beneficiary enrolled in a Medicare Advantage plan, you will also be responsible for some of the costs of your healthcare.
How old do you have to be to get Medicare Advantage?
How Does Medicare Advantage Reimbursement Work? In the United States, you are eligible to enroll in a Medicare Advantage plan if you are either 65 years of age or older, are under 65 with certain disabilities.
Does Medicare Advantage cover dental?
Medicare Advantage plans must provide the same coverage as Parts A and B, but many offer additional benefits, such as vision and dental care, hearing exams, wellness programs, and Part D, prescription drug coverage.
Is Medicare Part C required?
Having a Medicare Part C plan is not a requirement for Medicare coverage, it is strictly an option many beneficiaries choose. If you decide to enroll in a Medicare Advantage plan, you are still enrolled in Medicare and have the same rights and protection that all Medicare beneficiaries have.
What is Medicare Advantage?
Medicare Advantage, a health plan provided by private insurance companies, is paid for by federal funding, subscriber premiums and co-payments. It includes the same coverage as the federal government’s Original Medicare program as well as additional supplemental benefits.
How is health insurance funded?
Treasury. The Hospital Insurance Trust Fund is funded by federal payroll taxes and income taxes from Social Security benefits.
What is Supplementary Medical Insurance Fund?
The Supplementary Medical Insurance Fund is composed of funds approved by Congress and Part B and Part D premiums paid by subscribers.
Is Medicare Advantage financed by monthly premiums?
Each insurance company is approved and contracted by Medicare and must fulfill guidelines for coverage as established by the government. Medicare Advantage plans are also financed by monthly premiums paid by subscribers. The premium amounts vary by company and plan.