The Coordination of Benefits program identifies the health benefits available to a person with Medicare, and coordinates the payment process to prevent mistaken payment of Medicare benefits. Medicare eligibility data are shared with other payers, and Medicare-paid medical claims are transmitted to supplemental insurers for secondary payment.
How does Medicare supplement insurance work with Medicare?
They only pay after Medicare, employer group health plans, and/or Medicare Supplement Insurance (Medigap) have paid. If you still have questions about who should pay or who should pay first: • Check your insurance policy or coverage. It may include rules about who pays first. • Call the Benefits Coordination & Recovery Center (BCRC) at
What is Medicare supplement insurance (Medigap) for retirees?
If you're retired, have Medicare and have group health plan coverage from a former employer, generally Medicare pays first. Your retiree coverage pays second. What's Medicare Supplement Insurance (Medigap)? Read about Medigap (Medicare Supplement Insurance), which helps pay some of the health care costs that Original Medicare doesn't cover.
How does Medicare work with other insurance?
Dec 01, 2021 · In the absence of an agreement, the person with Medicare is required to coordinate secondary or supplemental payment of benefits with any other insurers he or she may have in addition to Medicare. Ensures that the amount paid by plans in dual coverage situations does not exceed 100% of the total claim, to avoid duplicate payments.
Who pays first – Medicare or Medicare supplement insurance?
Medigap is Medicare Supplement Insurance that helps fill "gaps" in . Original Medicare and is sold by private companies. Original Medicare pays for much, but not all, of the cost for covered health care services and supplies. A Medicare Supplement Insurance (Medigap) policy can help pay some of the remaining health care costs, like: Copayments
How are Medicare and supplemental policies billed?
When you have Medicare and other health insurance, such as a Medicare Supplement insurance plan, each type of coverage is called a “payer.” The primary payer will pay what it owes on your health-care bills first and then send the balance to the secondary payer.
What is the relationship between Medigap insurance and Medicare?
A Medigap policy is different from a Medicare Advantage Plan. Those plans are ways to get Medicare benefits, while a Medigap policy only supplements your Original Medicare benefits. The periodic payment to Medicare, an insurance company, or a health care plan for health or prescription drug coverage.
Are Medicare Supplement plans secondary to Medicare?
Medicare Supplements provide extra coverage for what Medicare includes. Thus, your Medigap plan will always be secondary to Medicare. Supplemental insurance is available for what doesn't get coverage. For example, Part D is drug coverage, which is supplemental insurance.Oct 7, 2021
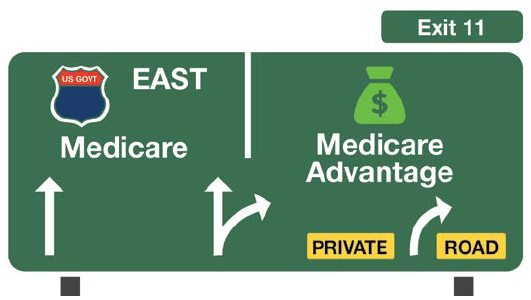
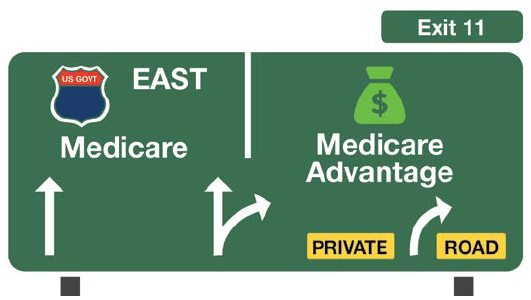
Is a Medicare Supplement plan the same as a Medicare Advantage Plan?
Medicare Advantage and Medicare Supplement are different types of Medicare coverage. You cannot have both at the same time. Medicare Advantage bundles Part A and B often with Part D and other types of coverage. Medicare Supplement is additional coverage you can buy if you have Original Medicare Part A and B.Oct 1, 2021
Why do doctors not like Medicare Advantage plans?
If they don't say under budget, they end up losing money. Meaning, you may not receive the full extent of care. Thus, many doctors will likely tell you they do not like Medicare Advantage plans because the private insurance companies make it difficult for them to get paid for the services they provide.
What is the downside to Medigap plans?
Some disadvantages of Medigap plans include: Higher monthly premiums. Having to navigate the different types of plans. No prescription coverage (which you can purchase through Plan D)
How are Medicare supplements divided?
Supplemental insurance plans are divided into categories with an alphabetic label. Medigap plans in tiers A through K provide the highest cost sharing benefits, while plans K through N plans provide less cost coverage.Jul 20, 2018
Is Medigap the same as supplemental?
Are Medigap and Medicare Supplemental Insurance the same thing? En español | Yes. Medigap or Medicare Supplemental Insurance is private health insurance that supplements your Medicare coverage by helping you pay your share of health care costs. You have to buy and pay for Medigap on your own.
Does Medigap pay Part A deductible?
Medigap, also known as Medicare Supplement plans, can help pay some of your out-of-pocket costs, including your Medicare Part A deductibles. These plans are sold through private insurers. There are eight standardized plans across 47 states and the District of Columbia.
Can I switch from a Medicare Supplement to an Advantage plan?
Can you switch from Medicare Supplement (Medigap) to Medicare Advantage? Yes. There can be good reasons to consider switching your Medigap plan. Maybe you're paying too much for benefits you don't need, or your health needs have changed and now you need more benefits.Jun 24, 2021
Can I drop my Medicare Advantage plan and go back to original Medicare?
Yes, you can elect to switch to traditional Medicare from your Medicare Advantage plan during the Medicare Open Enrollment period, which runs from October 15 to December 7 each year. Your coverage under traditional Medicare will begin January 1 of the following year.
What's the difference between a supplement and an Advantage plan?
Keep in mind that Medicare Supplement insurance plans can only be used to pay for Original Medicare costs; they can't be used with Medicare Advantage plans. In contrast, Medicare Advantage plans are an alternative to Original Medicare. If you enroll in a Medicare Advantage plan, you're still in the Medicare program.
How Medicare works with other insurance
Learn how benefits are coordinated when you have Medicare and other health insurance.
Retiree insurance
Read 5 things you need to know about how retiree insurance works with Medicare. If you're retired, have Medicare and have group health plan coverage from a former employer, generally Medicare pays first. Your retiree coverage pays second.
What's Medicare Supplement Insurance (Medigap)?
Read about Medigap (Medicare Supplement Insurance), which helps pay some of the health care costs that Original Medicare doesn't cover.
When can I buy Medigap?
Get the facts about the specific times when you can sign up for a Medigap policy.
How to compare Medigap policies
Read about different types of Medigap policies, what they cover, and which insurance companies sell Medigap policies in your area.
Medigap & travel
Read about which Medigap policies offer coverage when you travel outside the United States (U.S.).
What is Medicare investigation?
The investigation determines whether Medicare or the other insurance has primary responsibility for meeting the beneficiary's health care costs. Collecting information on Employer Group Health Plans and non-group health plans (liability insurance ...
What is BCRC in Medicare?
Benefits Coordination & Recovery Center (BCRC) - The BCRC consolidates the activities that support the collection, management, and reporting of other insurance coverage for beneficiaries. The BCRC takes actions to identify the health benefits available to a beneficiary and coordinates the payment process to prevent mistaken payment of Medicare benefits. The BCRC does not process claims, nor does it handle any GHP related mistaken payment recoveries or claims specific inquiries. The Medicare Administrative Contractors (MACs), Intermediaries and Carriers are responsible for processing claims submitted for primary or secondary payment.
Why do we need MSP records on CWF?
Establishing MSP occurrence records on CWF to keep Medicare from paying when another party should pay first. The CWF is a single data source for fiscal intermediaries and carriers to verify beneficiary eligibility and conduct prepayment review and approval of claims from a national perspective.
What is a COB plan?
Coordination of benefits (COB) allows plans that provide health and/or prescription coverage for a person with Medicare to determine their respective payment responsibilities (i.e., determine which insurance plan has the primary payment responsibility and the extent to which the other plans will contribute when an individual is covered by more than one plan).
What is the purpose of the MSP?
To report employment changes, or any other insurance coverage information. To report a liability, auto/no-fault, or workers’ compensation case. To ask a general MSP question. To ask a question regarding the MSP letters and questionnaires (i.e. Secondary Claim Development (SCD) questionnaire.)
Does Medicare pay a claim as a primary payer?
Where CMS systems indicate that other insurance is primary to Medicare, Medicare will not pay the claim as a primary payer and will return it to the provider of service with instructions to bill the proper party.
What is Medicare Advantage?
Medicaid. A joint federal and state program that helps with medical costs for some people with limited income and resources.
What is the difference between Medicare and Original Medicare?
Original Medicare. Original Medicare is a fee-for-service health plan that has two parts: Part A (Hospital Insurance) and Part B (Medical Insurance). After you pay a deductible, Medicare pays its share of the Medicare-approved amount, and you pay your share (coinsurance and deductibles). and is sold by private companies.
What is a Medigap policy?
Those plans are ways to get Medicare benefits, while a Medigap policy only supplements your Original Medicare benefits. The periodic payment to Medicare, an insurance company, or a health care plan for health or prescription drug coverage.
What happens if you buy a Medigap policy?
If you have Original Medicare and you buy a Medigap policy, here's what happens: Medicare will pay its share of the. Medicare-Approved Amount. In Original Medicare, this is the amount a doctor or supplier that accepts assignment can be paid. It may be less than the actual amount a doctor or supplier charges.
How many people does a Medigap policy cover?
for your Medigap policy. You pay this monthly premium in addition to the monthly Part B premium that you pay to Medicare. A Medigap policy only covers one person. If you and your spouse both want Medigap coverage, you'll each have to buy separate policies.
Can you cancel a Medigap policy?
This means the insurance company can't cancel your Medigap policy as long as you pay the premium. Some Medigap policies sold in the past cover prescription drugs. But, Medigap policies sold after January 1, 2006 aren't allowed to include prescription drug coverage.
Does Medicare cover all of the costs of health care?
Original Medicare pays for much, but not all, of the cost for covered health care services and supplies. A Medicare Supplement Insurance (Medigap) policy can help pay some of the remaining health care costs, like: Note: Medigap plans sold to people who are newly eligible for Medicare aren’t allowed to cover the Part B deductible.