How formularies are determined Health insurers and prescription benefit managers have pharmacy and therapeutics (P&T) committees made up of doctors, pharmacists, and other healthcare professionals that evaluate and select existing and new medications for the formulary.
What is a Medicare formulary?
A Medicare formulary is the list of prescription drugs that are covered by a particular Medicare Part D or Medicare Advantage plan. Each plan includes its own formulary that determines which drugs are covered by the plan and how much the drugs cost based on which tier the drug is classified into.
Why do I need a formulary for prescription drugs?
This helps make sure that people with different medical conditions can get the prescription drugs they need. All Medicare drug plans generally must cover at least 2 drugs per drug category, but plans can choose which drugs covered by Part D they will offer. The formulary might not include your specific drug.
Can drug plans remove brand name drugs from Medicare formularies?
For 2019 and beyond, drug plans offering Medicare prescription drug coverage (Part D) that meet certain requirements also can immediately remove brand name drugs from their formularies and replace them with new generic drugs, or they can change the cost or coverage rules for brand name drugs when adding new generic drugs.
Who approves the drugs on a health plan formulary?
Typically, a team of medical professionals approves the drugs on a health plan’s formulary based on safety, quality, and cost-effectiveness. The team is made up of pharmacists and physicians who review new and existing medications. Sometimes health plans choose not to cover a prescription drug. They do this if: The drug has a generic version.
What is a Medicare formulary?
Most Medicare drug plans have their own list of covered drugs, called a formulary. Plans cover both generic and brand-name prescription drugs. The formulary includes at least 2 drugs in the most commonly prescribed categories and classes.
How are drug tiers determined?
Tier 1: Least expensive drug options, often generic drugs. Tier 2: Higher price generic and lower-price brand-name drugs. Tier 3: Mainly higher price brand-name drugs. Tier 4: Highest cost prescription drugs.
How is formulary defined?
A list of prescription drugs covered by a prescription drug plan or another insurance plan offering prescription drug benefits. Also called a drug list.
How often is a formulary updated?
twice per yearFormulary changes typically occur twice per year. However, changes that have a positive impact for you — such as new medications or cost savings — may occur at any time. You can log in to optumrx.com at any time to check your medication coverage and lower cost options.
Who determines Medicare drug tiers?
Every plan creates its own formulary structure, decides which drugs it will cover and determines which tier a drug is on. One plan may cover a drug that another doesn't. The same drug may be on tier 2 in one plan's formulary and on tier 3 in a different plan's formulary.
What are the three types of formulary systems?
An open formulary has no limitation to access to a medication. Open formularies are generally large. A closed formulary is a limited list of medications. A closed formulary may limit drugs to specific physicians, patient care areas, or disease states via formulary restrictions.
How are formularies established?
The health plan generally creates this list by forming a pharmacy and therapeutics committee consisting of pharmacists and physicians from various medical specialties. This committee evaluates and selects new and existing medications for what is called the (health plan's) formulary.
What are the two types of formularies?
Other Types of Formularies. While “open” and “closed” formularies typically are used to denote the spectrum of evaluation, from a passive to active process, other permutations of formularies are known to exist.
Which committee develops a formulary for an institution?
The P&T committee is responsible for developing, managing, updating and administering the formulary. The P&T committee also designs and implements formulary system policies on utilization and access to medications.
Who manages formulary?
Health care practitioners serve many functions in the formulary management process. Pharmacists often lead formulary management initiatives, coordinate P&T committee tasks and make recommendations based on sound clinical evidence.
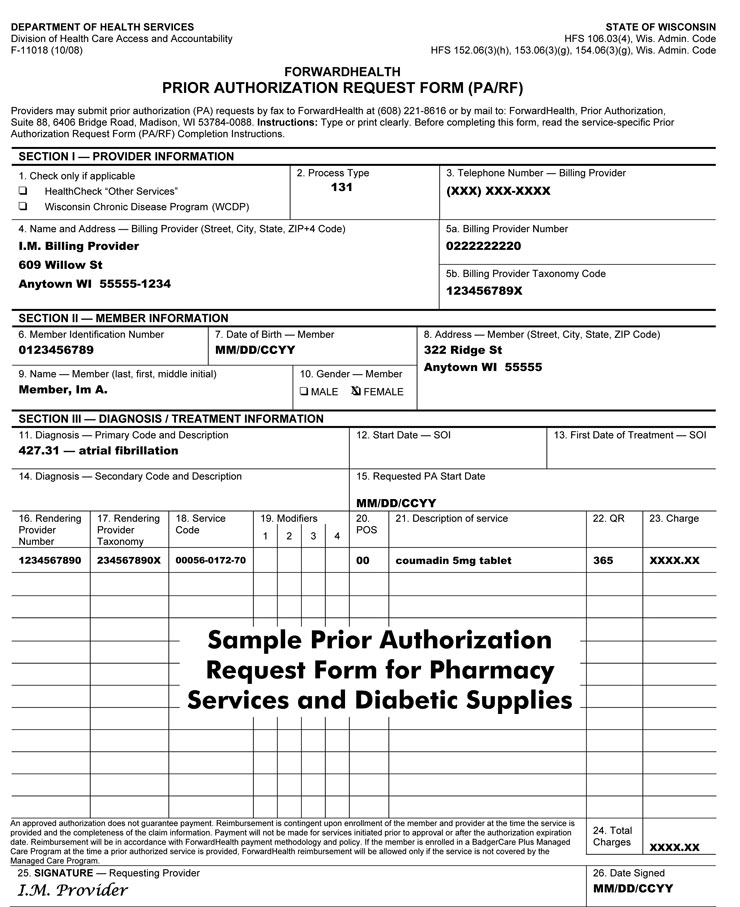
What are formulary changes?
Formulary changes happen from time to time if drugs are: Replaced by a new generic drug; or, Clinical restrictions are added, including, but not limited to, prior authorization, quantity limits or step therapy.
Why are drugs removed from formulary?
Your health insurance plan's Pharmacy & Therapeutics Committee might exclude a drug from its drug formulary a few common reasons: The health plan wants you to use a different drug in that same therapeutic class. The drug is available over-the-counter. The drug hasn't been approved by the U.S. FDA or is experimental.
What is a drug formulary?
A drug formulary is a list of medications covered by a Medicare drug plan. Here are 7 facts about Medicare drug formularies that every beneficiary should know. A Medicare formulary is the list of prescription drugs that are covered by a particular Medicare Part D or Medicare Advantage plan. Each plan includes its own formulary ...
What is tier 1 drug?
Drugs on a Medicare formulary are divided into tiers that determine the cost paid by beneficiaries. For example, a tier 1 drug might consist of low-cost, generic drugs and require only a small copayment in order to fill a prescription.
Does Medicare have to include certain drugs?
You can also request to pay a lower amount for a covered drug. 5. Each formulary must include certain drugs. All Medicare formularies generally must include coverage for at least two different drugs within most drug categories, and they must include all available drugs for the following categories: HIV/AIDS treatments.
Can Medicare formulary change?
A Medicare formulary can change throughout the year. Drugs may be added or removed from the market at any time, and therefore drugs may be added or removed from a plan’s formulary. Drugs may also remain for sale on the market but be removed from a plan’s formulary for a variety of reasons.
Does Medicare have restrictions on prescription drugs?
All Medicare plans with prescription drug coverage must make sure that members have access to all medically necessary drugs listed on their formulary. 7. There are restrictions on some drugs on a formulary. Some drugs on a Medicare formulary come with certain types of restrictions, such as: Prior authorization.
How to know what medications are in Medicare Part D?
How to Know What Medications are in a Medicare Part D Formulary. If you have a health insurance agent, they can assist in finding your plan’s formulary list. You can check insurance carrier websites to view the drug formularies they offer. Those with Medicare are eligible for a drug plan and should enroll as soon as possible.
What is formulary exception?
A Formulary Exception is a form of a request to determine coverage. By obtaining an exception, you may be able to get a drug that’s not on your plan’s formulary or ask your plan to bypass step therapy or prior authorizations.
What does a doctor's report state?
If you’re seeking a tiering exception, your doctor’s report must state that the preferred medications would adversely affect you. If you’re trying to obtain a formulary exception, your doctor’s statement must indicate that the non-formulary drug is necessary.
What is Medicare Part D?
The Medicare Part D formulary is a list of drugs that have coverage under your policy. The formulary must include at least two drugs per category, and the insurance company can choose the options.
Can I pay for a drug yourself?
You may pay for the medication yourself. But, sometimes, you can find a manufacturer coupon to help cover the cost. Or, you can file an appeal or request a formulary exception. Then, during AEP, you can change your Part D plan.
Can a doctor prescribe a prescription?
A doctor prescribes a prescription, but it requires prior authorization or step therapy; however, you don’t feel you can meet the requirements. Your plan removes your medication from the formulary, and there aren’t other drugs you can use.
Is Medicare Part D 5 star?
Medicare Part D plans have a star-rating system similar to Medicare Advantage. Many locations don’t have 5-star plans, but some areas will have those options. The best Part D plan in 2021 varies by county; in some areas, Cigna may have higher ratings, whereas Humana could have higher ratings in other areas.
What do pharmacists do when filling prescriptions?
When you fill a prescription at the pharmacy, Medicare drug plans and pharmacists routinely check to make sure the prescription is correct, that there are no interactions, and that the medication is appropriate for you. They also conduct safety reviews to monitor the safe use of opioids and other frequently abused medications. These reviews are especially important if you have more than one doctor who prescribes these drugs. In some cases, the Medicare drug plan or pharmacist may need to first talk to your doctor before the prescription can be filled.
What to do if your prescription is not filled?
If your pharmacy can’t fill your prescription as written, the pharmacist will give you a notice explaining how you or your doctor can call or write to your plan to ask for a coverage decision. If your health requires it, you can ask the plan for a fast coverage decision. You may also ask your plan for an exception to its rules before you go to the pharmacy, so you’ll know if your plan will cover the medication. Visit Medicare.gov/medicare-prescription-drug-coverage-appeals to learn how to ask for an exception.
Does Medicare cover prescription drugs?
Medicare drug plans have contracts with pharmacies that are part of the plan’s “network.” If you go to a pharmacy that isn’t in your plan’s network, your plan might not cover your drugs. Along with retail pharmacies, your plan’s network might include preferred pharmacies, a mail-order program, or an option for retail pharmacies to supply a 2- or 3-month supply.
Does Medicare cover opioids?
Some Medicare drug plans will have a drug management program to help patients who are at risk for prescription drug abuse. If you get opioids from multiple doctors or pharmacies, your plan may talk with your doctors to make sure you need these medications and that you’re using them appropriately. If your Medicare drug plan decides your use of prescription opioids and benzodiazepines may not be safe, the plan will send you a letter in advance. This letter will tell you if the plan will limit coverage of these drugs for you, or if you’ll be required to get the prescriptions for these drugs only from a doctor or pharmacy that you select.
Prescription Drugs Not Covered by a Health Plan
Understanding your health plan’s formulary is an important part of understanding your overall benefits because your plan might only pay for medications on the “preferred” list that they’ve developed. Your health plan may exclude a drug from the formulary for several reasons, including:
What Is a Formulary Tier?
Tiers are the different cost levels health plan members pay for medications. Your employer or your health plan assigns each tier a unique cost, which is the amount you will pay when filling a prescription. Let’s use a typical health plan with four tiers to illustrate how formulary tiers usually work.
Formulary Restrictions
Most health plan formularies have procedures to limit or restrict certain medications to encourage doctors to prescribe certain medications appropriately and save money by preventing medication overuse or abuse. Some common restrictions include:
Discuss the Formulary With Your Healthcare Provider
There are exceptions to the rules when your health plan’s formulary doesn’t include certain medications, especially when this lapse might lead you to use a less effective drug or one that could result in a harmful medical event. As a plan member, you can request coverage for a medication not listed on the formulary.
What is a formulary in medicine?
formulary is more than a list of approved medications. A formulary must consist of drugs that will provide patients with a clinically appropriate medication for the course of treatment established by the physician. Consistent with industry standards/practices, the formulary is supported by a system of care management tools to consistently provide patients with access to medications that have been demonstrated to be safe, effective, and affordable, while maintaining and improving quality patient care. To ensure that Medicare prescription drug plans are following best practices, the CMS formulary review will follow four important principles.
What is the MMA in Medicare?
The addition of a prescription drug benefit to Medicare as a result of the MMA represents a landmark change to the Medicare program, a change that will significantly improve the healthcare coverage available to millions of Medicare beneficiaries. In the final regulation, we have included policies, such as formulary requirements and exceptions and appeals processes, to assure that beneficiaries have access to covered drugs that are medically necessary for their condition while enabling plans to design and manage their formularies to provide the most affordable benefit possible. We are also adjusting the payments to drug plans based on the expected costs of their enrollees, as well as implementing many other steps to limit the financial risk facing drug plans. Together, our goal is to provide a foundation for fair competition to offer high-quality coverage at the lowest cost to all types of Medicare beneficiaries, and to reward plans that focus on this critical policy goal.
Does CMS review drug lists?
Regardless of the classification system chosen, CMS will review and approve drug lists that are consistent with best practice formularies currently in widespread use today. The following paragraphs describe the multiple checks that will be utilized as part of the drug list review.
How many drugs does Medicare cover?
All Medicare drug plans generally must cover at least 2 drugs per drug category, but plans can choose which drugs covered by Part D they will offer. The formulary might not include your specific drug. However, in most cases, a similar drug should be available.
How many prescription drugs are covered by Medicare?
Plans include both brand-name prescription drugs and generic drug coverage. The formulary includes at least 2 drugs in the most commonly prescribed categories and classes. This helps make sure that people with different medical conditions can get the prescription drugs they need. All Medicare drug plans generally must cover at least 2 drugs per ...
What is formulary exception?
A formulary exception is a drug plan's decision to cover a drug that's not on its drug list or to waive a coverage rule. A tiering exception is a drug plan's decision to charge a lower amount for a drug that's on its non-preferred drug tier.
What happens if you don't use a drug on Medicare?
If you use a drug that isn’t on your plan’s drug list, you’ll have to pay full price instead of a copayment or coinsurance, unless you qualify for a formulary exception. All Medicare drug plans have negotiated to get lower prices for the drugs on their drug lists, so using those drugs will generally save you money.
What does Medicare Part D cover?
All plans must cover a wide range of prescription drugs that people with Medicare take, including most drugs in certain protected classes,” like drugs to treat cancer or HIV/AIDS. A plan’s list of covered drugs is called a “formulary,” and each plan has its own formulary.
What is a tier in prescription drug coverage?
Tiers. To lower costs, many plans offering prescription drug coverage place drugs into different “. tiers. Groups of drugs that have a different cost for each group. Generally, a drug in a lower tier will cost you less than a drug in a higher tier. ” on their formularies. Each plan can divide its tiers in different ways.
What is a drug plan's list of covered drugs called?
A plan’s list of covered drugs is called a “formulary,” and each plan has its own formulary. Many plans place drugs into different levels, called “tiers,” on their formularies. Drugs in each tier have a different cost. For example, a drug in a lower tier will generally cost you less than a drug in a higher tier.
The basics
Navigating your health insurance coverage can feel like a drive through dense fog or heavy rain. It’s hard to see due to lack of clarity and visibility — especially when it comes to medication coverage. That’s why understanding your plan’s prescription drug formulary is critical on your journey to better health and saving money.
What is a drug formulary?
A formulary is a list of generic and brand name prescription drugs covered by your health plan. Your health plan may only help you pay for the drugs listed on its formulary. It’s their way of providing a wide range of effective medications at the lowest possible cost.
What is a tier?
Your health plan’s formulary is divided into three or four categories. These categories are called tiers. Drugs are placed in tiers based on the type of drug: generic, preferred brand, non-preferred brand, and specialty. Here’s what typical formulary tiers look like:
How are they created and why do they change?
Typically, a team of medical professionals approves the drugs on a health plan’s formulary based on safety, quality, and cost-effectiveness. The team is made up of pharmacists and physicians who review new and existing medications.
Can my healthcare provider access my formulary?
Yes and no. Many health plans share their formularies with healthcare providers. Others don’t, leaving it up to you to take your prescription needs into your own hands. Here’s what you can do:
What should I consider when choosing a health plan?
When shopping for a health plan, there’s a wide range of variables to consider. You may ask questions like, “Can I afford the monthly premium?” and “Can I continue to see my favorite healthcare provider?”