How are they created and why do they change? Typically, a team of medical professionals approves the drugs on a health plan’s formulary based on safety, quality, and cost-effectiveness. The team is made up of pharmacists and physicians who review new and existing medications.
What are the rules of Medicare?
- You must have Medicare Part A and Part B.
- A Medigap policy is different from a Medicare Advantage Plan. ...
- You pay the private insurance company a monthly premium The periodic payment to Medicare, an insurance company, or a health care plan for health or prescription drug coverage. ...
- A Medigap policy only covers one person. ...
What is the Medicare Part D formulary?
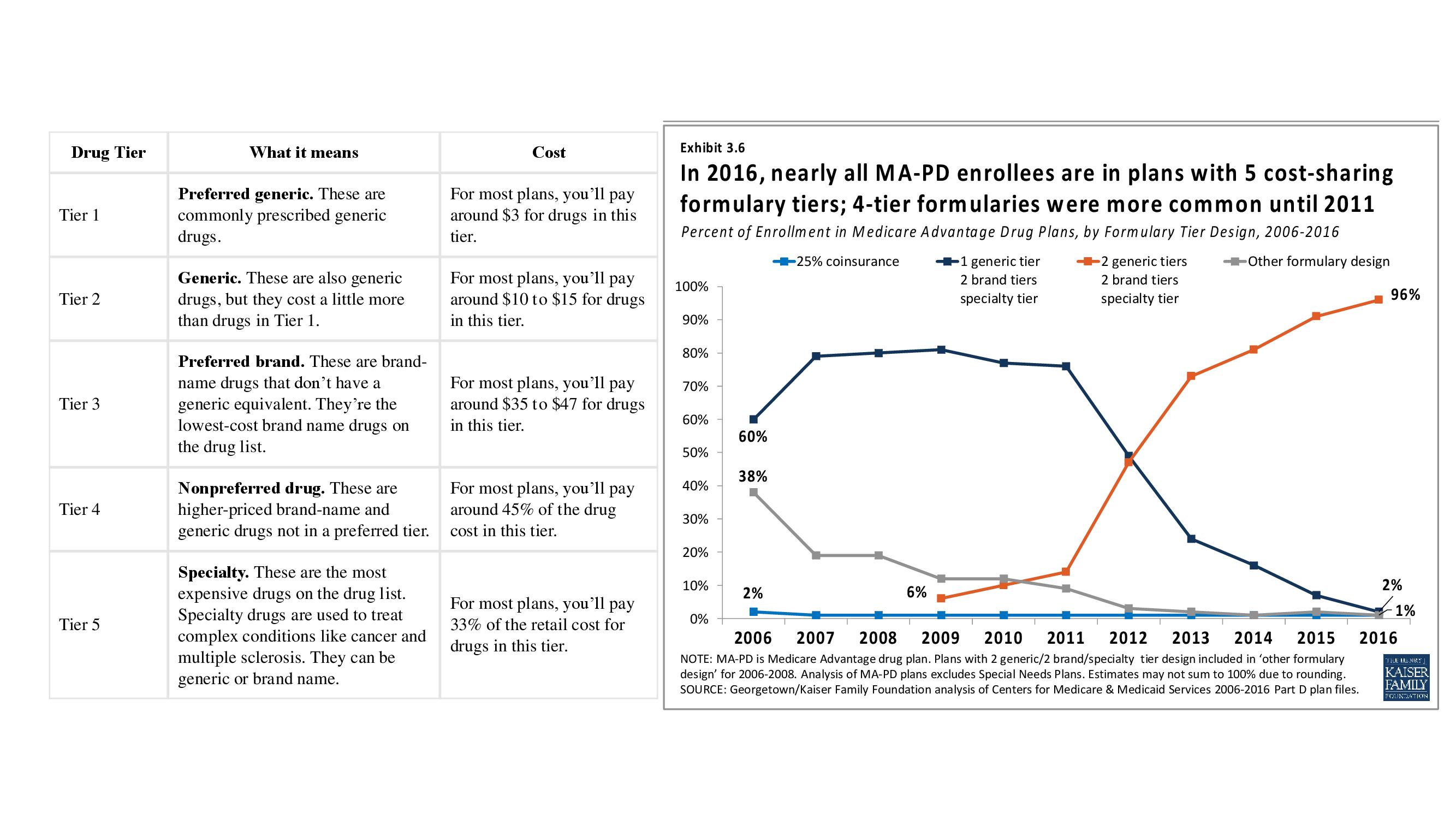
- Tier 1: Preferred generic drugs
- Tier 2: Generic drugs
- Tier 3: Preferred brand drugs and select insulin drugs
- Tier 4: Non-preferred drugs
- Tier 5: Specialty drugs
What is formulary drug list?
A formulary drug or drug formulary is a list of prescription drugs that includes both generic and brand names. These are used by doctors or practitioners to identify drugs that have the greatest overall value. The formulary is maintained by an independent committee of practicing physicians and pharmacists.
What is a drug formulary and tier pricing?
This formulary outlines the most commonly prescribed medications covered under your plan’s prescription drug benefits. The formulary is also known as the Prescription Drug List (PDL). A formulary identifies the drugs available for certain conditions and organizes them into cost levels, also known as tiers.

How is formulary determined?
Formulary Development The medications and related products listed on a formulary are determined by a pharmacy and therapeutics (P&T) committee or an equivalent entity. P&T committees are comprised of primary care and specialty physicians, pharmacists and other professionals in the health care field.
What is a Medicare formulary?
Most Medicare drug plans have their own list of covered drugs, called a formulary. Plans cover both generic and brand-name prescription drugs. The formulary includes at least 2 drugs in the most commonly prescribed categories and classes.
Who manages the formulary system?
pharmacy and therapeuticsFormulary systems are managed by the pharmacy and therapeutics (P&T) committee and provide a process for using medications and related drug products to offer safe, cost-effective, and beneficial outcomes for patients. Each medication used in the formulary system is chosen based on evidence-based research.
Are all Medicare Part D formularies the same?
Each plan can divide its tiers in different ways. Each tier costs a different amount. Generally, a drug in a lower tier will cost you less than a drug in a higher tier. A type of Medicare prescription drug coverage determination.
How often are formularies updated?
There are also some instances where the same product can be made by two or more manufacturers, but greatly vary in cost. In these instances, only the lower cost product may be covered. How often is the Formulary updated? Formulary changes typically occur twice per year.
What are the three types of formulary systems?
An open formulary has no limitation to access to a medication. Open formularies are generally large. A closed formulary is a limited list of medications. A closed formulary may limit drugs to specific physicians, patient care areas, or disease states via formulary restrictions.
What are the two types of formularies?
Other Types of Formularies. While “open” and “closed” formularies typically are used to denote the spectrum of evaluation, from a passive to active process, other permutations of formularies are known to exist.
What are the parts of formulary?
In accordance with these objectives, the formulary- should consist of three main parts: Part One—Information on hospital policies and'procedures concerning drugs. Part Two—Drug products listing and Part Three—Special information. A more detailed look at each section follows.
What is a managed formulary?
What is a managed formulary? Unlike an open formulary, which automati- cally covers all drugs requiring a prescrip- tion, a managed formulary covers drugs based on a set of review criteria.
Why do doctors not like Medicare Advantage plans?
If they don't say under budget, they end up losing money. Meaning, you may not receive the full extent of care. Thus, many doctors will likely tell you they do not like Medicare Advantage plans because private insurance companies make it difficult for them to get paid for their services.
What type of medications are not covered on a formulary?
However, plans usually do not cover:Weight loss or weight gain drugs.Drugs for cosmetic purposes or hair growth.Fertility drugs.Drugs for sexual or erectile dysfunction.Over-the-counter drugs.
What is the CMS formulary Reference File?
Guidance for frequently asked questions pertain to CMS' Formulary Reference File (FRF). The FRF serves as a listing of drug products that can be included on Part D sponsors' Health Plan Management System (HPMS) formulary files that are submitted to CMS for review and approval.
What is a drug formulary?
A drug formulary is a list of medications covered by a Medicare drug plan. Here are 7 facts about Medicare drug formularies that every beneficiary should know. A Medicare formulary is the list of prescription drugs that are covered by a particular Medicare Part D or Medicare Advantage plan. Each plan includes its own formulary ...
What is tier 1 drug?
Drugs on a Medicare formulary are divided into tiers that determine the cost paid by beneficiaries. For example, a tier 1 drug might consist of low-cost, generic drugs and require only a small copayment in order to fill a prescription.
Does Medicare have to include certain drugs?
You can also request to pay a lower amount for a covered drug. 5. Each formulary must include certain drugs. All Medicare formularies generally must include coverage for at least two different drugs within most drug categories, and they must include all available drugs for the following categories: HIV/AIDS treatments.
Can Medicare formulary change?
A Medicare formulary can change throughout the year. Drugs may be added or removed from the market at any time, and therefore drugs may be added or removed from a plan’s formulary. Drugs may also remain for sale on the market but be removed from a plan’s formulary for a variety of reasons.
Does Medicare have restrictions on prescription drugs?
All Medicare plans with prescription drug coverage must make sure that members have access to all medically necessary drugs listed on their formulary. 7. There are restrictions on some drugs on a formulary. Some drugs on a Medicare formulary come with certain types of restrictions, such as: Prior authorization.
Prescription Drugs Not Covered by a Health Plan
Understanding your health plan’s formulary is an important part of understanding your overall benefits because your plan might only pay for medications on the “preferred” list that they’ve developed. Your health plan may exclude a drug from the formulary for several reasons, including:
What Is a Formulary Tier?
Tiers are the different cost levels health plan members pay for medications. Your employer or your health plan assigns each tier a unique cost, which is the amount you will pay when filling a prescription. Let’s use a typical health plan with four tiers to illustrate how formulary tiers usually work.
Formulary Restrictions
Most health plan formularies have procedures to limit or restrict certain medications to encourage doctors to prescribe certain medications appropriately and save money by preventing medication overuse or abuse. Some common restrictions include:
Discuss the Formulary With Your Healthcare Provider
There are exceptions to the rules when your health plan’s formulary doesn’t include certain medications, especially when this lapse might lead you to use a less effective drug or one that could result in a harmful medical event. As a plan member, you can request coverage for a medication not listed on the formulary.
What do pharmacists do when filling prescriptions?
When you fill a prescription at the pharmacy, Medicare drug plans and pharmacists routinely check to make sure the prescription is correct, that there are no interactions, and that the medication is appropriate for you. They also conduct safety reviews to monitor the safe use of opioids and other frequently abused medications. These reviews are especially important if you have more than one doctor who prescribes these drugs. In some cases, the Medicare drug plan or pharmacist may need to first talk to your doctor before the prescription can be filled.
What to do if your prescription is not filled?
If your pharmacy can’t fill your prescription as written, the pharmacist will give you a notice explaining how you or your doctor can call or write to your plan to ask for a coverage decision. If your health requires it, you can ask the plan for a fast coverage decision. You may also ask your plan for an exception to its rules before you go to the pharmacy, so you’ll know if your plan will cover the medication. Visit Medicare.gov/medicare-prescription-drug-coverage-appeals to learn how to ask for an exception.
Does Medicare cover prescription drugs?
Medicare drug plans have contracts with pharmacies that are part of the plan’s “network.” If you go to a pharmacy that isn’t in your plan’s network, your plan might not cover your drugs. Along with retail pharmacies, your plan’s network might include preferred pharmacies, a mail-order program, or an option for retail pharmacies to supply a 2- or 3-month supply.
Does Medicare cover opioids?
Some Medicare drug plans will have a drug management program to help patients who are at risk for prescription drug abuse. If you get opioids from multiple doctors or pharmacies, your plan may talk with your doctors to make sure you need these medications and that you’re using them appropriately. If your Medicare drug plan decides your use of prescription opioids and benzodiazepines may not be safe, the plan will send you a letter in advance. This letter will tell you if the plan will limit coverage of these drugs for you, or if you’ll be required to get the prescriptions for these drugs only from a doctor or pharmacy that you select.
What is a formulary in Medicare?
A formulary is the list of medications that are covered by your plan. Understanding how a formulary works is an essential part of choosing your plan and taking full advantage of its benefits. Within the list of covered drugs, providers break down the category of coverage into tiers. Each tier helps designate the costs of any particular medication. While a particular medication can be on different tiers in different plans, you’ll consistently find the preferred generic medications are classified as Tier 1 and the more expensive brand medications will be found in Tiers 3-5. If you can resolve your medical conditions with generic medications, which are typically found in Tiers 1 and 2, you can keep your costs to the lowest levels.
Is Medicare Part A or D?
Medicare Part A (hospital coverage) and Medicare Part B (medical coverage) are offered through the federal government, but Medicare Part D prescription drug coverage is privatized. Through private insurance companies approved by the government, beneficiaries can either purchase a stand-alone Part D plan (to complement their Original Medicare coverage) or a Medicare Advantage plan that bundles Original Medicare with drug coverage. Each participating plan’s list of covered drugs will vary by tier, copays and coinsurance. These costs, which often also include a deductible, will typically change year after year, so paying close attention to the changes in your Part D benefits is very important. According to Medicare.gov, “All plans must cover a wide range of prescription drugs that people with Medicare take, including most drugs in certain protected classes, like drugs to treat cancer or HIV/AIDs.”
What is a formulary?
A formulary is a list of generic and brand name drugs that are covered by a health plan. Pharmacy Benefit Dimensions (PBD) offers several formulary options for both our self-funded and Medicare Part D Prescription Drug Plan (PDP) Employer Group Waiver Plan (EGWP) clients.
What is a tier?
A formulary is divided into various categories, or tiers. Drugs are placed in tiers based on the drug type. Drug types include generic, preferred brand, non-preferred brand and specialty. At PBD, we offer a variety of formulary options based on a tiering structure including:
How does this benefit our clients?
Our clinical team utilizes a value-based approach when making formulary decisions which focuses on low-cost therapeutic alternatives such as generic medications, to help balance efficacy, safety and cost-effectiveness.
What is a formulary in medicine?
formulary is more than a list of approved medications. A formulary must consist of drugs that will provide patients with a clinically appropriate medication for the course of treatment established by the physician. Consistent with industry standards/practices, the formulary is supported by a system of care management tools to consistently provide patients with access to medications that have been demonstrated to be safe, effective, and affordable, while maintaining and improving quality patient care. To ensure that Medicare prescription drug plans are following best practices, the CMS formulary review will follow four important principles.
What is the MMA in Medicare?
The addition of a prescription drug benefit to Medicare as a result of the MMA represents a landmark change to the Medicare program, a change that will significantly improve the healthcare coverage available to millions of Medicare beneficiaries. In the final regulation, we have included policies, such as formulary requirements and exceptions and appeals processes, to assure that beneficiaries have access to covered drugs that are medically necessary for their condition while enabling plans to design and manage their formularies to provide the most affordable benefit possible. We are also adjusting the payments to drug plans based on the expected costs of their enrollees, as well as implementing many other steps to limit the financial risk facing drug plans. Together, our goal is to provide a foundation for fair competition to offer high-quality coverage at the lowest cost to all types of Medicare beneficiaries, and to reward plans that focus on this critical policy goal.
What is CMS MMA?
In support of the Medicare Modernization Act (MMA), CMS is establishing a systems interface within the Health Plan Management System (HPMS) to enable MA-PD plans and PDPs to submit their formularies electronically. This functionality will provide for the upload and receipt of the formulary file, exceptions and notes file, prior authorization supplemental data and step therapy supplemental data, as defined by CMS. It will also allow CMS to provide more timely, systematic, and consistent feedback to plans regarding their formulary practices.
Does CMS review drug lists?
Regardless of the classification system chosen, CMS will review and approve drug lists that are consistent with best practice formularies currently in widespread use today. The following paragraphs describe the multiple checks that will be utilized as part of the drug list review.
What is Medicare approved amount?
Medicare-Approved Amount. In Original Medicare, this is the amount a doctor or supplier that accepts assignment can be paid. It may be less than the actual amount a doctor or supplier charges. Medicare pays part of this amount and you’re responsible for the difference.
What is Medicare Part A?
Medicare Part A (Hospital Insurance) Part A covers inpatient hospital stays, care in a skilled nursing facility, hospice care, and some home health care. coverage. Transplant drugs can be very costly. If you’re worried about paying for them after your Medicare coverage ends, talk to your doctor, nurse, or social worker.
How long does Medicare cover after kidney transplant?
If you're entitled to Medicare only because of ESRD, your Medicare coverage ends 36 months after the month of the kidney transplant. Part A covers inpatient hospital stays, care in a skilled nursing facility, hospice care, and some home health care. coverage. Transplant drugs can be very costly.
What is a prodrug?
A prodrug is an oral form of a drug that, when ingested, breaks down into the same active ingredient found in the injectable drug. As new oral cancer drugs become available, Part B may cover them. If Part B doesn’t cover them, Part D does.
What happens if you get a drug that Part B doesn't cover?
If you get drugs that Part B doesn’t cover in a hospital outpatient setting, you pay 100% for the drugs, unless you have Medicare drug coverage (Part D) or other drug coverage. In that case, what you pay depends on whether your drug plan covers the drug, and whether the hospital is in your plan’s network. Contact your plan to find out ...
What is Part B covered by Medicare?
Here are some examples of drugs Part B covers: Drugs used with an item of durable medical equipment (DME) : Medicare covers drugs infused through DME, like an infusion pump or a nebulizer, if the drug used with the pump is reasonable and necessary.
Does Medicare cover transplant drugs?
Medicare covers transplant drug therapy if Medicare helped pay for your organ transplant. Part D covers transplant drugs that Part B doesn't cover. If you have ESRD and Original Medicare, you may join a Medicare drug plan.
