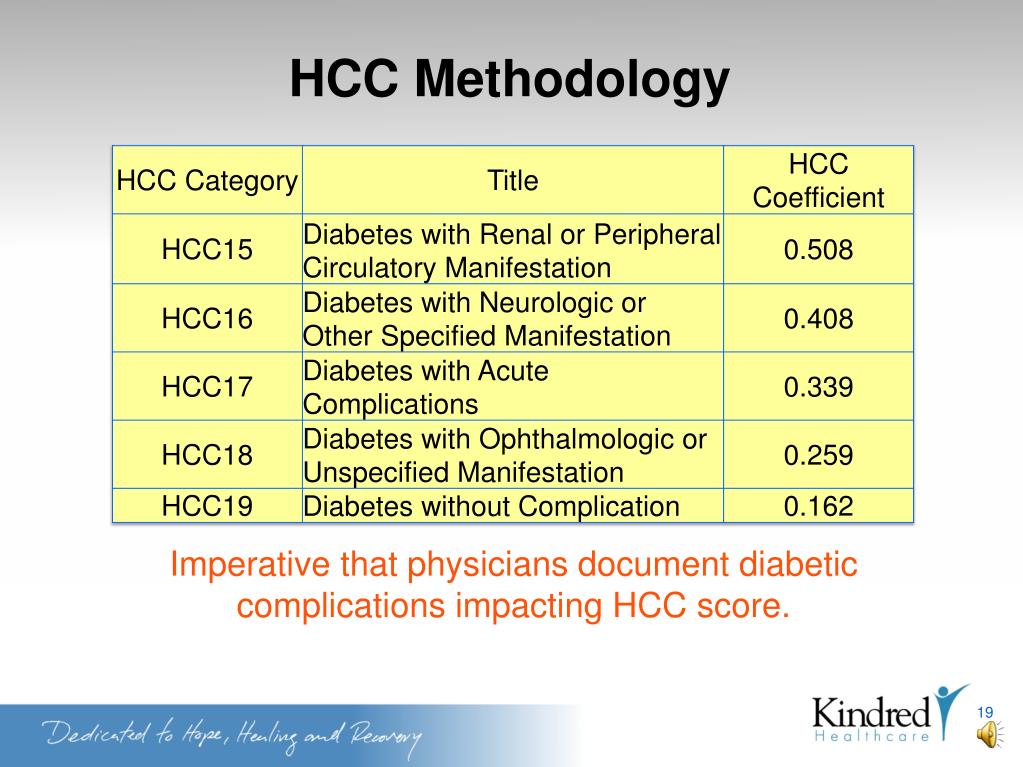
Physician reimbursement from Medicare is a three-step process: 1) appropriate coding of the service provided by utilizing current procedural terminology (CPT ®); 2) appropriate coding of the diagnosis using ICD-9 code; and 3) the Centers for Medicare and Medicaid Services (CMS
Centers for Medicare and Medicaid Services
The Centers for Medicare & Medicaid Services, previously known as the Health Care Financing Administration, is a federal agency within the United States Department of Health and Human Services that administers the Medicare program and works in partnership with state government…
Are you eligible for a Medicare reimbursement?
Only the member or a Qualified Surviving Spouse/Domestic Partner enrolled in Parts A and B is eligible for Medicare Part B premium reimbursement. 4. I received a letter stating that I pay a higher Part B premium based on my income level (Income-Related Monthly Adjustment Amount, i.e., IRMAA).
How are Medicare claims get paid?
- Providers can enter data via the Interactive Voice Response (IVR) telephone systems operated by the MACs.
- Providers can submit claim status inquiries via the Medicare Administrative Contractors’ provider Internet-based portals.
- Some providers can enter claim status queries via direct data entry screens.
Will Medicare reimburse me?
While people on Medicare are not able to seek reimbursement for at-home tests, you can instead order one for free through the federal government. The government will send out 500 million at-home test kits. You can order one through the forthcoming government website.
How does Medicare Advantage reimbursement work?
- You can get covered services for any health problems that aren’t part of your terminal illness and related conditions.
- You can choose to get services not related to your terminal illness from either your plan or Original Medicare.
- What you pay will depend on the plan and whether you follow the plan’s rules like seeing in-network providers. ...

How do physicians bill Medicare?
Payment for Medicare-covered services is based on the Medicare Physicians' Fee Schedule, not the amount a provider chooses to bill for the service. Participating providers receive 100 percent of the Medicare Allowed Amount directly from Medicare.
Does Medicare pay doctors directly?
Physicians and other health professionals: Medicare reimburses physicians and other health professionals (e.g., nurse practitioners) based on a fee-schedule for over 7,000 services.
What percentage of the allowable fee does Medicare pay a doctor?
80 percentUnder current law, when a patient sees a physician who is a “participating provider” and accepts assignment, as most do, Medicare pays 80 percent of the fee schedule amount and the patient is responsible for the remaining 20 percent.
Does Medicare pay doctors less?
Fee reductions by specialty Summarizing, we do find corroborative evidence (admittedly based on physician self-reports) that both Medicare and Medicaid pay significantly less (e.g., 30-50 percent) than the physician's usual fee for office and inpatient visits as well as for surgical and diagnostic procedures.
Why do doctors charge more than Medicare pays?
Why is this? A: It sounds as though your doctor has stopped participating with Medicare. This means that, while she still accepts patients with Medicare coverage, she no longer is accepting “assignment,” that is, the Medicare-approved amount.
Can a doctor charge more than the Medicare approved amount?
A doctor who does not accept assignment can charge you up to a maximum of 15 percent more than Medicare pays for the service you receive. A doctor who has opted out of Medicare cannot bill Medicare for services you receive and is not bound by Medicare's limitations on charges.
Why do doctors not like Medicare Advantage plans?
If they don't say under budget, they end up losing money. Meaning, you may not receive the full extent of care. Thus, many doctors will likely tell you they do not like Medicare Advantage plans because private insurance companies make it difficult for them to get paid for their services.
What is Medicare reimbursement fee schedule?
A fee schedule is a complete listing of fees used by Medicare to pay doctors or other providers/suppliers. This comprehensive listing of fee maximums is used to reimburse a physician and/or other providers on a fee-for-service basis.
Do doctors treat Medicare patients differently?
Many doctors try to help out patients who can't afford to pay the full amount for an office visit or the copay for a pricey medication. Now along comes a study suggesting that physicians in one Texas community treat patients differently, depending on whether they are on Medicare or have private insurance.
What percentage of doctors do not accept Medicare?
Only 1 percent of non-pediatric physicians have formally opted-out of the Medicare program. As of September 2020, 9,541 non-pediatric physicians have opted out of Medicare, representing a very small share (1.0 percent) of the total number active physicians, similar to the share reported in 2013.
Do hospitals lose money on Medicare patients?
Those hospitals, which include some of the nation's marquee medical centers, will lose 1% of their Medicare payments over 12 months. The penalties, based on patients who stayed in the hospitals anytime between mid-2017 and 2019, before the pandemic, are not related to covid-19.
What is a Medicare participating provider?
Physicians who agree to fully accept the rates set by Medicare are referred to as participating providers. They accept Medicare’s reimbursements fo...
What is a non-participating Medicare provider?
Because the reimbursement rates are generally lower than physicians receive from private insurance carriers, some physicians opt to be non-particip...
What is a Medicare opt-out provider?
A small number of doctors (less than 1 percent of eligible physicians) opt out of Medicare entirely, meaning that they do not accept Medicare reimb...
Why do doctors accept Medicare?
The reason so many doctors accept Medicare patients, even with the lower reimbursement rate, is that they are able to expand their patient base and serve more people.
What happens when someone receives Medicare benefits?
When someone who receives Medicare benefits visits a physician’s office, they provide their Medicare information , and instead of making a payment, the bill gets sent to Medicare for reimbursement.
Can a patient receive treatment for things not covered by Medicare?
A patient may be able to receive treatment for things not covered in these guidelines by petitioning for a waiver. This process allows Medicare to individually review a recipient’s case to determine whether an oversight has occurred or whether special circumstances allow for an exception in coverage limits.
Do you have to pay Medicare bill after an appointment?
For some patients, this means paying the full amount of the bill when checking out after an appointment, but for others , it may mean providing private insurance information and making a co-insurance or co-payment amount for the services provided. For Medicare recipients, however, the system may work a little bit differently.
What is Medicare participating provider?
Physicians who agree to fully accept the rates set by Medicare are referred to as participating providers. They accept Medicare’s reimbursements for all Medicare-covered services, for all Medicare patients, and bill Medicare directly for covered services. Most eligible providers are in this category. A Kaiser Family Foundation analysis found that ...
What happens if you don't accept assignment for treatment?
If you receive treatment from a non-participating provider who doesn’t accept assignment for the treatment you receive, you may have to pay the bill up front and seek reimbursement from Medicare for the portion they’ll pay.
What is Medicare reimbursement?
A: Medicare reimbursement refers to the payments that hospitals and physicians receive in return for services rendered to Medicare beneficiaries. The reimbursement rates for these services are set by Medicare, and are typically less than the amount billed or the amount that a private insurance company would pay.
How many psychiatrists have opted out of Medicare?
Of the tiny fraction of doctors who have opted out of Medicare entirely, 42 percent are psychiatrists. And although the number of doctors opting out increased sharply from 2012 to 2016, it dropped in 2017, with 3,732 doctors opting out.
Can a physician accept Medicare reimbursement?
Because the reimbursement rates are generally lower than physicians receive from private insurance carriers, some physicians opt to be non-participating providers. This means that they haven’t signed a contract agreeing to accept Medicare reimbursement as payment-in-full for all services, but they can agree to accept Medicare reimbursement ...
Does Medicare pay for the entire bill?
If a Medicare beneficiary receives services from one of these doctors, the patient must pay the entire bill; Medicare will not reimburse the doctor or the patient for any portion of the bill, and the provider can set whatever fees they choose.
Can a doctor opt out of Medicare?
A small number of doctors (less than 1 percent of eligible physicians) opt out of Medicare entirely, meaning that they do not accept Medicare reimbursement as payment-in-full for any services, for any Medicare patients. If a Medicare beneficiary receives services from one of these doctors, the patient must pay the entire bill;
What is the calendar year 2021 PFS?
The calendar year (CY) 2021 PFS proposed rule is one of several proposed rules that reflect a broader Administration-wide strategy to create a healthcare system that results in better accessibility, quality, affordability, empowerment, and innovation.
What is the CY 2021 rule?
The calendar year (CY) 2021 PFS final rule is one of several rules that reflect a broader Administration-wide strategy to create a healthcare system that results in better accessibility, quality, affordability, empowerment, and innovation.
When is the 2021 Medicare PFS final rule?
The CY 2021 Medicare Physician Fee Schedule Final Rule was placed on display at the Federal Register on December 2, 2020. This final rule updates payment policies, payment rates, and other provisions for services furnished under the Medicare Physician Fee Schedule (PFS) on or after Jan. 1, 2021.
When will Medicare start charging for PFS 2022?
The CY 2022 Medicare Physician Fee Schedule Proposed Rule with comment period was placed on display at the Federal Register on July 13, 2021. This proposed rule updates payment policies, payment rates, and other provisions for services furnished under the Medicare Physician Fee Schedule (PFS) on or after January 1, 2022.
What is the 2020 PFS rule?
The calendar year (CY) 2020 PFS final rule is one of several rules that reflect a broader Administration-wide strategy to create a healthcare system that results in better accessibility, quality, affordability, empowerment, and innovation.
When is the CY 2020 PFS final rule?
This final rule updates payment policies, payment rates, and other provisions for services furnished under the Medicare Physician Fee Schedule (PFS) on or after Jan. 1, 2020.
When is the Medicare Physician Fee Schedule 2020?
This final rule updates payment policies, payment rates, and other provisions for services furnished under the Medicare Physician Fee Schedule (PFS) on or after Jan. 1, 2020.
Clinical labor rates
A scheduled update to clinical labor rates will be implemented over a four-year period, culminating with the new rates taking full effect in 2025, according to a provision in the final rule. That’s a change from the proposed rule, which indicated the full change would be in 2022.
Telehealth
A number of telehealth services will continue to be covered by Medicare through 2023 as CMS evaluates whether they should be covered permanently. The services were scheduled to lose eligibility for coverage at the conclusion of the public health emergency.
Evaluation and management visits
The new rule establishes a definition for split E/M visits as visits provided in the facility setting by a physician and nonphysician practitioner in the same group. The visit should be billed by the clinician who provides “the substantive portion of the visit.”
Vaccine administration
Payment in 2022 will be $30 for influenza, pneumococcal and hepatitis B vaccines and will remain $40 for the COVID-19 vaccine, with the latter rate in effect through the end of the year in which the public health emergency ends. Payment will be $75.50 if administration of the COVID-19 vaccine takes place in a beneficiary’s home.
How Does Medicare Reimbursement Work?
If you are on Medicare, you usually don’t have to submit a claim when you receive medical services from a doctor, hospital or other health care provider so long as they are participating providers.
How to Get Reimbursed from Medicare
While most doctors simply bill Medicare directly, some other health care providers may require you to file for reimbursement from Medicare.
Reimbursement for Original Medicare
You won’t likely see a bill for services covered by Original Medicare. Participating providers will simply bill Medicare directly.
Medicare Advantage
You will never have to file a Medicare reimbursement claim if you have a Medicare Advantage plan. Medicare pays the private companies that manage Medicare Advantage plans to handle your claims for you.
Part D Prescription Drug Plan Reimbursement
Medicare Part D Prescription Drug plans are administered by private insurance companies. Generally, these companies handle any reimbursement process so you don’t have to worry about filing one.
What is the SGR for Medicare?
Under current law, Medicare’s physician fee-schedule payments are subject to a formula, called the Sustainable Growth Rate (SGR) system, enacted in 1987 as a tool to control spending. For more than a decade this formula has called for cuts in physician payments, reaching as high as 24 percent.
Does Medicare use prospective payment systems?
Medicare uses prospective payment systems for most of its providers in traditional Medicare. In general, these systems require that Medicare pre-determine a base payment rate for a given unit of service (e.g., a hospital stay, an episode of care, a particular service).
Does Medicare have a fee for service?
Current payment systems in traditional Medicare have evolved over the last several decades, but have maintained a fee-for-service payment structure for most types of providers. In many cases, private insurers have modeled their payment systems on traditional Medicare, including those used for hospitals and physicians.
How many DRGs can be assigned to a patient?
Each DRG is based on a specific primary or secondary diagnosis, and these groups are assigned to a patient during their stay depending on the reason for their visit. Up to 25 procedures can impact the specific DRG that is assigned to a patient, and multiple DRGs can be assigned to a patient during a single stay.
What is Medicare reimbursement based on?
Reimbursement is based on the DRGs and procedures that were assigned and performed during the patient’s hospital stay. Each DRG is assigned a cost based on the average cost based on previous visits. This assigned cost provides a simple method for Medicare to reimburse hospitals as it is only a simple flat rate based on the services provided.
What is Medicare Part A?
What Medicare Benefits Cover Hospital Expenses? Medicare Part A is responsible for covering hospital expenses when a Medicare recipient is formally admitted. Part A may include coverage for inpatient surgeries, recovery from surgery, multi-day hospital stays due to illness or injury, or other inpatient procedures.
How much higher is Medicare approved?
The amount for each procedure or test that is not contracted with Medicare can be up to 15 percent higher than the Medicare approved amount. In addition, Medicare will only reimburse patients for 95 percent of the Medicare approved amount.
How much extra do you have to pay for Medicare?
This means that the patient may be required to pay up to 20 percent extra in addition to their standard deductible, copayments, coinsurance payments, and premium payments. While rare, some hospitals completely opt out of Medicare services.
Is Medicare reimbursement lower than private insurance?
This is mainly due to the fact that Medicare reimbursement amounts are often lower than those received from private insurance companies . For these providers, the patient may be required to pay for the full cost of the visit up front and can then seek personal reimbursement from Medicare afterwards.
Does Medicare cover permanent disability?
Medicare provides coverage for millions of Americans over the age of 65 or individuals under 65 who have certain permanent disabilities. Medicare recipients can receive care at a variety of facilities, and hospitals are commonly used for emergency care, inpatient procedures, and longer hospital stays. Medicare benefits often cover care ...