You will qualify for Medicare and Medicaid
Medicaid
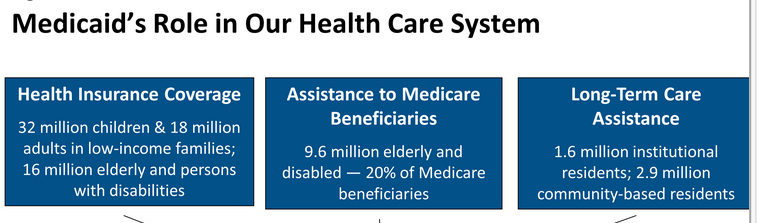
Medicaid in the United States is a federal and state program that helps with medical costs for some people with limited income and resources. Medicaid also offers benefits not normally covered by Medicare, including nursing home care and personal care services. The Health Insurance As…
Social Security Disability Insurance
Social Security Disability Insurance is a payroll tax-funded federal insurance program of the United States government. It is managed by the Social Security Administration and designed to provide income supplements to people who are physically restricted in their ability to be employed because of a notable disability. SSD can be supplied on either a temporary or permanent basis, usually directly correlated to …
Social Security Administration
The United States Social Security Administration is an independent agency of the U.S. federal government that administers Social Security, a social insurance program consisting of retirement, disability, and survivors' benefits. To qualify for most of these benefits, most workers pay Social …
How do I get Medicaid or Medicare?
Dec 29, 2021 · Some Medicare recipients also have Medicaid, a joint federal and state program. Medicaid covers the cost of long-term care if you meet your state’s eligibility requirements. The Centers for Medicare & Medicaid Services (CMS) monitors the quality of long-term services and supports (LTSS) delivered by state Medicaid authorities.
How does Medicare work with Medicaid and Medicare?
Feb 11, 2022 · If Medicare does not cover the full cost, Medicaid (the secondary payer) will cover the remaining cost, given they are Medicaid covered expenses. Medicaid also covers some expenses that Medicare does not, such as personal care assistance in the home and community and long-term skilled nursing home care.
What does Medicaid pay for?
If you have Medicare and full Medicaid coverage, most of your health care costs are likely covered. You can get your Medicare coverage through Original Medicare or a Medicare Advantage Plan (Part C). If you have Medicare and full Medicaid, you'll get your Part D prescription drugs through Medicare. And, you'll automatically qualify for Extra Help paying for your …
How can I see if I qualify for Medicaid?
Medicaid provides health coverage to 7.2 million low-income seniors who are also enrolled in Medicare. Medicaid also provides coverage to 4.8 million people with disabilities who are enrolled in Medicare. In total, 12 million people are "dually eligible" and enrolled in both Medicaid and Medicare, composing more than 15% of all Medicaid enrollees.

What is the lowest income to qualify for Medicaid?
Federal Poverty Level thresholds to qualify for Medicaid The Federal Poverty Level is determined by the size of a family for the lower 48 states and the District of Columbia. For example, in 2022 it is $13,590 for a single adult person, $27,750 for a family of four and $46,630 for a family of eight.Mar 26, 2022
When the patient is covered by both Medicare and Medicaid what would be the order of reimbursement?
Medicare pays first, and Medicaid pays second . If the employer has 20 or more employees, then the group health plan pays first, and Medicare pays second .
Can I have both Medicare and Medicaid?
Some Americans qualify for both Medicare and Medicaid, and when this happens, it usually means they don't have any out-of-pocket healthcare costs. Beneficiaries with Medicare and Medicaid are known as dual eligibles – and account for about 20 percent of Medicare beneficiaries (about 12.3 million people).
Will Medicaid pay for my Medicare Part B premium?
Medicaid can provide premium assistance: In many cases, if you have Medicare and Medicaid, you will automatically be enrolled in a Medicare Savings Program (MSP). MSPs pay your Medicare Part B premium, and may offer additional assistance.
How are my health care costs reimbursed if I have Medicare and Medicaid?
When dual eligible beneficiaries have healthcare expenses, Medicare pays first and Medicaid pays last. But this is not the case for things Medicare...
How do I know if I should be dual eligible?
Beneficiaries can find out if they’re eligible for Medicaid by contacting their Medicaid office. An Internet search for Medicaid offices in a benef...
What is the income range for beneficiaries who are dual eligibles?
Generally, beneficiaries earning less than 135 percent of the federal poverty level are eligible for the MSP if they also have limited savings (alt...
Can I select an insurance plan for my Medicare and Medicaid benefits?
If you are dual eligible, you are can enroll in a dual eligible special needs plan (D-SNP) that covers both Medicare and Medicaid benefits. These p...
What is extra help?
And, you'll automatically qualify for. Extra Help. A Medicare program to help people with limited income and resources pay Medicare prescription drug program costs, like premiums, deductibles, and coinsurance. paying for your.
Which pays first, Medicare or Medicaid?
Medicare pays first, and. Medicaid. A joint federal and state program that helps with medical costs for some people with limited income and resources. Medicaid programs vary from state to state, but most health care costs are covered if you qualify for both Medicare and Medicaid. pays second.
What is original Medicare?
Original Medicare. Original Medicare is a fee-for-service health plan that has two parts: Part A (Hospital Insurance) and Part B (Medical Insurance). After you pay a deductible, Medicare pays its share of the Medicare-approved amount, and you pay your share (coinsurance and deductibles). or a.
Does Medicare cover prescription drugs?
. Medicaid may still cover some drugs and other care that Medicare doesn’t cover.
Does Medicare have demonstration plans?
Medicare is working with some states and health plans to offer demonstration plans for certain people who have both Medicare and Medicaid and make it easier for them to get the services they need. They’re called Medicare-Medicaid Plans. These plans include drug coverage and are only in certain states.
Does Medicare Advantage cover hospice?
Medicare Advantage Plans provide all of your Part A and Part B benefits, excluding hospice. Medicare Advantage Plans include: Most Medicare Advantage Plans offer prescription drug coverage. . If you have Medicare and full Medicaid, you'll get your Part D prescription drugs through Medicare.
Can you get medicaid if you have too much income?
Even if you have too much income to qualify, some states let you "spend down" to become eligible for Medicaid. The "spend down" process lets you subtract your medical expenses from your income to become eligible for Medicaid. In this case, you're eligible for Medicaid because you're considered "medically needy."
How many people are covered by medicaid?
Medicaid also provides coverage to 4.8 million people with disabilities who are enrolled in Medicare.
Can Medicare help with out of pocket medical expenses?
Medicare enrollees who have limited income and resources may get help paying for their premiums and out-of-pocket medical expenses from Medicaid (e.g. MSPs, QMBs, SLBs, and QIs).
Can you be covered by Medicare and Medicaid?
Individuals who are enrolled in both Medicaid and Medicare, by federal statute, can be covered for both optional and mandatory categories.
What is a dual eligible special needs plan?
If you are dual eligible, you are can enroll in a dual eligible special needs plan (D-SNP) that covers both Medicare and Medicaid benefits. These plans may also pay for expenses that Medicare and Medicaid don’t over individually, including over-the-counter items, hearing aids, and vision or dental care. Beneficiaries who are dual eligible can ...
What is dual eligible Medicare?
Beneficiaries with Medicare and Medicaid are known as dual eligibles – and account for about 20 percent of Medicare beneficiaries (12.1 million people). Dual eligibles are categorized based on whether they receive partial or full Medicaid benefits. Full-benefit dual eligibles have comprehensive Medicaid coverage, ...
Is Medicare the same as Medicaid?
The federal government oversees Medicare eligi bility – meaning it is the same in each state. But states set their own eligibility rules for Medicaid and the MSPs (within federal guidelines) – and income limits for these programs vary widely.
Do seniors qualify for medicaid?
Many seniors who live in nursing homes are dual eligible: they qualify for Medicare based on their age, and Medicaid because of their financial circumstances.
Does Medicare cover long term care?
But this is not the case for things Medicare doesn’t cover, like long-term care . If Medicaid is covering a beneficiary’s long-term care, Medicare will still be the primary payer for any Medicare-covered services – like skilled nursing care or physical therapy.
Who is Josh Schultz?
Josh Schultz has a strong background in Medicare and the Affordable Care Act. He coordinated a Medicare ombudsman contract at the Medicare Rights Center in New York City, and represented clients in extensive Medicare claims and appeals.
When will I receive medicaid if I receive SSDI?
If you receive SSI, you will receive Medicaid. Keep in mind that for SSDI recipients, Medicare eligibility and coverage will not begin until 24 months have passed since you were first eligible for benefits.
Can I get medicaid if I have SSDI?
You will qualify for Medicare and Medicaid while you receive disability insurance, with some particular limitations. For instance, if you receive SSDI benefits, you will be eligible for certain parts of Medicare. If you receive SSI, you will receive Medicaid.
How long does it take to receive Medicaid inheritance?
As mentioned previously, a Medicaid beneficiary generally has 10 calendar days to report the receipt of an inheritance. However, based on the state in which one resides, the timeframe could be shorter or it could be longer. Also, as mentioned above, California allows Medicaid recipients to gift inheritance, which is considered “income”, the month in which it is received without violating Medicaid’s look back period. For state specific rules, one should contact their state Medicaid agency or a Medicaid professional that can research the individual’s specific situation.
How long does Medicaid look back?
Medicaid’s look back rule considers a long term care Medicaid applicant’s asset transfers for 60-months immediately preceding application to ensure assets were not given away or sold under fair market value. It also considers a Medicaid beneficiary giving away an inheritance as a violation of this rule, resulting in a penalty period.
How to meet Medicaid's asset limit?
Ways in which one might spend down an inheritance to meet Medicaid’s asset limit include paying off debt, purchasing an irrevocable funeral trust to prepay for funeral / burial costs, buying new household furnishings or appliances, and / or making home modifications.
What happens if you don't spend your inheritance?
Depending on the amount of the remaining inheritance, this can cause one to be asset ineligible, which means the individual is not eligible for Medicaid until the “excess” assets ...
How long does it take to report an inheritance to Medicaid?
Generally, this change in circumstance must be reported within 10 calendar days. Although this doesn’t give you a very large window to report it, it is vital that you do so. If you do not and the inheritance would have ...
Where does Albert live?
Albert resides in a Medicaid-funded nursing home in Pennsylvania, where the income limit is $2,349 / month and the asset limit is $2,000. His monthly income is $1,500, and the receipt of a $10,000 inheritance on June 15th pushes him well above Medicaid’s income limit. This causes him to be ineligible for Medicaid in June, ...
Can you accept an inheritance from Medicaid?
While you do not have to accept an inheritance and can instead “disclaim” (refuse) it, is not recommended that Medicaid beneficiaries do so. This is because when it comes to Medicaid, disclaiming an inheritance is not allowed under federal law. This is because Medicaid considers the inheritance a means for one to pay for his / her long term care.