
A person may qualify for both Medicare and Medicaid
Medicaid
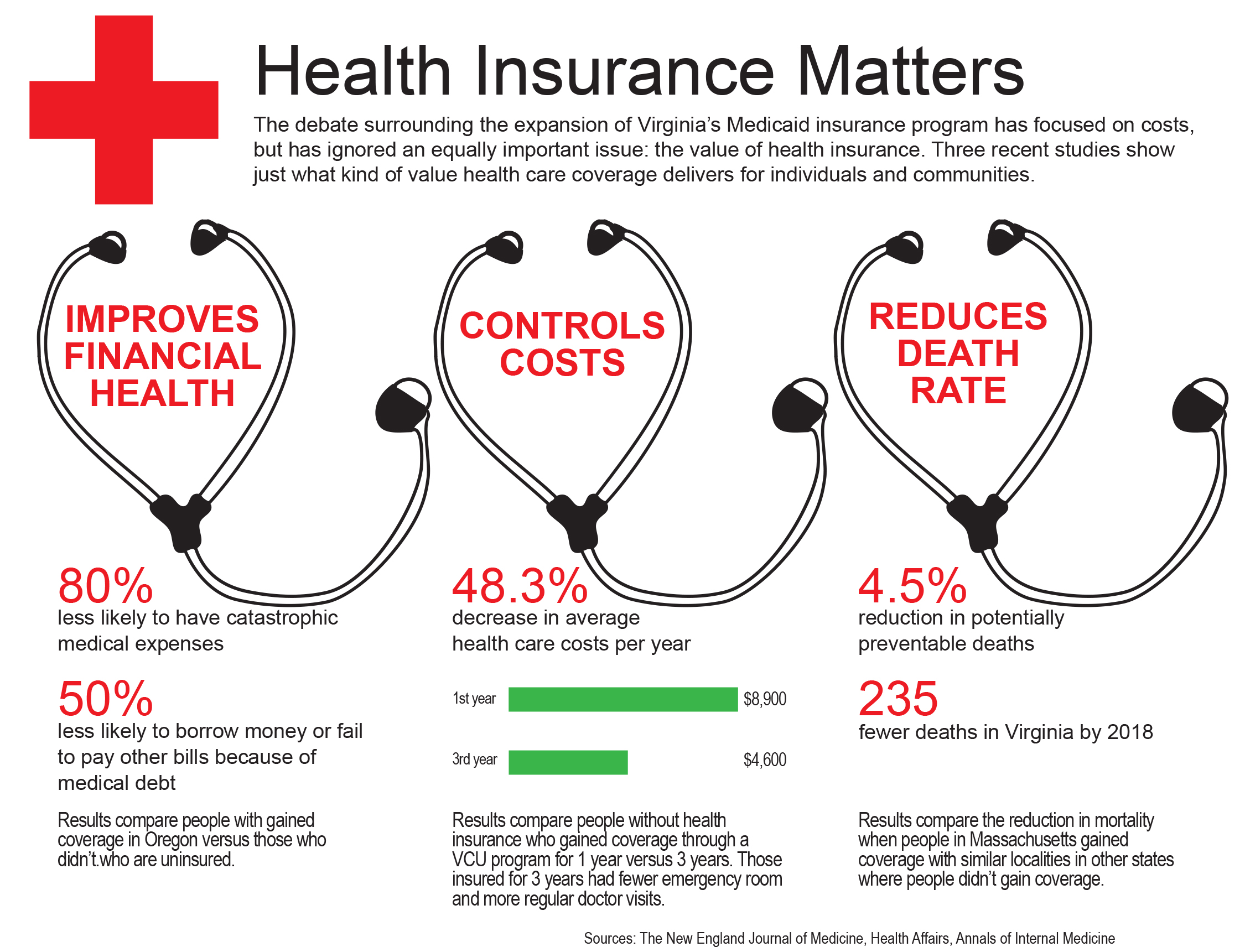
Medicaid in the United States is a federal and state program that helps with medical costs for some people with limited income and resources. Medicaid also offers benefits not normally covered by Medicare, including nursing home care and personal care services. The Health Insurance As…
How do I get Medicaid or Medicare?
Call your state Medicaid program to see if you qualify and learn how to apply. If you have Medicare and full Medicaid coverage, most of your health care costs are likely covered. You can get your Medicare coverage through Original Medicare or a Medicare Advantage Plan (Part C).
Can you have Medicare and Medicaid?
You might even be able to have a Medicare Advantage plan with Medicaid. Read more about Medicaid vs Medicare Advantage. Are you wondering if you can have Medicare and Medicaid? You might even be able to have a Medicare Advantage plan with Medicaid.
How many people are eligible for Medicare and Medicaid?
Medicaid also provides coverage to 4.8 million people with disabilities who are enrolled in Medicare. In total, 12 million people are "dually eligible" and enrolled in both Medicaid and Medicare, composing more than 15% of all Medicaid enrollees.
How does Medicare work with Medicaid and Medicare?
If you have Medicare and full Medicaid coverage, most of your health care costs are likely covered. You can get your Medicare coverage through Original Medicare or a Medicare Advantage Plan (Part C). If you have Medicare and full Medicaid, you'll get your Part D prescription drugs through Medicare.
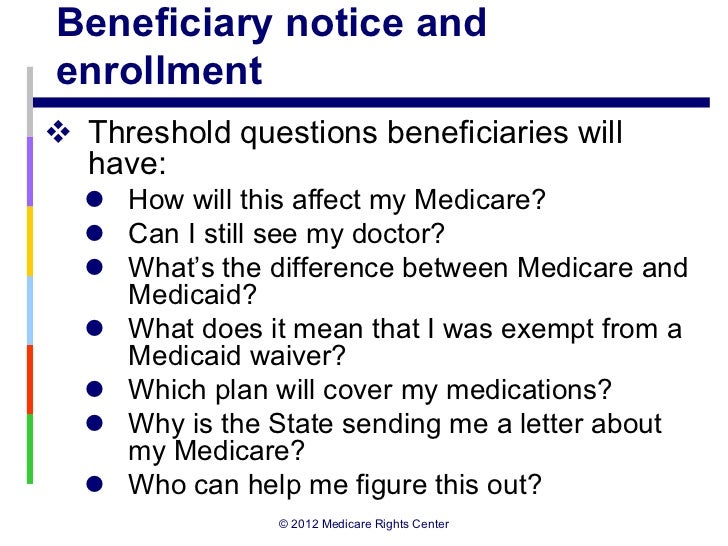
What do you call an individual who receives both Medicare and Medicaid?
Beneficiaries with Medicare and Medicaid are known as dual eligibles – and account for about 20 percent of Medicare beneficiaries (about 12.3 million people). Dual eligibles are categorized based on whether they receive partial or full Medicaid benefits.
What is the highest income to qualify for Medicaid?
Federal Poverty Level thresholds to qualify for Medicaid The Federal Poverty Level is determined by the size of a family for the lower 48 states and the District of Columbia. For example, in 2022 it is $13,590 for a single adult person, $27,750 for a family of four and $46,630 for a family of eight.
What does it mean if a Medicare patient is dual eligible?
Dually eligible beneficiaries are people enrolled in both Medicare and Medicaid who are eligible by virtue of their age or disability and low incomes.
When a patient is covered through Medicare and Medicaid which coverage is primary?
gov . Medicare pays first, and Medicaid pays second . If the employer has 20 or more employees, then the group health plan pays first, and Medicare pays second .
Can you have Medicare and Medicaid at the same time?
Yes. A person can be eligible for both Medicaid and Medicare and receive benefits from both programs at the same time.
How can I be eligible for Medicaid?
Medicaid beneficiaries generally must be residents of the state in which they are receiving Medicaid. They must be either citizens of the United States or certain qualified non-citizens, such as lawful permanent residents. In addition, some eligibility groups are limited by age, or by pregnancy or parenting status.
Can I get Medicare Part B for free?
While Medicare Part A – which covers hospital care – is free for most enrollees, Part B – which covers doctor visits, diagnostics, and preventive care – charges participants a premium. Those premiums are a burden for many seniors, but here's how you can pay less for them.
What is a partial dual eligible?
“Partial dual eligible” is a term used to describe Medicare beneficiaries who receive financial assistance for certain Medicare costs from their state Medicaid program. These individuals don't qualify for full Medicaid benefits from their state, like long-term services and supports or behavioral health services.
Is Medicare provided without cost to the Medicare beneficiary?
Medicare is provided without cost to the Medicare beneficiary. The Affordable Care Act is reducing enrollee cost sharing during the drug coverage gap. CMS requires MA plans to have a quality improvement program to measure program performance.
What is the point of secondary insurance?
A secondary insurance policy is a plan that you get on top of your main health insurance. Secondary insurance can help you improve your coverage by giving you access to additional medical providers, such as out-of-network doctors. It can also provide benefits for uncovered health services, such as vision or dental.
What are the disadvantages of Medicaid?
Disadvantages of Medicaid They will have a decreased financial ability to opt for elective treatments, and they may not be able to pay for top brand drugs or other medical aids. Another financial concern is that medical practices cannot charge a fee when Medicaid patients miss appointments.
Can you use 2 insurance plans?
While it sounds confusing, having dual insurance like this is perfectly legal—you just need to make sure you're coordinating your two benefits correctly to make sure your medical expenses are being covered compliantly.
How are my health care costs reimbursed if I have Medicare and Medicaid?
When dual eligible beneficiaries have healthcare expenses, Medicare pays first and Medicaid pays last. But this is not the case for things Medicare...
How do I know if I should be dual eligible?
Beneficiaries can find out if they’re eligible for Medicaid by contacting their Medicaid office. An Internet search for Medicaid offices in a benef...
What is the income range for beneficiaries who are dual eligibles?
Generally, beneficiaries earning less than 135 percent of the federal poverty level are eligible for the MSP if they also have limited savings (alt...
Can I select an insurance plan for my Medicare and Medicaid benefits?
If you are dual eligible, you are can enroll in a dual eligible special needs plan (D-SNP) that covers both Medicare and Medicaid benefits. These p...
What is Medicare and Medicaid?
Differentiating Medicare and Medicaid. Persons who are eligible for both Medicare and Medicaid are called “dual eligibles”, or sometimes, Medicare-Medicaid enrollees. Since it can be easy to confuse the two terms, Medicare and Medicaid, it is important to differentiate between them. While Medicare is a federal health insurance program ...
How old do you have to be to apply for medicare?
Citizens or legal residents residing in the U.S. for a minimum of 5 years immediately preceding application for Medicare. Applicants must also be at least 65 years old.
What is the CMS?
The Centers for Medicare and Medicaid Services, abbreviated as CMS, oversees both the Medicare and Medicaid programs. For the Medicaid program, CMS works with state agencies to administer the program in each state, and for the Medicare program, the Social Security Administration (SSA) is the agency through which persons apply.
How much does Medicare Part B cost?
For Medicare Part B (medical insurance), enrollees pay a monthly premium of $148.50 in addition to an annual deductible of $203. In order to enroll in a Medicare Advantage (MA) plan, one must be enrolled in Medicare Parts A and B. The monthly premium varies by plan, but is approximately $33 / month.
What is the income limit for Medicaid in 2021?
In most cases, as of 2021, the individual income limit for institutional Medicaid (nursing home Medicaid) and Home and Community Based Services (HCBS) via a Medicaid Waiver is $2,382 / month. The asset limit is generally $2,000 for a single applicant.
Is Medicare the first payer?
For Medicare covered expenses, such as medical and hospitalization, Medicare is always the first payer (primary payer). If Medicare does not cover the full cost, Medicaid ...
Can you be disqualified from Medicaid if you have assets?
Please note that income and assets over the Medicaid limit (s) in one’s state is not cause for automatic disqualification. This is because there are Medicaid-compliant planning strategies intended to lower one’s countable income and / or assets in order to meet the limit (s). A word of caution: It is vital that assets not be given away a minimum of 5 years (2.5 years in California) prior to the date of one’s Medicaid application. (New York is in the process of implementing a 2.5 year look back for long-term home and community based services). This is because Medicaid has a look-back period in which past transfers are reviewed to ensure an applicant (and / or an applicant’s spouse) has not gifted assets or sold them under fair market value. If this rule has been violated, it is assumed the assets were transferred in order to meet Medicaid’s asset limit and a penalty period of Medicaid disqualification will be calculated.
How old do you have to be to qualify for Medicare?
Eligibility for Medicare. The usual way to qualify for Medicare is to be 65 years of age. A person can receive premium-free Part A (hospital coverage) benefits if they or their spouse is 65 or older and has paid sufficient Medicare taxes through previous employment.
Why is it important to have both Medicare and Medicaid?
Receiving both Medicare and Medicaid can help decrease healthcare costs for those who are often most in need of treatment.
How many people are dually eligible for medicaid?
If a person qualifies for both, the government refers to them as dually eligible. An estimated 12 million people in the United States are dually eligible for Medicare and Medicaid, according to Medicaid.gov. In this article, we discuss eligibility for Medicare and Medicaid, as well as what to know about each program.
What is Medicare Part B?
They can also qualify for Medicare Part B, which is medical coverage for doctor visits and many other medical-related expenses.
What is the age limit for Medicare?
Medicare. Medicare is an insurance plan for people at or over the age of 65 and for others with qualifying medical concerns. A person must meet eligibility criteria based on their work history or that of their spouse. They can qualify for premium-free hospital coverage and pay a premium for medical and prescription drug coverage.
How often does medicaid change?
Medicaid standards can change every year. If a person was unsuccessful in a prior application, they might qualify at a later date. One of the most important factors for Medicaid eligibility is where a person falls on the Federal Poverty Level (FPL).
What is Medicaid insurance?
Medicaid is a health insurance program providing financial assistance to individuals and families with a low income or limited financial resources. The federal government sets rules and regulations regarding Medicaid, and individual states are responsible for operating Medicaid programs.
What is the difference between Medicare and Medicaid?
Simply put, both Medicare and Medicaid are government-regulated health insurance programs that help to provide healthcare service and treatment to millions of Americans, but each program has slightly different rules of eligibility and provides different coverage to different groups of people.
What is Medicare for seniors?
Medicare is a health insurance program that is designed to help seniors and certain qualifying disabled individuals pay for their health care costs.
What is dual eligible Medicare?
Individuals who qualify for both Medicare and Medicaid are known as “dual eligible” and are likely to have most of their healthcare needs covered in some form.
What percentage of Medicare beneficiaries are dual eligible?
Dual eligible individuals account for about 20 percent of Medicare beneficiaries, and are classified into two separate categories.
What is a Pacde plan?
PACE plans provide medical and social services to a myriad of elderly individuals, most of whom are dual eligible. PACDE operates as a sort of “home-health” model where a multi-faceted team of healthcare professionals work together to provide coordinated care to an individual from the comfort of their very own home or community.
How much money do I need to qualify for SSI in 2021?
To qualify for SSI, you must be under a specified income limit (As of 2021: $794 per month for an individual or child, and $1,191 for a couple) and your assets must be considered limited (As of 2021: $2,000 for an individual or child, $3,000 for a couple).
Can dual eligible individuals receive Medicare?
Dual eligible individuals may wish to receive healthcare coverage through Original Medicare Parts A and B. If so decided, the beneficiary would receive Part A and Part B coverage directly with Medicaid serving as a “wrap around” coverage that pays for services that Original Medicare does not cover.
What is not covered by Medicare?
Offers benefits not normally covered by Medicare, like nursing home care and personal care services
What is original Medicare?
Original Medicare. Original Medicare is a fee-for-service health plan that has two parts: Part A (Hospital Insurance) and Part B (Medical Insurance). After you pay a deductible, Medicare pays its share of the Medicare-approved amount, and you pay your share (coinsurance and deductibles). or a.
Which pays first, Medicare or Medicaid?
Medicare pays first, and. Medicaid. A joint federal and state program that helps with medical costs for some people with limited income and resources. Medicaid programs vary from state to state, but most health care costs are covered if you qualify for both Medicare and Medicaid. pays second.
Does Medicare have demonstration plans?
Medicare is working with some states and health plans to offer demonstration plans for certain people who have both Medicare and Medicaid and make it easier for them to get the services they need. They’re called Medicare-Medicaid Plans. These plans include drug coverage and are only in certain states.
Does Medicare cover health care?
If you have Medicare and full Medicaid coverage, most of your health care costs are likely covered.
Does Medicare Advantage cover hospice?
Medicare Advantage Plans provide all of your Part A and Part B benefits, excluding hospice. Medicare Advantage Plans include: Most Medicare Advantage Plans offer prescription drug coverage. . If you have Medicare and full Medicaid, you'll get your Part D prescription drugs through Medicare.
Can you get medicaid if you have too much income?
Even if you have too much income to qualify, some states let you "spend down" to become eligible for Medicaid. The "spend down" process lets you subtract your medical expenses from your income to become eligible for Medicaid. In this case, you're eligible for Medicaid because you're considered "medically needy."
How many people are covered by medicaid?
Medicaid also provides coverage to 4.8 million people with disabilities who are enrolled in Medicare.
What is Part B in Medicare?
Part B: Pays for physician services, lab and x-ray services, durable medical equipment, and outpatient and other services
Can you be covered by Medicare and Medicaid?
Individuals who are enrolled in both Medicaid and Medicare, by federal statute, can be covered for both optional and mandatory categories.
Can Medicare help with out of pocket medical expenses?
Medicare enrollees who have limited income and resources may get help paying for their premiums and out-of-pocket medical expenses from Medicaid (e.g. MSPs, QMBs, SLBs, and QIs).
How many people are covered by medicaid?
Medicaid is a joint federal and state program that, together with the Children’s Health Insurance Program (CHIP), provides health coverage to over 72.5 million Americans, including children, pregnant women, parents, seniors, and individuals with disabilities. Medicaid is the single largest source of health coverage in the United States.
What is dual eligible for Medicare?
Eligibility for the Medicare Savings Programs, through which Medicaid pays Medicare premiums, deductibles, and/or coinsurance costs for beneficiaries eligible for both programs (often referred to as dual eligibles) is determined using SSI methodologies..
What is MAGI for Medicaid?
MAGI is the basis for determining Medicaid income eligibility for most children, pregnant women, parents, and adults. The MAGI-based methodology considers taxable income and tax filing relationships to determine financial eligibility for Medicaid. MAGI replaced the former process for calculating Medicaid eligibility, ...
What is the Medicaid age limit?
The Affordable Care Act of 2010 created the opportunity for states to expand Medicaid to cover nearly all low-income Americans under age 65 . Eligibility for children was extended to at least 133% of the federal poverty level (FPL) in every state (most states cover children to higher income levels), and states were given the option to extend eligibility to adults with income at or below 133% of the FPL. Most states have chosen to expand coverage to adults, and those that have not yet expanded may choose to do so at any time. See if your state has expanded Medicaid coverage to low-income adults.
What is Medicaid coverage?
Medicaid is the single largest source of health coverage in the United States. To participate in Medicaid, federal law requires states to cover certain groups of individuals. Low-income families, qualified pregnant women and children, and individuals receiving Supplemental Security Income (SSI) are examples of mandatory eligibility groups (PDF, ...
How long does medicaid last?
Benefits also may be covered retroactively for up to three months prior to the month of application, if the individual would have been eligible during that period had he or she applied. Coverage generally stops at the end of the month in which a person no longer meets the requirements for eligibility.
Does Medicaid require income?
Certain Medicaid eligibility groups do not require a determination of income by the Medicaid agency. This coverage may be based on enrollment in another program, such as SSI or the breast and cervical cancer treatment and prevention program.
How does Medicare work with other insurance?
When there's more than one payer, "coordination of benefits" rules decide which one pays first. The "primary payer" pays what it owes on your bills first, and then sends the rest to the "secondary payer" (supplemental payer) ...
What is the phone number for Medicare?
It may include the rules about who pays first. You can also call the Benefits Coordination & Recovery Center (BCRC) at 1-855-798-2627 (TTY: 1-855-797-2627).
What is a Medicare company?
The company that acts on behalf of Medicare to collect and manage information on other types of insurance or coverage that a person with Medicare may have, and determine whether the coverage pays before or after Medicare. This company also acts on behalf of Medicare to obtain repayment when Medicare makes a conditional payment, and the other payer is determined to be primary.
How long does it take for Medicare to pay a claim?
If the insurance company doesn't pay the claim promptly (usually within 120 days), your doctor or other provider may bill Medicare. Medicare may make a conditional payment to pay the bill, and then later recover any payments the primary payer should have made. If Medicare makes a. conditional payment.
What is a group health plan?
If the. group health plan. In general, a health plan offered by an employer or employee organization that provides health coverage to employees and their families.
How many employees does a spouse have to have to be on Medicare?
Your spouse’s employer must have 20 or more employees, unless the employer has less than 20 employees, but is part of a multi-employer plan or multiple employer plan. If the group health plan didn’t pay all of your bill, the doctor or health care provider should send the bill to Medicare for secondary payment.
Which pays first, Medicare or group health insurance?
If you have group health plan coverage through an employer who has 20 or more employees, the group health plan pays first, and Medicare pays second.
What Is The Difference Between Medicare and Medicaid?
Is It Possible to Be Eligible For Both Medicare and Medicaid?
- It may come as a surprise to many, but the answer to this question is yes: it is indeed possible to qualify for both Medicare and Medicaid simultaneously. This status is known as dual eligibility, and may give you access to more comprehensive benefits than you otherwise would have. If you are a dual eligible individual, you are likely to have most ...
Full-Benefit Dual Eligibility
- Full-benefit dual eligibles are individuals who have access to comprehensive Medicaid coverage and are also enrolled in Medicare coverage. Remember that Medicaid eligibility requirements vary by state, so it is important to refer to your state’s guidelines before exploring your possible benefits under dual eligibility. Generally, however, people who qualify for full dual eligible covera…
Partial-Benefit Dual Eligibility
- Typically, those who are considered partial-benefit dual eligibles do not receive full Medicaid coverage and usually fall into one of the following Medicare Savings Program (MSP)categories: