While it is always advisable to have Part A, you can buy Medicare Part B (medical insurance) without having to buy Medicare Part A (hospital insurance) as long as you are: Age 65+ And, a U.S. citizen or a legal resident who has lived in the U.S. for at least five years
Do you really need Medicare Part B?
Medicare Part B isn’t a legal requirement, and you don’t need it in some situations. In general, if you’re eligible for Medicare and have creditable coverage, you can postpone Part B penalty-free. Creditable coverage includes the insurance provided to you or your spouse through work.
How do I add Part B to my Medicare?
When you have an Advantage plan, Medicare Parts A and Part B do not act as secondary coverage for your Advantage plan. You don’t get healthcare services from both, because when you choose a Medicare Advantage plan you are deselecting CMS as the ...
What is the maximum premium for Medicare Part B?
The standard monthly premium for Part B, which covers outpatient care and durable equipment ... or offers a different copay and an out-of-pocket maximum (a Medicare Advantage Plan). The Aduhelm situation highlights the ripple effect that expensive drugs ...
Does Medicaid replace Medicare Part B?
More than 8 million people have both Medicare and Medicaid. In this situation, Medicare becomes your primary insurance and settles your medical bills first; and Medicaid become secondary, paying for services that Medicare doesn’t cover and also paying most of your out-of-pocket expenses in Medicare (premiums, deductibles and copays).

What is Medicare Part B only?
Medicare Part B (Medical Insurance) Part B helps cover medically necessary services like doctors' services, outpatient care, and other medical services that Part A doesn't cover. Part B also covers many preventive services. Part B coverage is your choice.
How does one enroll in Medicare Part B?
Most people get Medicare Part B (Medical Insurance) when they turn 65....There are 3 ways you can sign up:Fill out a short form, and send it to your local Social Security office.Call Social Security at 1-800-772-1213. TTY users can call 1-800-325-0778.Contact your local Social Security office.
Are Medicare Part B premiums standard for everyone?
Most people pay the standard Part B premium amount. If your modified adjusted gross income as reported on your IRS tax return from 2 years ago is above a certain amount, you'll pay the standard premium amount and an Income Related Monthly Adjustment Amount (IRMAA).
How do I know if I am entitled to Medicare Part B?
You're 65 years old You automatically qualify for Medicare Part B once you turn 65 years old. Although you'll need to wait to use your benefits until your 65th birthday, you can enroll: 3 months before your 65th birthday.
Can I add Medicare Part B at any time?
You can sign up for Medicare Part B at any time that you have coverage through current or active employment. Or you can sign up for Medicare during the eight-month Special Enrollment Period that starts when your employer or union group coverage ends or you stop working (whichever happens first).
How long does it take for Medicare Part B to be approved?
You can also call the Social Security Administration at 1-800-772-1213 or go to your local Social Security office. It takes about 45 to 90 days to receive your acceptance letter after submitting your Medicare application.
Is Medicare Part B automatically deducted from Social Security?
Yes. In fact, if you are signed up for both Social Security and Medicare Part B — the portion of Medicare that provides standard health insurance — the Social Security Administration will automatically deduct the premium from your monthly benefit.
What is the Medicare Part B premium for 2021?
$148.50Medicare Part B Premium and Deductible The standard monthly premium for Medicare Part B enrollees will be $170.10 for 2022, an increase of $21.60 from $148.50 in 2021. The annual deductible for all Medicare Part B beneficiaries is $233 in 2022, an increase of $30 from the annual deductible of $203 in 2021.
Can I get Medicare Part B for free?
While Medicare Part A – which covers hospital care – is free for most enrollees, Part B – which covers doctor visits, diagnostics, and preventive care – charges participants a premium. Those premiums are a burden for many seniors, but here's how you can pay less for them.
Who is eligible for Medicare Part B reimbursement?
1. How do I know if I am eligible for Part B reimbursement? You must be a retired member or qualified survivor who is receiving a pension and is eligible for a health subsidy, and enrolled in both Medicare Parts A and B.
Do you have to enroll in Medicare Part B every year?
Do You Need to Renew Medicare Part B every year? As long as you pay the Medicare Part B medical insurance premiums, you'll continue to have the coverage. The premium is subtracted monthly from most people's Social Security payments. If you don't get Social Security, you'll get a bill.
Why is Medicare Part B required?
Medicare Part B helps cover medical services like doctors' services, outpatient care, and other medical services that Part A doesn't cover. Part B is optional. Part B helps pay for covered medical services and items when they are medically necessary.
Understanding What Medicare Part B Offers
First, let’s take a look at what Medicare Part B actually covers. Medicare Part B covers medical treatments and services under two classifications:...
Medicare Part B Enrollment Options and Penalties
Medicare Part B is optional, but in some ways, it can feel mandatory, because there are penalties associated with delayed enrollment. As discussed...
The Cost of Medicare Part B
Unlike Medicare Part A, Medicare Part B requires a premium. For the most part, the premium for Medicare Part B is $134 per month. You also pay $204...
Medicare Part B Financial Assistance
Because Medicare Part B requires a monthly payment (known as a premium) for its services, some people may find it difficult to pay for the monthly...
Medicare Part B Special Circumstances and Updates
Some people don’t need Medicare Part B coverage right away, because they have medical insurance through their employers or meet other special condi...
Benefits of Medicare Part B
Medicare Part B covers a variety of routine healthcare visits and treatments. If you can afford the premiums, then you may want to take advantage o...
How to qualify for Medicare premium free?
To be eligible for premium-free Part A, an individual must be entitled to receive Medicare based on their own earnings or those of a spouse, parent, or child. To receive premium-free Part A, the worker must have a specified number of quarters of coverage (QCs) and file an application for Social Security or Railroad Retirement Board (RRB) benefits. The exact number of QCs required is dependent on whether the person is filing for Part A on the basis of age, disability, or End Stage Renal Disease (ESRD). QCs are earned through payment of payroll taxes under the Federal Insurance Contributions Act (FICA) during the person's working years. Most individuals pay the full FICA tax so the QCs they earn can be used to meet the requirements for both monthly Social Security benefits and premium-free Part A.
When do you have to be on Medicare before you can get Medicare?
Individuals already receiving Social Security or RRB benefits at least 4 months before being eligible for Medicare and residing in the United States (except residents of Puerto Rico) are automatically enrolled in both premium-free Part A and Part B.
How long do you have to be on Medicare if you are disabled?
Disabled individuals are automatically enrolled in Medicare Part A and Part B after they have received disability benefits from Social Security for 24 months. NOTE: In most cases, if someone does not enroll in Part B or premium Part A when first eligible, they will have to pay a late enrollment penalty.
How long does it take to get Medicare if you are 65?
For someone under age 65 who becomes entitled to Medicare based on disability, entitlement begins with the 25 th month of disability benefit entitlement.
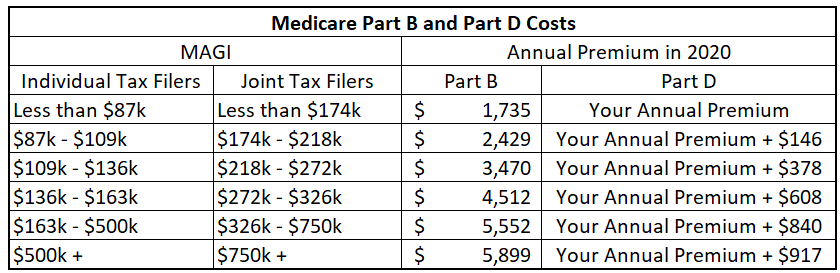
What is the income related monthly adjustment amount for Medicare?
Individuals with income greater than $85,000 and married couples with income greater than $170,000 must pay a higher premium for Part B and an extra amount for Part D coverage in addition to their Part D plan premium. This additional amount is called income-related monthly adjustment amount. Less than 5 percent of people with Medicare are affected, so most people will not pay a higher premium.
How long does Medicare take to pay for disability?
A person who is entitled to monthly Social Security or Railroad Retirement Board (RRB) benefits on the basis of disability is automatically entitled to Part A after receiving disability benefits for 24 months.
When do you have to apply for Medicare if you are already on Social Security?
Individuals already receiving Social Security or RRB benefits at least 4 months before being eligible for Medicare and residing in the United States (except residents of Puerto Rico) are automatically enrolled in both premium-free Part A and Part B. People living in Puerto Rico who are eligible for automatic enrollment are only enrolled in premium-free Part A.
How long do you have to be a resident to be eligible for Medicare?
And, a U.S. citizen or a legal resident who has lived in the U.S. for at least five years. Note, however, that if you do not enroll in Part A when you are first eligible for Medicare and you have to pay a premium for Part A, you can only enroll later if you have a Special Enrollment Period, or during the General Enrollment Period .
How to contact Medicare in New York?
If you live in New York and have questions about cost-saving programs, call the Medicare Rights Center’s free national helpline at 800-333-4114.
What is covered by Medicare Part B?
In addition, Part B may cover other medical procedures and treatments that fall within the necessary or preventive range. Ambulance services, clinical research, mental health counseling and some prescription drugs for outpatient treatment may all be covered under Medicare Part B.
Why don't people enroll in Medicare Part B?
And some people choose not to enroll in Medicare Part B, because they don’t want to pay for medical coverage they feel they don’t need. There are a variety of reasons why you might hesitate to pay for medical insurance. Likewise, you may be concerned about how the new healthcare laws affect Medicare Part B coverage.
How to reduce Medicare premiums?
One such way is to enroll in a Medicare Savings Program. Run by individual states in conjunction with Medicare, Medicare Savings Plans help you pay for medical costs associated with deductibles, coinsurance and copayments, in some cases. There are four Medicare Savings Programs available, but only three of them relate to Medicare Part B. They are:
What happens if you miss your Medicare enrollment window?
What happens if you miss your initial enrollment window? If you delay Medicare Part B enrollment, then you’ll have to wait to enroll when the general enrollment period starts. In this example, your birthday is March 8. Because you missed your initial window, you’ll have to wait until January of the following year to enroll and July of the following year to start receiving coverage.
How much does Medicare pay if you make less than $500,000?
Individuals who earn more than $163,000 but less than $500,000 per year will pay $462.70 in Medicare Part B premiums per month. If you earn $500,000 per year or more, your Medicare Part B premium will be $491.60 per month. These amounts reflect individual incomes only.
How long do you have to be in Medicare to get Medicare Part B?
You have a seven-month initial period to enroll in Medicare Part B. The seven months include the three months prior to your 65th birthday, the month containing your 65th birthday and the three months that follow your birthday month. If you turn 65 on March 8, then you have from December 1 to June 30 to enroll in Medicare Part B.
How much is Medicare Part B in 2021?
That premium changes each year, usually increasing. In 2021, the Part B premium is $148.50 a month. You’ll also have an annual deductible of $203 in 2021 (an increase from the $198 deductible in 2020).
What is the Part B premium reduction benefit?
The giveback benefit, or Part B premium reduction, is when a Part C Medicare Advantage (MA) plan reduces the amount you pay toward your Part B monthly premium. Your reimbursement amount could range from less than $1 to the full premium amount, which is $170.10 in 2022.
What happens if you don't pay Medicare Part B?
If you don't pay your monthly Medicare Part B premiums through Social Security, the giveback benefit would be credited to your monthly statement. Instead of paying the full $148.50, you'd only pay the amount with the giveback benefit deducted.
What is the Medicare premium for 2021?
In 2021, the standard Medicare Part B monthly premium is $148.50. Beneficiaries also have a $203 deductible, and once they meet the deductible, must typically pay 20% of the Medicare-approved amount for any medical services and supplies.
What does it mean to be dually eligible for Medicare?
If you're dually eligible, it means you have both Medicare and Medicaid.
How to find Part B buy down?
If you enroll in a plan that offers a giveback benefit, you'll find a section in the plan's summary of benefits or evidence of coverage (EOC) that outlines the Part B premium buy-down. Here, you'll see how much of a reduction you'll get. You can also call us toll-free at 1-855-537-2378 and one of our knowledgeable, licensed agents will answer your questions and explain your options.
Can you lower Medicare Part B premium?
There are other ways you can lower or eliminate how much you pay for the Medicare Part B premium. This includes certain Medicaid programs or benefits from some retiree health plans.
Can you enroll in Medicare Advantage if you have Medicaid?
This means anyone with Medicaid or other forms of assistance that pay the Part B premium cannot enroll in one of these Medicare Advantage plans.
What does BCRC do?
The BCRC will gather information about any conditional payments Medicare made related to your settlement, judgment, award or other payment. If you get a payment, you or your lawyer should call the BCRC. The BCRC will calculate the repayment amount (if any) on your recovery case and send you a letter requesting repayment.
What is a Medicare company?
The company that acts on behalf of Medicare to collect and manage information on other types of insurance or coverage that a person with Medicare may have, and determine whether the coverage pays before or after Medicare. This company also acts on behalf of Medicare to obtain repayment when Medicare makes a conditional payment, and the other payer is determined to be primary.
What is conditional payment?
A conditional payment is a payment Medicare makes for services another payer may be responsible for. Medicare makes this conditional payment so you won't have to use your own money to pay the bill. The payment is "conditional" because it must be repaid to Medicare if you get a settlement, judgment, award, or other payment later.
How long does it take for Medicare to pay a claim?
If the insurance company doesn't pay the claim promptly (usually within 120 days), your doctor or other provider may bill Medicare. Medicare may make a conditional payment to pay the bill, and then later recover any payments the primary payer should have made. If Medicare makes a. conditional payment.
What is a group health plan?
If the. group health plan. In general, a health plan offered by an employer or employee organization that provides health coverage to employees and their families.
How does Medicare work with other insurance?
When there's more than one payer, "coordination of benefits" rules decide which one pays first. The "primary payer" pays what it owes on your bills first, and then sends the rest to the "secondary payer" (supplemental payer) ...
What is the difference between primary and secondary insurance?
The insurance that pays first (primary payer) pays up to the limits of its coverage. The one that pays second (secondary payer) only pays if there are costs the primary insurer didn't cover. The secondary payer (which may be Medicare) may not pay all the uncovered costs.
Do I Need to Enroll in a QMB Program if I Have Medigap?
Medigap coverage isn’t necessary for anyone on the QMB program. This program helps you avoid the need for a Medigap plan by assisting in coverage for copays, premiums, and deductibles. Those that don’t qualify for the QMB program may find that a Medigap plan helps make their health care costs much more predictable.
What is a QMB premium?
The Part A monthly premium (if applicable) The Part B monthly premium and annual deductible. Coinsurance and deductibles for health care services through Parts A and B. If you’re in a QMB program, you’re also automatically eligible for the Extra Help program, which helps pay for prescription drugs.
What is a qualified Medicare beneficiary?
The Qualified Medicare Beneficiary program is a type of Medicare Savings Program (MSP). The QMB program allows beneficiaries to receive financial help from their state of residence with the costs of Medicare premiums and more. A Qualified Medicare Beneficiary gets government help to cover health care costs like deductibles, premiums, and copays.
What is QMB in Medicare?
Qualified Medicare Beneficiary (QMB) Program. If you’re a Medicare beneficiary, you know that health care costs can quickly add up. These costs are especially noticeable when you’re on a fixed income. If your monthly income and total assets are under the limit, you might be eligible for a Qualified Medicare Beneficiary program, or QMB.
What is Medicare qualified?
A Qualified Medicare Beneficiary gets government help to cover health care costs like deductibles, premiums, and copays. Recipients must meet all criteria to qualify for the program assistance.
What is the QMB in North Carolina?
In North Carolina QMB is called MQB. If you live in Nebraska, Federal QMB is replaced with full Medicaid.
Why do you need a QMB with Advantage?
Pairing an Advantage Special Needs Plan with your QMB is a great way to protect yourself from unexpected health costs. It also provides extra benefits at an affordable price.
