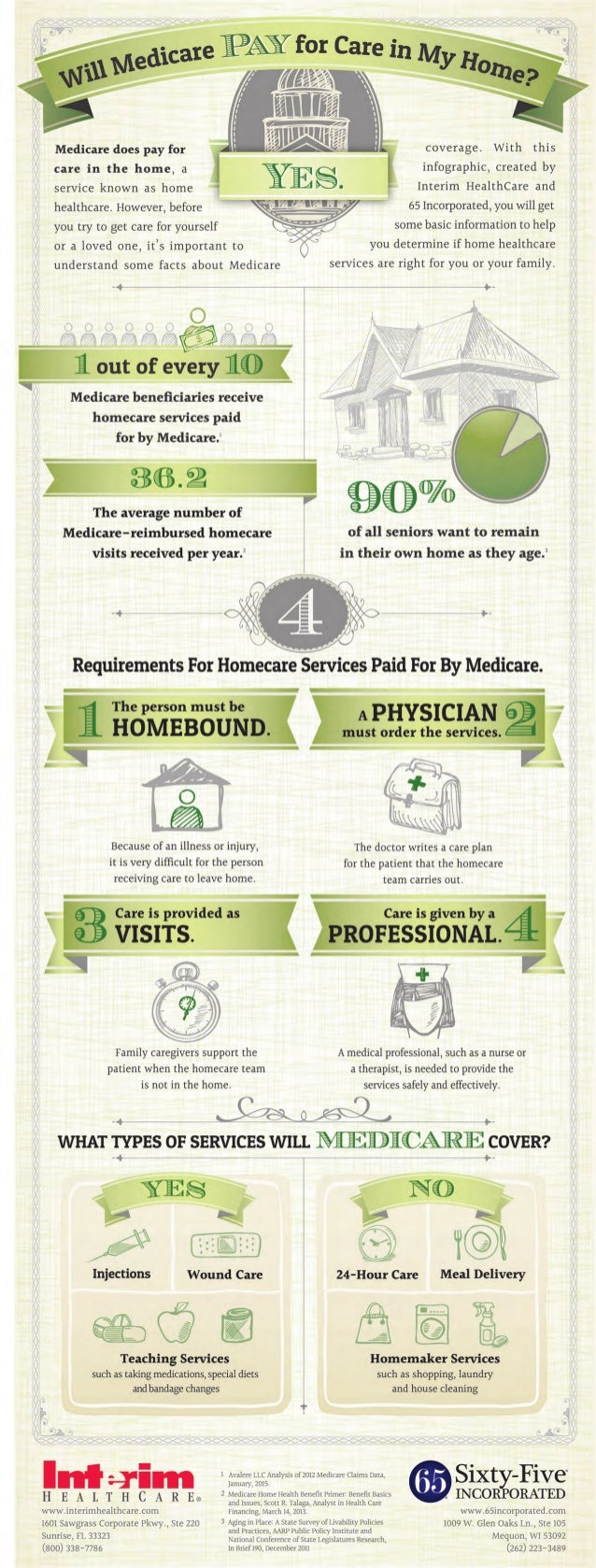
To qualify for home health benefits under original Medicare, a person must have a diagnosis and a relevant prescription from a qualified medical professional. Any home health services must be prescribed by a doctor and reasonably priced, so it’s important to check the costs of home health services in your area before choosing a provider.
Full Answer
How do I contact Medicare about home health care?
If you have questions about your Medicare home health care benefits or coverage and you have Original Medicare, visit Medicare.gov, or call 1-800-MEDICARE (1-800-633-4227). TTY users can call 1-877-486-2048.
How much does Medicare pay for home health care?
Your costs in Original Medicare $0 for home health care services. 20% of the Medicare-approved amount for Durable Medical Equipment (DME). Before you start getting your home health care, the home health agency should tell you how much Medicare will pay.
How do you pay for nursing home care?
There are several other ways you can pay for nursing home care: Medicaid. Medicaid is a joint federal and state program that helps with medical costs for some people with limited income and resources. Most health care costs are covered if you qualify for both Medicare and Medicaid. Most, but not all, nursing homes accept Medicaid payment.
How do I get help with Medicare benefits?
TTY users can call 1-877-486-2048. If you get your Medicare benefits through a Medicare Advantage Plan (Part C) or other Medicare health plan, call your plan. You may also call the State Health Insurance Assistance Program (SHIP).
How to find out if you have long term care insurance?
If you have long-term care insurance, check your policy or call the insurance company to find out if the care you need is covered. If you're shopping for long-term care insurance, find out which types of long-term care services and facilities the different policies cover.
Can federal employees buy long term care insurance?
Federal employees, members of the uniformed services, retirees, their spouses, and other qualified relatives may be able to buy long-term care insurance at discounted group rates. Get more information about long-term care insurance for federal employees.
Do nursing homes accept Medicaid?
Most, but not all, nursing homes accept Medicaid payment. Even if you pay out-of-pocket or with long-term care insurance, you may eventually "spend down" your assets while you’re at the nursing home, so it’s good to know if the nursing home you chose will accept Medicaid. Medicaid programs vary from state to state.
Does Medicare cover nursing home care?
Medicare generally doesn't cover Long-term care stays in a nursing home. Even if Medicare doesn’t cover your nursing home care, you’ll still need Medicare for hospital care, doctor services, and medical supplies while you’re in the nursing home.
Do you need a therapist for your aging parents?
You are doing everything you can for your aging parents, but sometimes it comes to the point where that is not enough. After a hospitalization, or to simply maintain or slow the decline of their health, Mom or Dad may need skilled therapists and nurses. This new twist in caring for Mom and Dad raises many questions.
Does Medicare cover home aides?
Medicare also covers continuous health care but on a different level. It only covers a percentage of the cost. Unfortunately, home aides that help with housework, bathing, dressing and meal preparations are not covered by Medicare.
What Is In-Home Care?
In-home care (also known as “home health care”) is a service covered by Medicare that allows skilled workers and therapists to enter your home and provide the services necessary to help you get better.
What Parts Of In-Home Care Are Covered?
In-home care can cover a wide range of services, but they’re not all covered by Medicare. According to the Medicare site, the in-home care services covered by parts A and B include:
How To Get Approved For In-Home Care
There are a handful of steps and qualifications you need to meet to have your in-home care covered by Medicare. It starts with the type of help your doctor says you or your loved one needs and includes other aspects of care.
Cashing In On In-Home Care
Once you qualify for in-home care, it’s time to find the right agency who will provide you or your loved one services. The company you receive your services from is up to you, but they must be approved by Medicare in order for their services to be covered.
How To Pay for In-Home Care Not Covered By Medicare
There may be times when not every part of your in-home care is covered. We already know 20 percent of the durable medical equipment needed to treat you is your responsibility, but there are other services like custodial care or extra round-the-clock care that won’t be covered by Medicare. This is where supplemental insurance (Medigap) comes in.
How do I contact Medicare for home health?
If you have questions about your Medicare home health care benefits or coverage and you have Original Medicare, visit Medicare.gov, or call 1-800-MEDICARE (1-800-633-4227) . TTY users can call 1-877-486-2048. If you get your Medicare benefits through a Medicare Advantage Plan (Part C) or other
What is an appeal in Medicare?
Appeal—An appeal is the action you can take if you disagree with a coverage or payment decision made by Medicare, your Medicare health plan, or your Medicare Prescription Drug Plan. You can appeal if Medicare or your plan denies one of these:
What happens when home health services end?
When all of your covered home health services are ending, you may have the right to a fast appeal if you think these services are ending too soon. During a fast appeal, an independent reviewer called a Beneficiary and Family Centered Care Quality Improvement Organization (BFCC-QIO) looks at your case and decides if you need your home health services to continue.
Why is home health important?
In general, the goal of home health care is to provide treatment for an illness or injury. Where possible, home health care helps you get better, regain your independence, and become as self-sucient as possible. Home health care may also help you maintain your current condition or level of function, or to slow decline.
Can Medicare take home health?
In general, most Medicare-certified home health agencies will accept all people with Medicare . An agency isn’t required to accept you if it can’t meet your medical needs. An agency shouldn’t refuse to take you because of your condition, unless the agency would also refuse to take other people with the same condition.
How to finance nursing home care?
In general, there are three ways you can finance long term care in a nursing home: pay for it from your own savings (self-insure), buy long-term care (LTC) insurance, or use government benefits. While all of this may sound pretty daunting, we want you to know that there is a way Medicare.org can help you.
What are the benefits of nursing home care?
If you meet certain eligibility requirements, three types of government benefits can help you pay the cost of nursing home care: Medicare, Medicaid, and veterans’ benefits. Medicare: Medicare does not cover the cost of custodial care in a nursing home or at home. However, it may help cover the costs ...
How much does Grant's LTC insurance cost?
Grant’s LTC insurance contract states that the company will pay for nursing home care beginning on the 16th day after care begins. Grant enters a nursing home that charges $125 a day. His total expenses for 60 days are $7,500. His insurance company sends him a check for $5,625 (45 x $125). The $5,625 he receives is excludable from his income for tax purposes when he files his annual income tax return.
Can you get treatment in a VA nursing home?
Secondly, you may be eligible for treatment in a Department of Veterans Affairs (VA) nursing home. You don’t have to have a service-connected illness or injury to get treatment, but since nursing home space is limited, veterans with service-connected conditions will be admitted first.
Can you take accelerated benefits from a nursing home?
If you are seriously ill, and the policy permits, you can take accelerated benefits from the policy. However, when you determine how much retirement income you will have and how much your nursing home costs will be, don’t forget to account for price increases and inflation. Consider also what will happen if your money runs out.
Can you liquidate your house?
You may be able to liquidate some investments or sell your house to come up with additional funds if you need to. You might also be able to borrow against your cash value life insurance policy. (Note that the death benefit available to your survivors will be reduced.)
Can a nursing home ask for a child's money?
It’s important to note that under federal law, it is illegal for a nursing home to ask a child to personally guarantee payment for your care . However, the nursing home may require you to prove you have the money to pay for your care by asking you to provide bank statements or by asking you to put down a deposit.
What are the eligibility requirements for Medicaid home care?
Eligibility Requirements for Medicaid Home Care. In order to be eligible for Medicaid, and hence, in-home care, there are eligibility requirements that must be met. In addition to being a resident in the state in which one applies, there are also financial and functional needs that must be met.
How much income can I have on Medicaid in 2021?
As a general rule of thumb, in 2021, 300% of SSI is used as the income limit. This means that an individual cannot have more than $2,382 / month in income. There is also an asset limit, which in most cases, is $2,000.
What is regular state medicaid?
With regular state Medicaid, also referred to as original Medicaid and classic Medicaid, the federal government requires that states make home health benefits available to those in need.
Do you need HCBS for nursing home?
On the other hand, for HCBS Medicaid waivers, a level of care consistent to that which is provided in a nursing home is generally required.
Can Medicaid recipients direct their own care?
Many states allow Medicaid recipients to direct their own in-home care. This model of receiving services is called consumer directed care, participant directed care, cash and counseling, and self-directed care, and often allows care recipients to hire relatives as paid caregivers. Some states even allow spouses to be hired, ...
Does Medicaid pay for nursing home care?
Yes, Medicaid will pay for in-home care, and does so in one form or another, in all 50 states. Traditionally, Medicaid has, and still continues to, pay for nursing home care for persons who demonstrate a functional and financial need. However, in-home care provides an alternative for seniors who require assistance to remain living at home, ...
Can you qualify for medicaid if you have over the income limit?
Being over the income and / or asset limit (s) does not mean that one cannot qualify for Medicaid. Certain higher end assets are generally exempt, or stated differently, not counted towards Medicaid’s asset limit. Examples include one’s home, household furnishings, vehicle, and engagement and wedding rings.
How much does a home health aide cost?
Cost of hiring a caregiver. A 2019 industry survey on home health costs found that a home health aide is likely to cost an average of $4,385 per month. The same survey listed the average monthly cost of a caregiver to provide custodial care services as $4,290.
What do you need to be a home health aide?
You need a home health aide to help care for you while you recover. The home health agency providing your care is Medicare-approved or certified.
What is a Medicare supplement?
If you think you or someone in your family might need custodial care, you may want to consider a long-term care insurance policy to help you cover the cost. A Medicare supplement (Medigap) plan may also help you pay some of the costs that Medicare won’t cover.
How long does Medicare Part A cover?
If you were admitted to the hospital for 3 consecutive days or Medicare covered your stay in a skilled nursing facility, Part A will cover home healthcare for 100 days, as long as you receive home health services within 14 days of leaving the hospital or nursing facility .
What is Medicare Part B?
Medicare Part B is medical coverage. If you need home health services but weren’t admitted to the hospital first, Part B covers your home healthcare. You do have to meet the other eligibility requirements, though.
How long do you have to see a doctor before you can get home health care?
To remain eligible for in-home care, you’ll need to see your doctor fewer than 90 days before or 30 days after you start receiving home healthcare services.
Does Medicare pay for physical therapy?
Physical therapy. If a physical therapist treats you in your home, Medicare is likely to pay for these kinds of services: assessment of your condition. gait training and exercises to help you recover from surgery, injuries, illnesses, or neurological conditions like stroke. postoperative wound care.
How much does a caregiver get paid per hour?
In very approximate terms, caregivers can expect to be paid between $9.00 – $19.25 per hour. It is important to note that the phrase “consumer direction” is not used in all states.
What is a medicaid waiver?
The first and most common Medicaid option is Medicaid Waivers. These are often called HCBS Waivers, short for Home and Community Based Services, or 1915 (c) Waivers or occasionally Section 1115 Waivers. Waivers allow states to pay for care and support services for individuals residing outside of nursing homes. Commonly, they pay for personal care (assistance with activities of daily living, such as eating, dressing, and mobility) and chore services provided for elderly or disabled persons who live in their homes or the homes of family members.
What is the caregiver exemption?
The Caregiver Exemption is also referred to as the Child Caregiver Exception. This option does not directly pay the adult child for their caregiving efforts on an hourly basis, but instead compensates them indirectly. To better understand this option, some background information on Medicaid eligibility is required. Eligibility for elderly persons is based largely on their income and their assets. One’s home, provided it is lived in by the Medicaid participant, is considered an exempt asset. However, if one moves from their home (into a nursing home, for example), then their home is no longer considered an exempt asset (unless their spouse lives there or the Medicaid recipient expresses an intent to return home). When the elderly person passes away, their state may try to take the home or some of the home’s value as reimbursement for the elderly person’s care. This is known as Medicaid Estate Recovery.
What is Medicaid estate recovery?
This is known as Medicaid Estate Recovery. The Caregiver Exemption allows the adult child who provides care for their elderly parent in their parent’s home to inherit the home, instead of the state taking the home under Estate Recovery rules. There are additional requirements.
What is the most common source of payment for family members?
Medicaid Options. Of all the programs that pay family members as caregivers, Medicaid is the most common source of payment. Medicaid has eligibility requirements that apply to the program participant and it has rules that dictate who is allowed to provide them with care.
How long do you have to live in a nursing home for an adult child?
There are additional requirements. The adult child must live in the home with their parent and provide care for at least two years. The level of care they provide must prevent their parent from being placed in a nursing home and they must have the medical documentation to validate this fact.
Does Medicaid pay for room and board?
In return, the adult children are compensated by Medicaid for their care services, but not for room and board. Medicaid, by law, cannot pay for room and board.
