The appeal can be filed at your local DHS office, in the following ways: Your local Family Community Resource Center can give you an appeal form and will help you fill it out, if you wish; You can email the completed form to [email protected]
How do I appeal a Medicare decision?
The appeals process has 5 levels. If you disagree with the decision made at any level of the process, you can generally go to the next level. At each level, you'll get instructions in the decision letter on how to move to the next level of appeal. Write your Medicare Number on all documents you submit with your appeal request.
What are my Medicare Advantage plan appeal rights?
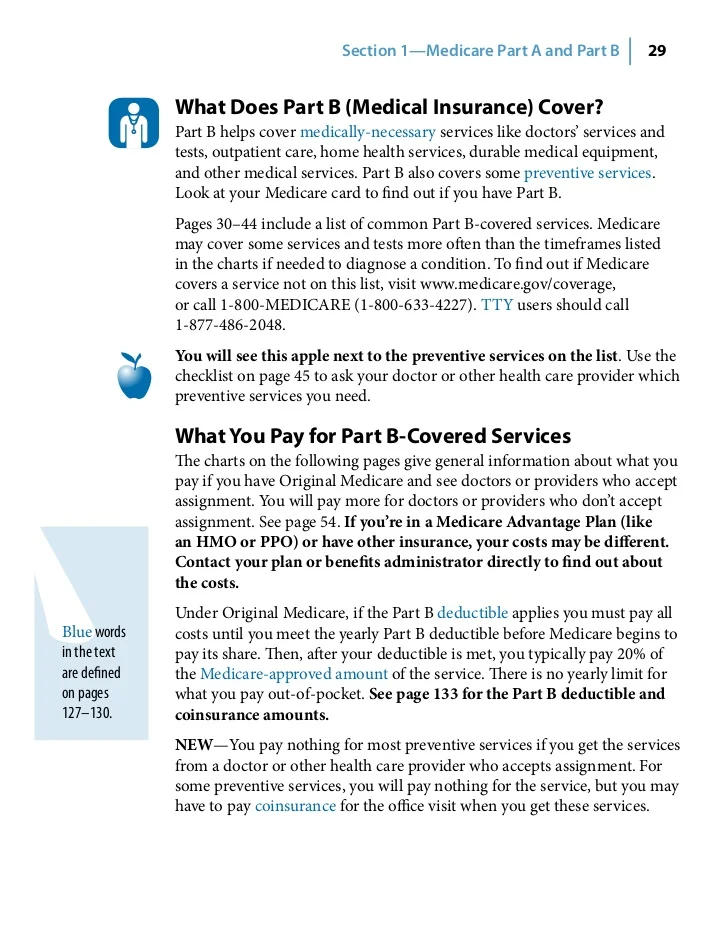
If you are enrolled in a Medicare Advantage Plan like an HMO or PPO, your appeal rights are explained in your plan’s materials. Your MSN tells you if Medicare has paid your medical claim or denied it. This is the initial determination, which is made by people at the company that handles Medicare billing.
How do I get a copy of my Medicare decision?
You can file a request for Appeals Council review in one of these ways: 1. Fill out a “Request for Review of an Administrative Law Judge (ALJ) Medicare Decision/Dismissal” form (DAB-101). To get a copy, visit hhs.gov/dab/divisions/dab101.pdf, or call 1-800-MEDICARE (1-800-633-4227) and ask for a copy.
Can I appeal my Medicare discharge too soon?
You have the right to a fast appeal if you think you’re being discharged too soon from your Medicare-covered inpatient hospital stay. Within 2 days of your hospital inpatient admission, you should get a notice called “An Important Message from Medicare about Your Rights” (sometimes called the “Important Message from Medicare” or the “IM”).
Can I appeal a Medicare decision?
An appeal is the action you can take if you disagree with a coverage or payment decision by Medicare or your Medicare plan. For example, you can appeal if Medicare or your plan denies: A request for a health care service, supply, item, or drug you think Medicare should cover.
How do I win a Medicare appeal?
Appeals with the best chances of winning are those where something was miscoded by a doctor or hospital, or where there is clear evidence that a doctor advised something and the patient followed that advice and then Medicare didn't agree with the doctor's recommendation.
How do I write a Medicare appeal letter?
The Medicare appeal letter format should include the beneficiary's name, their Medicare health insurance number, the claim number and specific item or service that is associated with the appeal, dates of service, name and location of the facility where the service was performed and the patient's signature.
What should I say in a Medicare appeal?
What are the steps for filing an appeal for original Medicare?your name and address.your Medicare number (as shown on your Medicare card)the items you want Medicare to pay for and the date you received the service or item.the name of your representative if someone is helping you manage your claim.More items...•
How often are Medicare appeals successful?
People have a strong chance of winning their Medicare appeal. According to Center, 80 percent of Medicare Part A appeals and 92 percent of Part B appeals turn out in favor of the person appealing.
What percentage of Medicare appeals are successful?
For the contracts we reviewed for 2014-16, beneficiaries and providers filed about 607,000 appeals for which denials were fully overturned and 42,000 appeals for which denials were partially overturned at the first level of appeal. This represents a 75 percent success rate (see exhibit 2).
What are the five steps in the Medicare appeals process?
The Social Security Act (the Act) establishes five levels to the Medicare appeals process: redetermination, reconsideration, Administrative Law Judge hearing, Medicare Appeals Council review, and judicial review in U.S. District Court. At the first level of the appeal process, the MAC processes the redetermination.
Who has the right to appeal denied Medicare claims?
You have the right to appeal any decision regarding your Medicare services. If Medicare does not pay for an item or service, or you do not receive an item or service you think you should, you can appeal. Ask your doctor or provider for a letter of support or related medical records that might help strengthen your case.
How long does it take Medicare to respond to an appeal?
about 60 daysHow Long Does a Medicare Appeal Take? You can expect a decision on your Medicare appeal within about 60 days. Officially known as a “Medicare Redetermination Notice,” the decision may come in a letter or an MSN. Medicare Advantage plans typically decide within 14 days.
How do I correct a rejected Medicare claim?
When a claim is denied because the information submitted was incorrect, often the claim can be reopened using a Clerical Error Reopening (CER). CERs can be used to fix errors resulting from human or mechanical errors on the part of the party or the contractor.
How do you appeal?
How to Write an Appeal Letter in 6 Simple StepsReview the appeal process if possible.Determine the mailing address of the recipient.Explain what occurred.Describe why it's unfair/unjust.Outline your desired outcome.If you haven't heard back in one week, follow-up.Appeal letter format.
What is the difference between reconsideration and redetermination?
Any party to the redetermination that is dissatisfied with the decision may request a reconsideration. A reconsideration is an independent review of the administrative record, including the initial determination and redetermination, by a Qualified Independent Contractor (QIC).
What are the steps in Medicare Part A and Part B appeal?
There are 5 steps in Part A and Part B appeals process: Redetermination by the company that handles bills for Medicare. Reconsideration by a Qualified Independent Contractor (QIC)
Can I appeal Medicare?
You have the right to file an appeal if you are found unqualified to participate in the Medicare program. You also may file an appeal if you believe that Medicare hasn't paid the proper amount for services, or if coverage has been denied. for a particular service.
File a complaint (grievance)
Find out how to file a complaint (also called a "grievance") if you have a concern about the quality of care or other services you get from a Medicare provider. Contact your State Health Insurance Assistance Program (SHIP) for local, personalized Medicare counseling.
File a claim
Get information on how and when to file a claim for your Medicare bills (sometimes called "Medicare billing"). You should only need to file a claim in very rare cases.
Check the status of a claim
Check your claim status with your secure Medicare account, your Medicare Summary Notice (MSN), your Explanation of Benefits (EOB), Medicare's Blue Button, or contact your plan.
File an appeal
How to appeal a coverage or payment decision made by Medicare, your health plan, drug plan or Medicare Medical Savings Account (MSA) Plan.
Your right to a fast appeal
Learn how to get a fast appeal for Medicare-covered services you get that are about to stop.
Authorization to Disclose Personal Health Information
Access a form so that someone who helps you with your Medicare can get information on your behalf.
What to do if you are not satisfied with the IRE decision?
If you’re not satisfied with the IRE’s reconsideration decision, you may request a decision by OMHA, based on a hearing before an Administrative Law Judge (ALJ) or, in certain circumstances, a review of the appeal record by an ALJ or an attorney adjudicator.
What to do if you are not satisfied with QIC?
If you’re not satisfied with the QIC’s reconsideration decision, you may request a decision by OMHA, based on a hearing before an Administrative Law Judge (ALJ) or , in certain circumstances, a review of the appeal record by an ALJ or attorney adjudicator.
What happens if you disagree with a decision?
If you disagree with the decision made at any level of the process, you can generally go to the next level. At each level, you’ll get instructions on how to move to the next level of appeal.
What is a home health change of care notice?
The “Home Health Change of Care Notice” is a written notice that your home health agency should give you when your home health plan of care is changing because of one of these:
How long does it take for an IRE to review a case?
They must get this information within 10 days after the date you get the notice telling you your case file has been sent to the IRE. The IRE’s address is on the notice.
Do doctors have to give advance notice of non-coverage?
Doctors, other health care providers, and suppliers don’t have to (but still may) give you an “Advance Beneficiary Notice of Noncoverage” for services that Medicare generally doesn’t cover, like:
Does CMS exclude or deny benefits?
The Centers for Medicare & Medicaid Services (CMS) doesn’t exclude, deny benefits to, or otherwise discriminate against any person on the basis of race, color, national origin, disability, sex, or age in admission to, participation in, or receipt of the services and benefits under any of its programs and activities, whether carried out by CMS directly or through a contractor or any other entity with which CMS arranges to carry out its programs and activities.
Overview Of Medicare Appeals Process
If you disagree with a decision by Medicare on whether to provide coverage or payment for a certain medical service, then you have certain appeal rights. You can make an appeal request for Medicare to reconsider their decision. There are five levels to the appeals process although they may not all be necessary for your specific appeal.
Five Levels Of Medicare Appeals
Similar to the court system, there are different levels of appeals in Medicare. If you are unsuccessful at one level, then you can appeal to the next level. If you go all the way to the top, you could end up in Federal court. In practice though, very few appeals make it that far. Here are the different levels and what you need to know about each.
How Long Do You Have To File An Appeal?
The answer depends on which stage of the process you are currently in. Initially, you should look at your Medicare Summary Notice (MSN) for the claim that you wish to appeal. It will have a date printed on it by which you must file your first level appeal. Generally, this date is 120 days from the date you received the initial determination.
Tips For Winning Your Appeal
We know that you want to win your appeal or else you would not be filing it in the first place. There are some things that you should keep in mind when filing appeals with the Centers for Medicare & Medicaid Services. If you keep these tips in mind, it can greatly increase your odds of being successful.
The Bottom Line
If you disagree with a decision by Medicare whether to cover a service or how much to pay, then you have a right to file an appeal. It could be nearly any decision that they make from whether to pay for care in a skilled nursing facility to whether a prescription drug is medically necessary.
How successful are Medicare appeals?
Medicare appeals are actually quite successful. In fact, data has shown that roughly 80% to 90% of appeals are won by the claimant who is appealing the decision. If you do not win your appeal at the first or second level, do not give up. Keep going as far in the appeals process as possible to increase your odds of ultimately winning your appeal.
How long does Medicare have to respond to an appeal?
It depends on which stage of the appeals process you are on. For Level 1, the general timeframe to respond to the appeal is 60 days. At level 2, the decision is again made within 60 days. If a decision cannot be reached in this timeframe, you will still receive notice of your rights in the appeals process.
What is a Medicare representative?
Your name, address, phone number, and Medicare Number. A statement appointing someone as your representative. The name, address, and phone number of your representative. The professional status of your representative (like a doctor) or their relationship to you. A statement authorizing the release of your personal and identifiable health ...
What is MAC in Medicare?
Send the representative form or written request with your appeal to the Medicare Administrative Contractor (MAC) (the company that handles claims for Medicare ), or your Medicare health plan. If you have questions about appointing ...
Who can act for you on a medical appeal?
You or your appointed representative (someone you name to act for you) may ask for a medical appeal. You can name a relative, friend, attorney, doctor, or someone else to act for you with an Appointment of Representative form. Under state law, others may already be allowed to act for you.
How to request a fast medical appeal?
Fast Medical (Expedited) Appeals. You or your doctor (without an appointment of representative form) can request a Fast Medical Appeal by phone or mail if waiting for a Standard Appeal could harm your health or your ability to function. You can get one: For medical care you have not yet received.
What is an appeal in insurance?
What is an appeal? An appeal, or redetermination, is a formal way to ask the plan to review a coverage decision about health care services and/or prescription drugs. You may ask for a review when you are not satisfied with our initial coverage decision.
How long does it take to get a fast appeal for a prescription?
If you are asking for a Fast Appeal for prescription drugs, we will give you an answer within 72 hours of receipt of your request.
What happens if you don't agree with a judge's decision?
If you do not agree with the decision the judge makes, you can move on to a Level 4 Appeal. At the Level 4 Appeal, the Medicare Appeals Council, who works for the federal government, will review your appeal and give you an answer.
What level do you have to appeal a fast track?
If you had a Fast Track Appeal at Level 1, you will have a Fast Track Appeal at Level 2. The time frames for a Fast and Standard Appeal at Level 2 are the same as for the initial appeal. If our plan denies your appeal for a Part D prescription drug, you will need to choose whether to accept this decision or appeal it to Level 2.
How long does it take to get an appointment of representative for Medicare?
Under state law, others may already be allowed to act for you. Get an Appointment of Representative form [PDF] You must make your request within 60 days from the date of the coverage determination. A coverage determination is the first decision made by your Medicare drug plan (not the pharmacy) about your drug benefits.
Where to file an appeal in Illinois?
You can file an appeal by writing to the Bureau of Hearings, 69 W. Washington, 4th Floor, Chicago, Il 60602; Or you may call 1-800-435-0774 (TTY: 1-877-734-7429).
How long do you have to appeal a Medicaid denial?
To continue Medicaid benefits during an appeal, you must appeal within 10 days of the date of the notice of change or before the date the change becomes effective (the date the change becomes effective is included on the notice of change).
What to do if your medicaid is turned down?
If your application for Medicaid is turned down, you can appeal and ask for a fair hearing. To learn more about the rules that DHS has to follow for Medicaid applications, you can read the Cash, SNAP, and Medical Policy Manual.
What happens if DHS does not approve your request?
If DHS does not approve your request at the pre- hearing stage, they will schedule a fair hearing. At the hearing you will have the opportunity to present your case before a hearing officer, and DHS will then issue a written decision. At the hearing, you have the following rights: To be represented by a lawyer, a friend or relative.
What rights do you have at a hearing?
At the hearing, you have the following rights: To be represented by a lawyer, a friend or relative. To bring in witnesses. To show documents supporting your case, such as medical records and your doctor's’ statements.
Can Medicaid sue an estate?
Medicaid can sue an estate to recover money spent on care. Prescription policy for Medicaid. Being denied Medicaid coverage with a disability. Being billed for services you think are covered by Medicaid. Spend-down process for Medicaid. Only logged-in users can post comments.