To get reimbursed, the person should take the following steps (first check with your Medicare Part D plan's Member Services department to see if a network pharmacy is nearby - the toll-free number for Member Services is printed on your Member ID card): Save the original receipt from the drug purchase.
Full Answer
Do you get a monthly Medicare payment receipt?
Mar 22, 2021 · Sign up for Medicare Easy Pay with the following steps: Type your username and password into the MyMedicare account page. Select “My Premiums” from the navigation menu at the top of the screen, then choose “Sign Up.” Complete the …
How do I Pay my Medicare premiums?
Feb 16, 2016 · The effective date of the Open Season change is the first day of the first full pay period in January. For annuitants this date will always be January 1. Also, the Medicare Part B premium comes out of the Social Security check and not the annuity check so the payment receipt would have to come from SSA.
How do I request reimbursement from my doctor?
Jul 27, 2021 · If you want Medicare to pay for your care, you’ll need to send a form to request reimbursement. Seeing a Non-participating Doctor. These doctors accept Medicare patients, but they haven’t agreed to Medicare’s rates. They may choose to accept Medicare rates in your case, or they may decide to bill you up to 15% more than the Medicare rate.
Where can I find more information about Medicare bill pay?
People with Original Medicare will receive a Medicare Summary Notice (MSN) in the mail every three months for their Medicare Parts A and B-covered services. This is strictly a notice, not a bill. (If you are enrolled in a Medicare Advantage plan, you will receive an Explanation of Benefits (EOB) if you get care covered by your plan.) The MSN shows: All your services or supplies that …
How do I get proof of Medicare payments?
Frequently Asked Questions What can I use as proof of eligible Medicare premium expenses? The easiest receipt for you to use as proof of eligible expenses is the annual statement you receive from Social Security for the upcoming calendar year.
How do I get proof of payment from Medicare Part B?
What can I do? You can call or visit your local Social Security Administration (SSA) office. You can also access proof of your 2020 Medicare Part B basic premium online at the SSA website: https://www.ssa.gov/myaccount/. You may be required to create or register your SSA account.
Can I view my Medicare payments online?
You can find more information at Medicare.gov or CMS's online bill pay webpage. Remember, CMS does not charge a fee for processing the electronic payments, but in some situations, a bank may charge their customers a fee for using their online bill payment service.Aug 3, 2017
Can I view my Medicare EOB online?
Your explanation of benefits, also called an EOB, is an important tool to help you keep track of your plan usage. Every time you get a new Medicare medical or Part D prescription coverage explanation of benefits, you can save time and paper by signing up to view them online.Jul 24, 2018
How do I get $148 back from Medicare?
How do I qualify for the giveback?Are enrolled in Part A and Part B.Do not rely on government or other assistance for your Part B premium.Live in the zip code service area of a plan that offers this program.Enroll in an MA plan that provides a giveback benefit.Jan 14, 2022
Will Medicare send me a bill for Part B?
If you're not collecting Social Security or Railroad Retirement Board benefits, you'll receive a bill from Medicare for your Part B premium. If you pay a Part A premium, you'll also receive a bill from Medicare.
How do I get a copy of my Medicare Summary Notice?
Log into (or create) your Medicare account. Select "Get your Medicare Summary Notices (MSNs) electronically" under the "My messages" section at the top of your account homepage. You'll come to the "My communication preferences" page where you can select "Yes" under "Change eMSN preference," then "Submit."
How do I know if Medicare received my payment?
For questions about your Medicare bill or if your payment was processed:Log into (or create) your Medicare account. Select “My premiums,” then, “Payment history.”Call us at 1-800-MEDICARE (1-800-633-4227). TTY: 1-877-486-2048.
How often does Medicare mail Paper Summary Medicare notices?
You'll get your MSN every 3 months if you get any services or medical supplies during that 3-month period.
Can you go paperless with Medicare?
Medicare has been improving its paperless billing options, and you can now choose to receive your Medicare Summary Notices and the Medicare & You handbook electronically.
What is Medicare Reimbursement?
If you’re on Medicare, your doctors will usually bill Medicare for any care you obtain. Medicare will then pay its rate directly to your doctor. Your doctor will only charge you for any copay, deductible, or coinsurance you owe.
How to Get Reimbursed From Medicare
To get reimbursement, you must send in a completed claim form and an itemized bill that supports your claim. It includes detailed instructions for submitting your request. You can fill it out on your computer and print it out. You can print it and fill it out by hand.
How to Get Help with Medicare Reimbursement
If you're looking for the best Medicare supplement plans, MedicareFAQ can help. Our agents research multiple companies and policies to give you a quote that's right for you. When you have a policy through us, our client care team can help you with any policy issues or inconveniences.
What is it?
It's not a bill. It’s a notice that people with Original Medicare get in the mail every 3 months for their Medicare Part A and Part B-covered services.
When should I get it?
You’ll get your MSN every 3 months if you get any services or medical supplies during that 3-month period. If you don’t get any services or medical supplies during that 3-month period you won’t get an MSN for that particular 3-month period.
Who sends it?
If you're not sure if your MSN is from Medicare, look for these things on the MSN envelope. [PDF, 380 KB]
What should I do if I get this notice?
If you have other insurance, check to see if it covers anything that Medicare didn’t.
Medicare summary notice
People with Original Medicare will receive a Medicare Summary Notice (MSN) in the mail every three months for their Medicare Parts A and B-covered services. This is strictly a notice, not a bill. (If you are enrolled in a Medicare Advantage plan, you will receive an Explanation of Benefits (EOB) if you get care covered by your plan.)
When you'll receive it
Every three months, Medicare will send you an MSN, but only if you received services or medical supplies during that three-month period.
What to do with the notice
If you have other insurance, check to see if it covers anything that Medicare didn’t.
For those who qualify, there are multiple ways to have your Medicare Part B premium paid
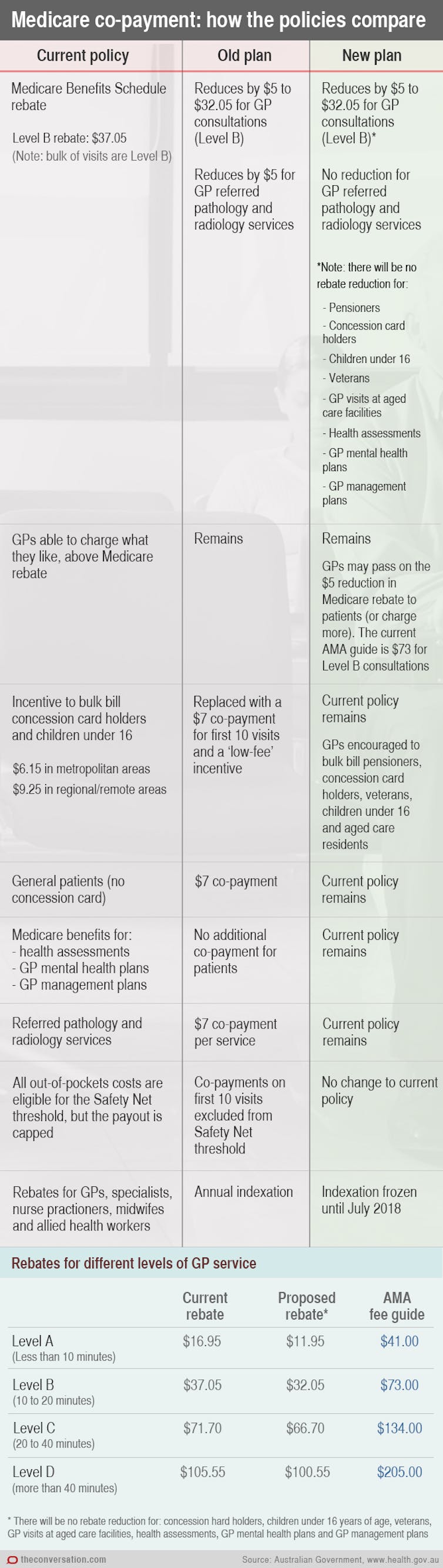
In 2022, the standard Medicare Part B monthly premium is $170.10. Beneficiaries also have a $233 deductible, and once they meet the deductible, must typically pay 20% of the Medicare-approved amount for any medical services and supplies.
What is the Part B premium reduction benefit?
The giveback benefit, or Part B premium reduction, is when a Part C Medicare Advantage (MA) plan reduces the amount you pay toward your Part B monthly premium. Your reimbursement amount could range from less than $1 to the full premium amount, which is $170.10 in 2022.
How to find plans that offer the giveback benefit
Not all MA plans offer this benefit, so you must find a plan that does in order to take advantage of the opportunity. In 2022, these plans are offered in nearly all states, so you may find one close to you.
Other Part B reimbursement options
There are other ways you can lower or eliminate how much you pay for the Medicare Part B premium. This includes certain Medicaid programs or benefits from some retiree health plans.
What Is It?
- It's not a bill. It’s a notice that people with Original Medicare get in the mail every 3 months for their Medicare Part A and Part B-covered services. The MSN shows: 1. All your services or supplies that providers and suppliers billed to Medicare during the 3-month period 2. What Medicare paid 3. The maximum amount you may owe the provider
When Should I Get It?
- You’ll get your MSN every 3 months if you get any services or medical supplies during that 3-month period. If you don’t get any services or medical supplies during that 3-month period you won’t get an MSN for that particular 3-month period. If I need to change my address: Contact Social Security. If you get RRB benefits, contact the RRB.
Who Sends It?
- Medicare If you're not sure if your MSN is from Medicare, look for these things on the MSN envelope. [PDF, 380 KB]
What Should I Do If I Get This Notice?
- If you have other insurance, check to see if it covers anything that Medicare didn’t.
- Keep your receipts and bills, and compare them to your MSN to be sure you got all the services, supplies, or equipment listed.
- If you paid a bill before you got your notice, compare your MSN with the bill to make sure you paid the right amount for your services.
- If you have other insurance, check to see if it covers anything that Medicare didn’t.
- Keep your receipts and bills, and compare them to your MSN to be sure you got all the services, supplies, or equipment listed.
- If you paid a bill before you got your notice, compare your MSN with the bill to make sure you paid the right amount for your services.
- If an item or service is denied, call your doctor’s or other health care provider's office to make sure they submitted the correct information. If not, the office may resubmit. If you disagree with...