How do I know if a test is covered by Medicare?
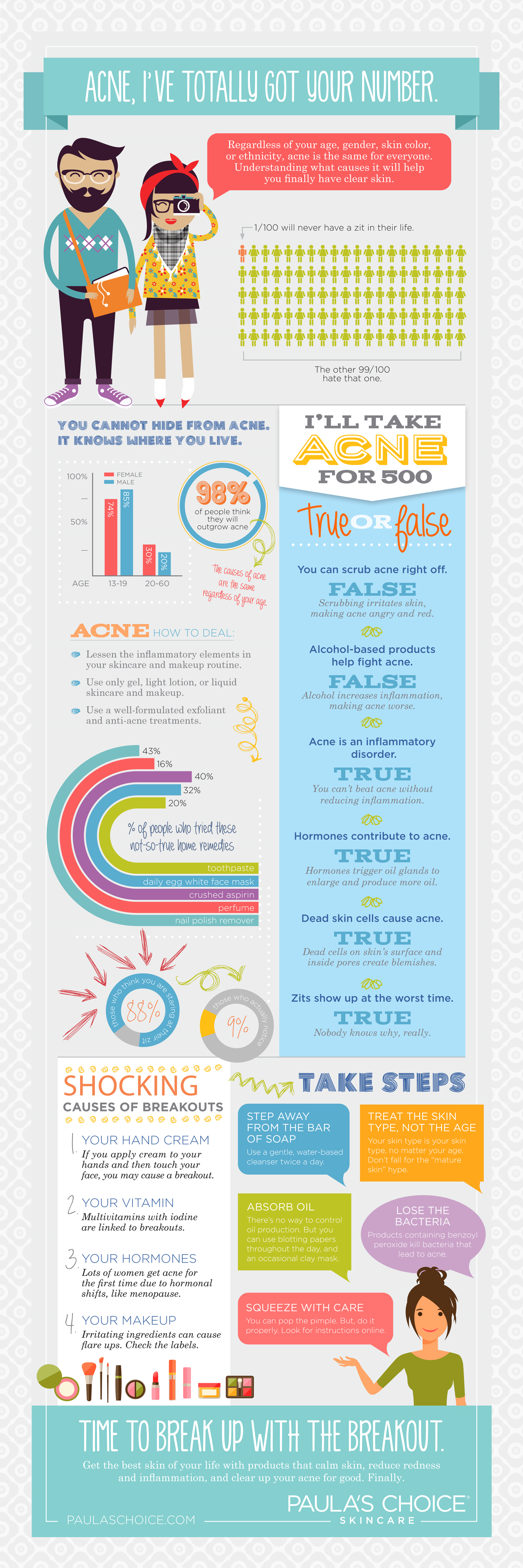
You usually pay nothing for Medicare-covered clinical diagnostic laboratory tests. What it is Diagnostic laboratory tests look for changes in your health and help your doctor diagnose or rule out a suspected illness or condition. Things to know Medicare also covers some preventive tests and screenings to help prevent or find a medical problem.
How much do blood tests cost with Medicare?
Apr 04, 2022 · You should check whether your pharmacy or health care provider is participating in the initiative, in which case they will bill Medicare for the over-the-counter test on your behalf. When does this initiative end? Medicare will pay for up to eight free over-the-counter COVID-19 tests per calendar month through this initiative as long as the COVID-19 PHE continues.
Does Medicare cover diagnostic laboratory tests?
Nov 23, 2021 · Medicare expands a number of services for COVID-19 coverage. Because the COVID-19 test is considered a clinical diagnostic laboratory test (no matter where it is actually administered), it is provided with no cost sharing. That means you will not have to pay anything toward your annual Part B deductible or any Part B coinsurance for the test.
What to do if a service is not listed on Medicare?
Mar 04, 2021 · Medicare offers a tool you can use to check which tests are covered. You can also go here to look through the list of covered tests from Medicare. You can look through lists of codes and items...
Will I have to pay for my COVID-19 test up front?
See full answerThe Biden-Harris Administration is strongly incentivizing health plans and insurers to set up a network of convenient locations across the country such as pharmacies or retailers where people with private health coverage will be able to order online or walk in and pick up at-home over-the-counter COVID-19 tests for free, rather than going through the process of having to submit claims for reimbursement. Consumers can find out from their plan or insurer if it provides direct coverage of over-the-counter COVID-19 tests through such a program or whether they will need to submit a claim for reimbursement. If you are charged for your test after January 15, keep your receipt and submit a claim to your insurance company for reimbursement.Jan 12, 2022
How much does a COVID-19 test cost?
The cost for testing should be covered by most insurance plans or through government-sponsored programs.For private pay patients, please contact your health care provider for cost to administer a COVID-19 test.
How many COVID-19 tests can I get reimbursed for?
Health plans must cover 8 individual at-home over-the-counter COVID-19 tests per person enrolled in the plan per month. That means a family of four can get 32 tests per month for free.Jan 12, 2022
What is a self-home test for COVID-19?
Self-tests for COVID-19 give rapid results and can be taken anywhere, regardless of your vaccination status or whether or not you have symptoms. They detect current infection and are sometimes also called “home tests,” “at-home tests,” or “over-the-counter (OTC) tests.”
Does CVS offer COVID-19 testing?
CVS provides laboratory-based nucleic acid amplification testing (NAAT) and rapid point-of-care (POC) testing at no cost to consumers at over 700 locations in 44 states, Washington DC, and Puerto Rico. Locations include community testing sites and some CVS pharmacies.Feb 4, 2022
How should you take a COVID-19 rapid test?
Please don't go sticking that #COVID19 testing swab down your throat. Use swabs as instructed: via the nose. FACT: When it comes to at-home rapid antigen #COVID19 tests, those swabs are for your nose and not your throat.Jan 11, 2022
What if I can’t afford to pay for the at-home over-the-counter COVID-19 test(s) upfront?
See full answerHealth plans and insurers are strongly incentivized to set up a network of convenient options across the country, such as pharmacies and retailers, where people will be able to order online or walk in and pick up at-home over-the-counter COVID-19 tests for free rather than going through the process of having to submit claims for reimbursement. Consumers can find out from their plan or insurer if it is providing direct coverage of over-the-counter COVID-19 tests through such a network of preferred pharmacies or retailers.You can also access free testing in the community. A list of community-based testing sites can be found here. COVID-19 tests are also available without cost-sharing to covered individuals when administered by a health care provider like a nurse, doctor, or pharmacist, without limitation.Jan 12, 2022
Do I qualify for the additional $300 in COVID-19 unemployment benefits?
The additional $300/week in Federal Pandemic Unemployment Compensation is available to claimants receiving unemployment benefits under the state or federal regular unemployment compensation programs (UCFE, UCX, PEUC, PUA, EB, STC, TRA, DUA, and SEA). The funds are available for any weeks of unemployment beginning after Dec. 26, 2020, and ending on or before March 14, 2021. You don’t need to apply separately to receive this supplemental amount.Jan 11, 2021
What are the risks of false negative COVID-19 results?
Risks to a patient of a false negative result include: delayed or lack of supportive treatment, lack of monitoring of infected individuals and their household or other close contacts for symptoms resulting in increased risk of spread of COVID-19 within the community, or other unintended adverse events.Jul 15, 2021
Where can I find a location that has at-home over-the-counter COVID-19 tests?
Consumers can visit stores online or in-person. The Biden-Harris Administration is also strongly incentivizing health plans and insurers to set up a network of convenient options across the country like pharmacies or retailers, including online retailers, where people can get COVID-19 tests for free at the point of sale, rather than having to submit claims for reimbursement. Consumers can find out from their plan or insurer if it is providing direct coverage of over-the-counter COVID-19 tests through such a network of preferred pharmacies or retailers.Jan 12, 2022
Are COVID-19 self-tests reliable?
Positive results from self-tests are highly reliable. Negative results from self-tests do not rule out SARS-CoV-2 infection. A negative self-test result may not be reliable, especially if you have symptoms associated with COVID-19.
What is the difference between a COVID-19 rapid Point-of-Care test and a self-test?
Rapid Point-of-Care tests, test performed or interpreted by someone other than the individual being tested, can be performed in minutes and can include antigen and some NAATs. Self-tests are rapid tests that can be taken at home or anywhere, are easy to use, and produce rapid results.
Medicare Expert Q&A: Does Medicare Cover COVID-19 Tests?
Medicare expert Christian Worstell details how Medicare covers COVID-19 testing, treatment and services during the coronavirus pandemic.
Learn More About Medicare
Join our email series to receive your free Medicare guide and the latest information about Medicare and Medicare Advantage.
What this means for Medicare beneficiaries
In the near future, all Medicare beneficiaries will be able to get up to eight over-the-counter COVID-19 tests per month at no cost. Tests will be made available at participating pharmacies and other retail locations.
Additional free test and mask resources
The Biden Administration is also mailing free at-home test kits to all Americans -- regardless of their health insurance status. Tests can be requested at COVIDTests.gov and will be shipped directly to homes.
Keep your finances in mind
The pandemic has created added stress for many Americans, including financial stress. If you're looking to keep extra spending to a minimum, take advantage of available free and low-cost COVID-19 resources like the programs mentioned above.
Top credit card wipes out interest into 2023
If you have credit card debt, transferring it to this top balance transfer card secures you a 0% intro APR into 2023! Plus, you’ll pay no annual fee. Those are just a few reasons why our experts rate this card as a top pick to help get control of your debt. Read The Ascent's full review for free and apply in just 2 minutes.
About the Author
Natasha specializes in credit card and rewards content. Her goal is to encourage more people to experience the world around them while making smart financial choices.
What is Medicare Part A?
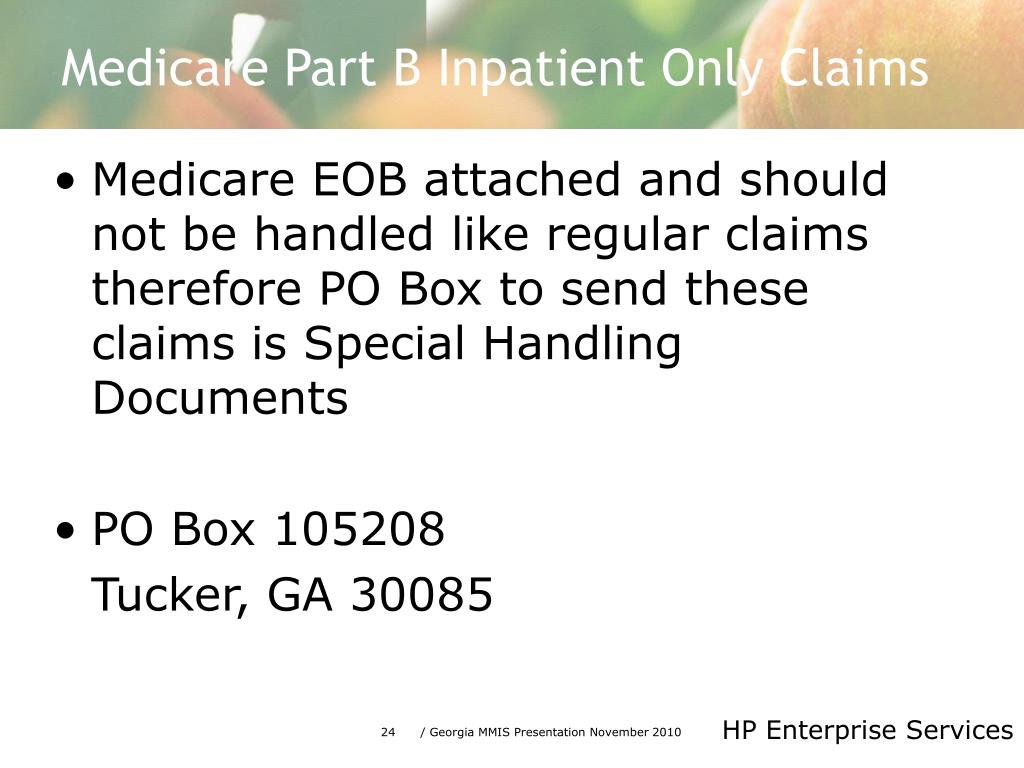
Medicare Part A offers coverage for medically necessary blood tests. Tests can be ordered by a physician for inpatient hospital, skilled nursing, hospice, home health, and other related covered services. Medicare Part B covers outpatient blood tests ordered by a physician with a medically necessary diagnosis based on Medicare coverage guidelines.
How often does Medicare cover mammograms?
once a year if you meet criteria. *Medicare covers diagnostic mammograms more often if your doctor orders them. You are responsible for the 20 percent coinsurance cost. Other nonlaboratory diagnostic screenings Medicare covers include X-rays, PET scans, MRI, EKG, and CT scans.
What is the purpose of blood test?
Blood tests are an important diagnostic tool doctors use to screen for risk factors and monitor health conditions. A blood test is generally a simple procedure to measure how your body is functioning and find any early warning signs. Medicare covers many types of blood tests. Trusted Source.
How much is Medicare Part B 2021?
You have to meet your annual deductible for this coverage as well. In 2021, the deductible is $203 for most people. Remember, you also have to pay your monthly Part B premium, which is $148.50 in 2021 for most beneficiaries.
Does Medicare cover 20 percent coinsurance?
You have to pay your 20 percent coinsurance as well as your deductible and any copays. Remember to go to providers that accept assignment to avoid charges Medicare won’t cover. Helpful links and tools. Medicare offers a tool you can use to check which tests are covered.
Does Medicare cover ABN?
Medicare offers a tool you can use to check which tests are covered. You can also go here to look through the list of covered tests from Medicare. You can look through lists of codes and items Medicare does not cover. Before signing an ABN, ask about the cost of the test and shop around.
Does Medicare Advantage cover blood work?
Medicare Advantage, or Part C, plans also cover blood tests. These plans may also cover additional tests not covered by original Medicare (parts A and B). Each Medicare Advantage plan offers different benefits, so check with your plan about specific blood tests. Also consider going to in-network doctors and labs to get the maximum benefits.
How much is Medicare Part A?
Part A. For Medicare Part A, which covers eligible inpatient care, a person is responsible for a deductible of $1,408 per benefit period. After an individual has paid the deductible, Medicare covers all eligible hospital costs for the first 60 days that a person is an inpatient, without charging a coinsurance.
How much is Medicare Part B deductible?
Part B. Medicare Part B has an annual deductible of $198. After meeting the deductible, Medicare pays 80% of allowable charges for medically necessary services. An individual is responsible for the remaining 20% coinsurance.
How long does it take for antibodies to return?
In the case of either a false positive or false negative test, a repeat test may be recommended by a doctor. The results of an antibody test can take 1–2 days to return. At this time, scientists do not know if the antibodies developed after an infection can protect a person from becoming unwell in the future.
How does LabCorp work?
A person receives the kit by mail, after which they collect a sample from their nose. The kit must then be returned to the lab by mail for testing. LabCorp will send a bill to a person’s health plan or use government funds to cover people who are not insured, but no charges will be made to individuals directly.
What is the difference between a viral and antibody test?
The viral test shows an active infection. An antibody test shows a past infection. For a viral test, a healthcare provider will take a sample swab from inside the nose. For an antibody test, a doctor orders a blood test.
How long does it take for a nose test to be returned?
The FDA has approved home test kits that enable people to collect a sample from their nose and mail it to a lab. Results are also usually returned in 1–3 days after the company receives the sample.
How long does it take for PCR results to come back?
One type of test, the PCR test, uses samples taken from the nose to check for infection. Results take from 1–3 days to return. Those who use the home test kits also get their results 1–3 days after the lab receives the sample.
How does the immune system work with TB?
Once TB bacteria enters the body, your immune system works to fight against the bacteria as it tries to grow and prevent it from becoming an active disease. While the bacteria will always remain present in the body, a successful immune response relieves you of any symptoms.
Can TB spread to others?
People with latent TB infection cannot spread the disease to others. Active TB disease can still occur if your immune system weakens enough to allow the bacteria to grow and spread. Once this happens, you may experience the following symptoms: Persistent cough for 3 weeks or longer. Blood or mucus when coughing.
Can health care workers get TB?
Health care workers may be exposed to active TB disease while caring for infected patients. Health. Medical conditions that weaken the immune system may mean a person has a higher chance of experiencing active TB disease if they are exposed to the bacteria. Travel.
Can you get a blood test for TB?
Because people who have previously received a tuberculosis vaccination can have a false-positive reaction to the skin test for TB, a blood test may be ordered instead. Additional testing may be required in either case to determine if the patient has a latent or active version of the disease.
What This Means For Medicare Beneficiaries
- In the near future, all Medicare beneficiaries will be able to get up to eight over-the-counter COVID-19 tests per month at no cost. Tests will be made available at participating pharmacies and other retail locations. Those eligible won't need to first pay for tests and then seek reimbursement. Instead, they will be able to pick up tests for free without paying out-of-pocket c…
Additional Free Test and Mask Resources
- The Biden Administration is also mailing free at-home test kitsto all Americans -- regardless of their health insurance status. Tests can be requested at COVIDTests.gov and will be shipped directly to homes. Each household will receive four free over-the-counter COVID-19 tests. If you have yet to request your tests, be sure to take advantage of this free resource. At-home test kits …
Keep Your Finances in Mind
- The pandemic has created added stress for many Americans, including financial stress. If you're looking to keep extra spending to a minimum, take advantage of available free and low-cost COVID-19 resources like the programs mentioned above. Even if money is tight, you can make small changes that benefit your financial situation. Over time, these changes can add up. For ad…