Njoyoc67, trying calling the State Medicaid
Medicaid
Medicaid in the United States is a federal and state program that helps with medical costs for some people with limited income and resources. Medicaid also offers benefits not normally covered by Medicare, including nursing home care and personal care services. The Health Insurance As…
How do I know if I am eligible for Medicaid?
Enter your household size and state. We'll tell you who is eligible for Medicaid, if your state expanded and if you qualify for Medicaid based only on your income. If you think you have Medicaid eligibility, you can create an account and fill out a Marketplace application.
Should you know about Medicaid if you have elderly parents?
If you have elderly parents, don’t wait to learn about Medicaid — sometimes referred to by a litany of other state names, like Medi-Cal and MassHealth.
Do I qualify for Medicaid based only on my income?
But if your state has expanded Medicaid coverage, you can qualify based on your income alone. Enter your household size and state. We'll tell you who is eligible for Medicaid, if your state expanded and if you qualify for Medicaid based only on your income.
How do I find out what Medicare coverage I have?
Fill out the requested information, including your zip code, Medicare number, name, date of birth and your effective date for Medicare Part A coverage or Part B coverage. Click “Continue,” and you should be taken to a page that shows the the coverage that you have. If you just recently enrolled, it may not be immediately reflected online.
How do I find out if a patient has Medicare?
The best way to check eligibility and enroll in Medicare online is to use the Social Security or Medicare websites. They are government portals for signing up for Medicare, and they offer free information about eligibility.
How do you determine which insurance is primary?
Primary insurance is a health insurance plan that covers a person as an employee, subscriber, or member. Primary insurance is billed first when you receive health care. For example, health insurance you receive through your employer is typically your primary insurance.
What is the difference in Medicare and Medicaid?
The difference between Medicaid and Medicare is that Medicaid is managed by states and is based on income. Medicare is managed by the federal government and is mainly based on age. But there are special circumstances, like certain disabilities, that may allow younger people to get Medicare.
Do I automatically get Medicare when I turn 65?
You automatically get Medicare when you turn 65 Part A covers inpatient hospital stays, skilled nursing facility care, hospice care, and some home health care. Part B covers certain doctors' services, outpatient care, medical supplies, and preventive services.
How do I know if my Medicare is primary or secondary?
Medicare pays first and your group health plan (retiree) coverage pays second . If the employer has 100 or more employees, then the large group health plan pays first, and Medicare pays second .
When two insurance which one is primary?
If you have two plans, your primary insurance is your main insurance. Except for company retirees on Medicare, the health insurance you receive through your employer is typically considered your primary health insurance plan.
Who qualifies for Medicaid?
To participate in Medicaid, federal law requires states to cover certain groups of individuals. Low-income families, qualified pregnant women and children, and individuals receiving Supplemental Security Income (SSI) are examples of mandatory eligibility groups (PDF, 177.87 KB).
Can you have Medicare and Medicaid?
Medicare-Medicaid Plans Medicare is working with some states and health plans to offer demonstration plans for certain people who have both Medicare and Medicaid and make it easier for them to get the services they need. They're called Medicare-Medicaid Plans.
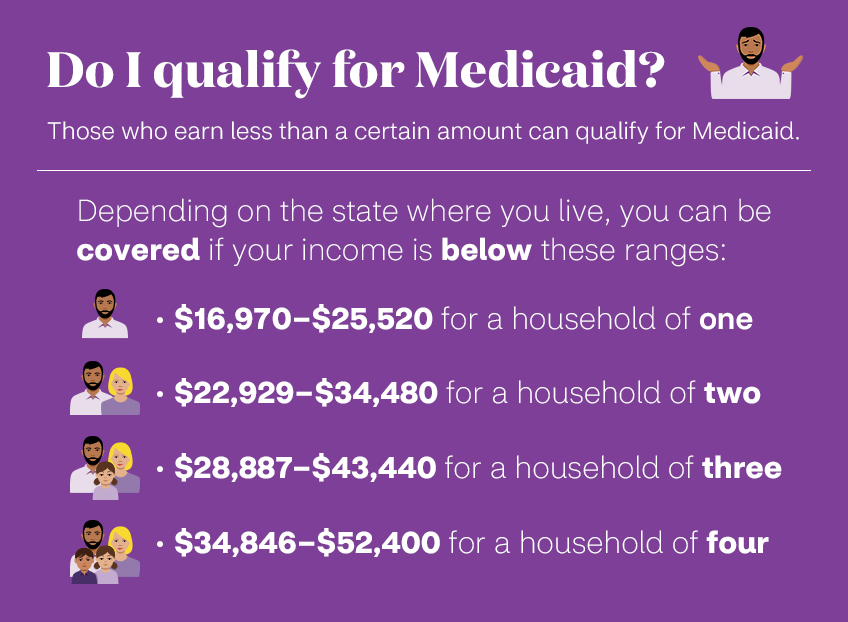
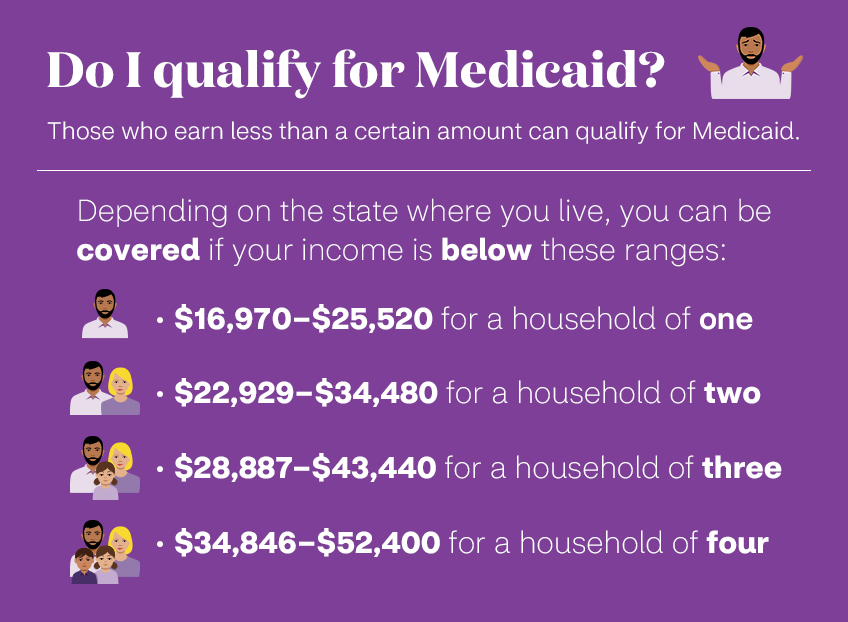
What is the highest income to qualify for Medicaid?
Federal Poverty Level thresholds to qualify for Medicaid The Federal Poverty Level is determined by the size of a family for the lower 48 states and the District of Columbia. For example, in 2022 it is $13,590 for a single adult person, $27,750 for a family of four and $46,630 for a family of eight.
Do they automatically send you a Medicare card?
You should automatically receive your Medicare card three months before your 65th birthday. You will automatically be enrolled in Medicare after 24 months and should receive your Medicare card in the 25th month.
How much Social Security will I get at the age of 65?
approximately $33,773 per yearIf you start collecting your benefits at age 65 you could receive approximately $33,773 per year or $2,814 per month. This is 44.7% of your final year's income of $75,629. This is only an estimate. Actual benefits depend on work history and the complete compensation rules used by Social Security.
Can I get Medicare Part B for free?
While Medicare Part A – which covers hospital care – is free for most enrollees, Part B – which covers doctor visits, diagnostics, and preventive care – charges participants a premium. Those premiums are a burden for many seniors, but here's how you can pay less for them.
How old do you have to be to qualify for medicare?
Citizens or legal residents residing in the U.S. for a minimum of 5 years immediately preceding application for Medicare. Applicants must also be at least 65 years old. For persons who are disabled or have been diagnosed with end-stage renal disease or Lou Gehrig’s disease (amyotrophic lateral sclerosis), there is no age requirement. Eligibility for Medicare is not income based. Therefore, there are no income and asset limits.
What is Medicare and Medicaid?
Differentiating Medicare and Medicaid. Persons who are eligible for both Medicare and Medicaid are called “dual eligibles”, or sometimes, Medicare-Medicaid enrollees. Since it can be easy to confuse the two terms, Medicare and Medicaid, it is important to differentiate between them. While Medicare is a federal health insurance program ...
How much does Medicare Part B cost?
For Medicare Part B (medical insurance), enrollees pay a monthly premium of $148.50 in addition to an annual deductible of $203. In order to enroll in a Medicare Advantage (MA) plan, one must be enrolled in Medicare Parts A and B. The monthly premium varies by plan, but is approximately $33 / month.
How to apply for medicaid?
How to Apply. To apply for Medicare, contact your local Social Security Administration (SSA) office. To apply for Medicaid, contact your state’s Medicaid agency. Learn about the long-term care Medicaid application process. Prior to applying, one may wish to take a non-binding Medicaid eligibility test.
Does Medicare cover out-of-pocket expenses?
Persons who are enrolled in both Medicaid and Medicare may receive greater healthcare coverage and have lower out-of-pocket costs. For Medicare covered expenses, such as medical and hospitalization, Medicare is always the first payer (primary payer). If Medicare does not cover the full cost, Medicaid (the secondary payer) will cover the remaining cost, given they are Medicaid covered expenses. Medicaid does cover some expenses that Medicare does not, such as personal care assistance in the home and community and long-term skilled nursing home care (Medicare limits nursing home care to 100 days). The one exception, as mentioned above, is that some Medicare Advantage plans cover the cost of some long term care services and supports. Medicaid, via Medicare Savings Programs, also helps to cover the costs of Medicare premiums, deductibles, and co-payments.
Does Medicaid cover nursing home care?
Medicaid also pays for nursing home care, and often limited personal care assistance in one’s home. While some states offer long-term care and supports in the home and community thorough their state Medicaid program, many states offer these supports via 1915 (c) Medicaid waivers.
Is Medicaid a federal program?
Eligibility requirements for Medicaid are not as straightforward as are the requirements for Medicare. This is because, as mentioned previously, Medicaid is a federal and state program. While the parameters of the program are federally set, each state can set their own rules within these guidelines. Even within the same state, there are a variety of pathways to Medicaid that have their own eligibility requirements.
What if I don't qualify for medicaid?
If you don't qualify for Medicaid, we'll tell you if you qualify for financial help to buy a Marketplace health plan instead. (But unless you qualify to enroll with a Special Enrollment Period, you'll have to wait until the next Open Enrollment Period.)
Can I buy a private health plan through the Marketplace?
You may be able to buy a private health plan through the Marketplace instead for the 2018 plan year in the fall. You may qualify for savings based on your income through a premium tax credit and savings on out-of-pocket costs. If you don't qualify for either Marketplace or Medicaid savings, you still have options. Learn more here.
Can I qualify for medicaid based on my income?
No matter your state, you may qualify for Medicaid based on your income, household size, disability, family status, and other factors. But if your state has expanded Medicaid coverage, you can qualify based on your income alone. Enter your household size and state.
How many people are covered by medicaid?
Medicaid also provides coverage to 4.8 million people with disabilities who are enrolled in Medicare.
Can you be covered by Medicare and Medicaid?
Individuals who are enrolled in both Medicaid and Medicare, by federal statute, can be covered for both optional and mandatory categories.
Can Medicare help with out of pocket medical expenses?
Medicare enrollees who have limited income and resources may get help paying for their premiums and out-of-pocket medical expenses from Medicaid (e.g. MSPs, QMBs, SLBs, and QIs).
What is Medicare insurance?
Medicare. Medicare is an insurance program. Medical bills are paid from trust funds which those covered have paid into. It serves people over 65 primarily, whatever their income; and serves younger disabled people and dialysis patients. Patients pay part of costs through deductibles for hospital and other costs.
Do you pay for medical expenses on medicaid?
Patients usually pay no part of costs for covered medical expenses. A small co-payment is sometimes required. Medicaid is a federal-state program. It varies from state to state. It is run by state and local governments within federal guidelines.
Is Medicare a federal program?
Small monthly premiums are required for non-hospital coverage. Medicare is a federal program. It is basically the same everywhere in the United States and is run by the Centers for Medicare & Medicaid Services, an agency of the federal government.
Recent Questions
How long does it take for Medicaid to begin once my mom is in the facility? This is now 5 weeks.
Popular Questions
How much can an elderly parent give as gifts without worrying about "look back" laws?
What is Medicaid for elderly parents?
By any name, this is government insurance for people who have very little money that covers , among other things, the cost of home care and nursing home care when a recipient can no longer care ...
How much can a spouse keep on Medicaid?
Under what’s known as the Community Spouse Resource Allowance, Medicaid will allow a spouse to keep the couple’s house, car, belongings, and, in some states, more than $100,000 in assets.
What to do if your parent wants to protect your assets?
If your parent wants to protect some assets, he should speak with a Medicaid planner, typically an elder law attorney, to sort it all out.
How long does it take to pay for nursing home care?
In other words, if someone gives away $60,000 and nursing home care costs $6,000 a month, he would have to pay for his own care for 10 months.
How early can you put your parents assets in an irrevocable trust?
But this has to be done very early in the game — five years early, to be specific.
Can Medicaid go after equity in home?
Medicaid eligibility and/or the state will then go after the equity in the home to recoup what’s been spent on health care. If an adult “child” lives in his parent’s home and cares for that parent for more than two years, some states allow the home to be transferred to the caregiver without penalty.
Is Medicaid a federal or state program?
Unlike Medicare, which is fully regulated by the federal government, Medicaid is a joint program of both federal and state governments. The federal government sets guidelines, and states establish their own rules and programs within these broad parameters. ( MORE: Find Out Qualifications for Medicaid Benefits)
What is an annual review of Medicare?
An annual review of your Medicare coverage can help you determine if your plan combination is right for your needs. For example, if you’re spending a considerable amount of money on prescription drugs, a Medicare Part D plan or a Medicare Advantage plan with prescription drug coverage may be something to consider.
What are the benefits of Medicare Advantage?
Most Medicare Advantage plans offer additional benefits not covered by Original Medicare, such as dental, vision and prescription drug coverage. Medicare Part D provides coverage for prescription medications, which is something not typically covered by Original Medicare.
How long does Medicare AEP last?
The Medicare AEP lasts from October 15 to December 7 every year. During this time, Medicare beneficiaries may do any of the following: Change from Original Medicare to a Medicare Advantage plan. Change from Medicare Advantage back to Original Medicare. Switch from one Medicare Advantage plan to another.
What is Medicare Part B?
Medicare Part B is medical insurance and provides coverage for outpatient appointments and durable medical equipment. Part B is optional, but is required for anyone wanting to enroll in Medicare Part C, Part D or Medicare Supplement Insurance. Part A and Part B are known together as “Original ...
Is Medicare Part A and Part B the same?
Part A and Part B are known together as “Original Medicare.”. Medicare Part C, also known as Medicare Advantage, provides all the same benefits as Medicare Part A and Part B combined into a single plan sold by a private insurance company.