What impact do you think did the establishment of Medicare and Medicaid have had on beneficiaries?
Medicare and Medicaid have greatly reduced the number of uninsured Americans and have become the standard bearers for quality and innovation in American health care. Fifty years later, no other program has changed the lives of Americans more than Medicare and Medicaid.
How do poor people pay for Medicare?
While eligibility for Medicare does not depend on income, lower-income Medicare enrollees qualify for help paying premiums, deductibles, and other cost sharing through Medicaid or the Medicare Low-Income Subsidy (LIS) program. In many cases, eligibility for that assistance is based on the federal poverty line.
What is the lowest income to qualify for Medicaid?
Federal Poverty Level thresholds to qualify for Medicaid The Federal Poverty Level is determined by the size of a family for the lower 48 states and the District of Columbia. For example, in 2022 it is $13,590 for a single adult person, $27,750 for a family of four and $46,630 for a family of eight.
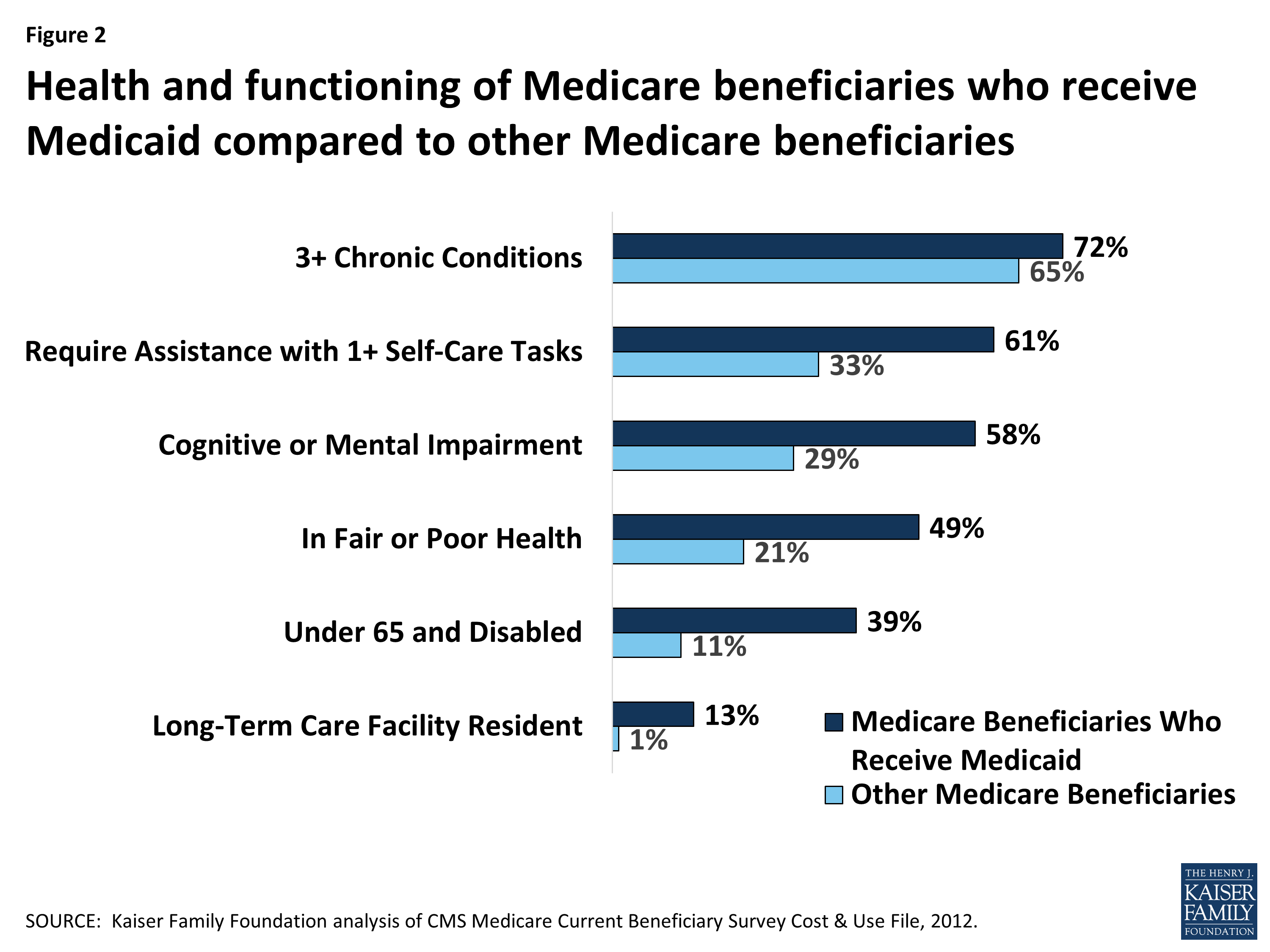
Who benefits the most from Medicaid?
Medicaid spending is concentrated on the elderly and people with disabilities. Seniors and people with disabilities make up 1 in 4 beneficiaries but account for almost two-thirds of Medicaid spending, reflecting high per enrollee costs for both acute and long-term care (Figure 9).
Which program helps low income individuals by requiring states?
Health Insurance Chapter 14, 15QuestionAnswerThis helps individuals whose assets are not low enough to qualify them for medicaid by requiring states to pay their medicare part A and B premiums, deductibles, and coinsurance amountsqualified medicare beneficiary program (QMBP)39 more rows
How do you pay for Medicare Part B if you are not collecting Social Security?
If you have Medicare Part B but you are not receiving Social Security or Railroad Retirement Board benefits yet, you will get a bill called a “Notice of Medicare Premium Payment Due” (CMS-500). You will need to make arrangements to pay this bill every month.
What are the disadvantages of Medicaid?
Disadvantages of Medicaid They will have a decreased financial ability to opt for elective treatments, and they may not be able to pay for top brand drugs or other medical aids. Another financial concern is that medical practices cannot charge a fee when Medicaid patients miss appointments.
Can you have Medicare and Medicaid at the same time?
Yes. A person can be eligible for both Medicaid and Medicare and receive benefits from both programs at the same time.
Can you have Medicare and Medicaid?
If you are eligible for both Medicare and Medicaid (dually eligible), you can have both. They will work together to provide you with health coverage and lower your costs.
Which state has highest income limit for Medicaid?
AlaskaThe state with the highest income limits for both a family of three and individuals is Washington, D.C. If you live in this area, a family of three can qualify for Medicaid if their income is at 221% of the FPL....Medicaid Income Limits by State 2022.StateAlaskaParents (Family of 3)138.00%Other Adults138.00%2022 Pop.720,76349 more columns
Which state is best for Medicaid?
Top 5 states on Medicaid eligibility, spending and qualityMassachusetts.Minnesota.California.Vermont.Rhode Island.
What is the difference between Medicare and Medicaid?
The difference between Medicaid and Medicare is that Medicaid is managed by states and is based on income. Medicare is managed by the federal government and is mainly based on age. But there are special circumstances, like certain disabilities, that may allow younger people to get Medicare.
What does SLMB cover?
SLMB benefits cover the cost of the monthly Medicare Part B premium. The standard Part B premium in 2021 is $148.50 per month and is required of all Medicare Part B beneficiaries.
How do you qualify for SLMB?
Each state Medicaid program has its own rules concerning qualification.
What other Medicare Savings Programs are there?
SLMB is just one of the available Medicare Savings Programs. Others include:
How do you apply for SLMB?
Contact your state Medicaid program for information and assistance with applying for the SLMB program.
Is there Medicaid assistance for Medicare Advantage beneficiaries?
Individuals who qualify for both Medicare and Medicaid are considered “dual eligible” and may qualify for a certain type of Medicare Advantage plan called a Special Needs Plan. And one particular type of Special Needs Plan is a Dual Eligible Special Needs Plan (D-SNP).
How Medicaid Works with Medicare
Many of the millions of Medicare enrollees in the United States are at least 65 years old; however, Medicare is also available to younger people with qualifying disabilities. You may also be eligible for Medicaid if you meet income and resource limit requirements.
2021 Dual Eligible Standards
Medicare is available if you’re at least 65 years old or have some disability, such as amyotrophic lateral sclerosis, that qualifies you for Social Security Disability Income (SSDI) benefits. To receive premium-free Part A coverage, you must have worked and paid Medicare taxes for a minimum number of quarters. You must also be a U.S.
Qualifying and Applying for Medicare and Medicaid
The Medicare eligibility requirements can be confusing, especially for applicants under 65 who get Medicare coverage for a qualifying disability. Area Agencies on Aging have trained counselors on hand to answer questions about Medicare and help current Medicare beneficiaries determine if they might be dually eligible.
Medicaid Costs
As long as they cover mandatory benefits required by CMS, states can implement cost-sharing arrangements as part of their Medicaid plans. CMS caps out-of-pocket costs, but state Medicaid programs are also allowed to charge a premium for enrollees in the following groups:
Medicaid Benefits
The federal government and individual states work together to ensure that individuals with low incomes have access to basic health coverage under the Medicaid program.
How to Apply
Contact your local Medicaid office to ask questions about program requirements and request a paper application. In many states, it’s also possible to apply for Medicaid coverage on HealthCare.gov. If you aren’t eligible for Medicaid, it may be possible to get a tax credit to help pay for a plan from the Health Insurance Marketplace.
Additional Resources
State Health Insurance Assistance Programs: Connect with an experienced counselor who can offer unbiased advice on Medicare and Medicaid options.
What is the benefit of Medicare for low income people?
Of the 54 million people with Medicare, a staggering 25% have annual incomes below $14,400. For these people living in retirement, or coping with a disability in poverty, Medicare coverage offers a lifeline, a chance to get needed health care. That precious red white and blue Medicare card means ...
Does Medicare work for people in poverty?
Fortunately, the Medicare lifeline does work for many people in poverty, but only because safety net programs work together with Medicare to plug coverage gaps and make the Medicare benefit affordable. The Medicaid program covers Medicare premiums, deductibles and co-payments.
How many people are covered by medicaid?
Medicaid also provides coverage to 4.8 million people with disabilities who are enrolled in Medicare.
Can you be covered by Medicare and Medicaid?
Individuals who are enrolled in both Medicaid and Medicare, by federal statute, can be covered for both optional and mandatory categories.
Can Medicare help with out of pocket medical expenses?
Medicare enrollees who have limited income and resources may get help paying for their premiums and out-of-pocket medical expenses from Medicaid (e.g. MSPs, QMBs, SLBs, and QIs).