How do I reenroll in Medicare Part B?
If you’ve disenrolled from or cancelled your Medicare Part B coverage, you may have to pay a costly late enrollment penalty to reenroll. This is especially true if you have a gap in coverage. If you’re looking to reenroll in Medicare Part B, follow these steps: Go to the Social Security Administration website. Complete the application.
What happens if you don’t enroll in Medicare Part B?
You could face a late-enrollment penalty if you miss it. For each full year that you should have been enrolled but were not, you’ll pay 10% of the monthly Part B base premium.
Can I enroll in Medicare Part B If I have ALS?
You have end stage renal disease (ESRD). You have amyotrophic lateral sclerosis (ALS). Though you’re unable to use the plan benefits until the day you turn 65 years old, you’re eligible to enroll: You’re also qualified to enroll in Medicare Part B if you have a disability and are receiving Social Security disability payments.
What happens to low-performing Medicare Advantage and Part D plans?
Low-performing Medicare Advantage or Medicare Part D plans may be discontinued by the Centers for Medicare and Medicaid Services (CMS). A private insurer may decide to restructure their plan offerings and drop a particular plan from their selection. An insurance company could go insolvent and shut their doors altogether.
Can a person lose their Medicare coverage?
In most cases, you won't lose your Medicare eligibility. But if you move out of the country, or if you qualify for Medicare by disability or health problem, you could lose your Medicare eligibility.
What are two major problems with respect to the future of Medicare?
Financing care for future generations is perhaps the greatest challenge facing Medicare, due to sustained increases in health care costs, the aging of the U.S. population, and the declining ratio of workers to beneficiaries.
At what income do you lose Medicare?
an individual monthly income of $4,379 or less. an individual resources limit of $4,000. a married couple monthly income of $5,892 or less. a married couple resources limit of $6,000.
Is Medicare broke or not?
Medicare is running out of money. According to the latest projections from the Congressional Budget Office (CBO), the program's Part A hospital insurance trust fund will be exhausted in 2024. That's just three years away, before the end of President Joe Biden's first term.
What are the challenges of Medicare?
Medicare's challenges are not solely financial. Medicare beneficiaries are a diverse group with diverse health care needs, and certain beneficiary populations—such as those with a disabilities or multiple chronic conditions—are particularly vulnerable to having high health care needs.
What happens when Medicare runs out in 2026?
The trust fund for Medicare Part A will be able to pay full benefits until 2026 before reserves will be depleted. That's the same year as predicted in 2020, according to a summary of the trustees 2021 report, which was released on Tuesday.
Why would my Medicare be Cancelled?
Depending on the type of Medicare plan you are enrolled in, you could potentially lose your benefits for a number of reasons, such as: You no longer have a qualifying disability. You fail to pay your plan premiums. You move outside your plan's coverage area.
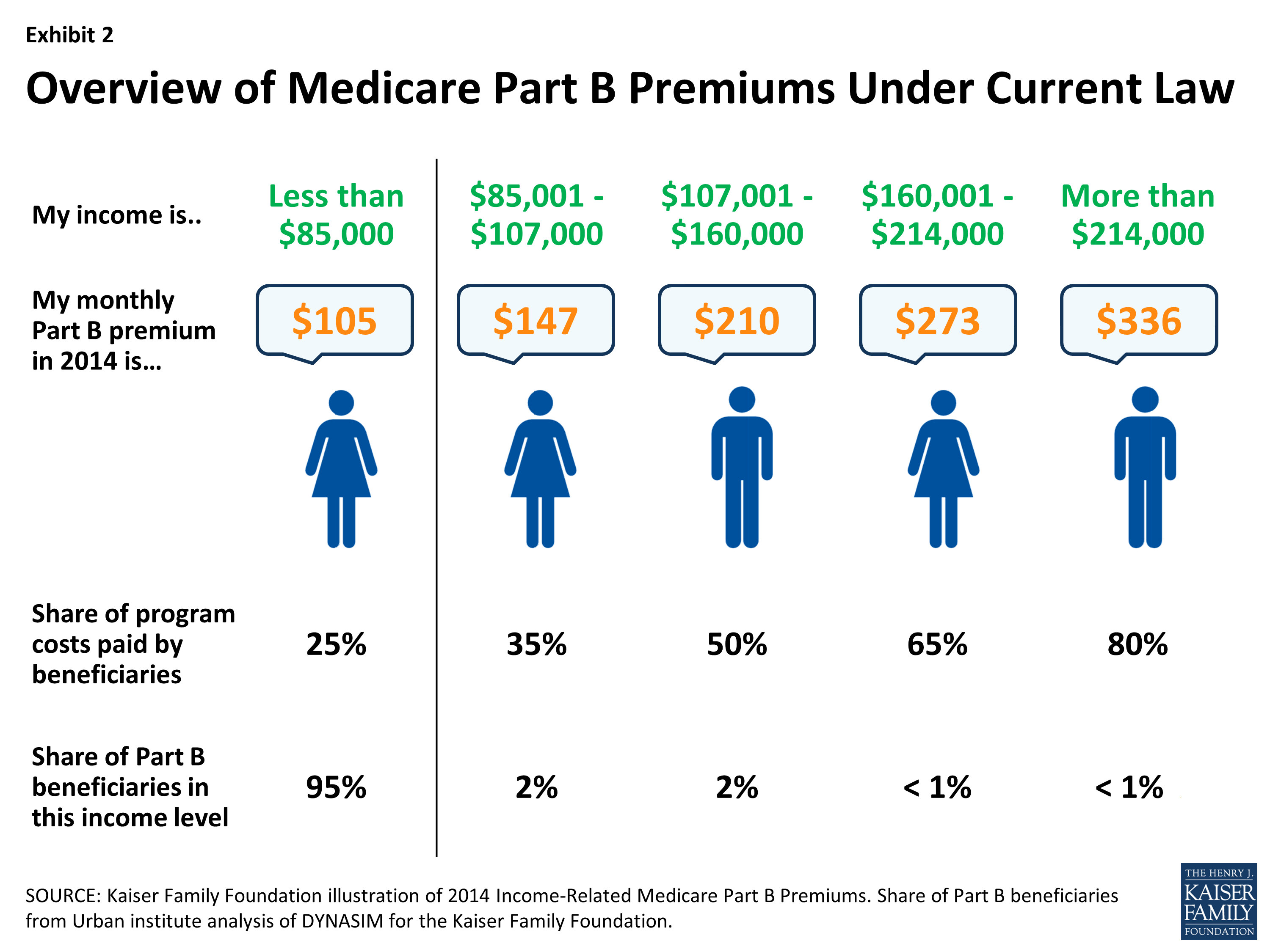
Is Medicare based on your income?
Medicare premiums are based on your modified adjusted gross income, or MAGI. That's your total adjusted gross income plus tax-exempt interest, as gleaned from the most recent tax data Social Security has from the IRS.
What income level triggers higher Medicare premiums?
If you file your taxes as “married, filing jointly” and your MAGI is greater than $182,000, you'll pay higher premiums for your Part B and Medicare prescription drug coverage. If you file your taxes using a different status, and your MAGI is greater than $91,000, you'll pay higher premiums.
What would happen if Medicare ended?
Payroll taxes would fall 10 percent, wages would go up 11 percent and output per capita would jump 14.5 percent. Capital per capita would soar nearly 38 percent as consumers accumulated more assets, an almost ninefold increase compared to eliminating Medicare alone.
What is the future for Medicare?
After a 9 percent increase from 2021 to 2022, enrollment in the Medicare Advantage (MA) program is expected to surpass 50 percent of the eligible Medicare population within the next year. At its current rate of growth, MA is on track to reach 69 percent of the Medicare population by the end of 2030.
What happens if you move to a new address with Medicare Advantage?
If you relocate to a new address with Medicare Advantage or Part D plan you could lose your coverage. Private insurance companies sell these plans, which are specific to certain areas.
How long does it take to get Medicare?
Medicare benefits start on the first day of the month of your 65th birthday if you’re getting Social Security. It could take up to three months if you apply yourself, or longer if you apply using the General Enrollment Period.
How Long Do Medicare Benefits Last?
For those under 65 who are eligible due to disability, Medicare benefits can last anywhere from one year to the rest of your life. The extent of your coverage depends on your situation. However, for those who age into Medicare at 65, benefits last a lifetime.
How long can you get Medicare if you stop receiving SSDI?
SSDI is a federal program that assists Americans with disabilities. Individuals who stop receiving SSDI benefits can continue Medicare coverage for 93 months. However, they can only get 93 months of Medicare if they’ve completed their nine-month work period.
How long can you get Medicare Part A?
Additionally, they become eligible for premium-free Medicare Part A for eight and a half years if they finish the nine-month period and their trial work period. In the meantime, they can also continue paying for your Part B coverage.
Can you lie about Medigap?
When applying for a Medigap, you should never lie or attempt to leave out the truth. Doing so can lead to the cancelation of your coverage. You’ll need to answer health questions and undergo the medical underwriting process if you apply outside of your Medigap Open Enrollment Period. In this situation, it’s crucial to be as honest as possible about your health.
Can you lose supplemental Medicare?
Losing supplemental Medicare coverage is different from becoming dis-enrolled from Original Medicare. The following are reasons that can disqualify you from your current supplemental coverage.
What happens if you lose your Medicare?
If you lose your current coverage, you must sign up for Medicare within a certain time frame. If you don’t, you’ ll incur penalties that may last your whole life.
What happens if you don't wait for Medicare open enrollment?
If this happens, don’t wait for the next Medicare open enrollment period, otherwise you may have a lapse in coverage and owe penalty fees.
How much is Medicare Part B in 2021?
Medicare Part B covers outpatient medical costs and comes with a monthly premium for all Medicare beneficiaries. The standard premium is $148.50 per month in 2021, but this rate could be higher based on your income. You can also defer Part B coverage. However, if you defer Medicare Part B coverage, you may receive significant financial penalties ...
How long do you have to enroll in Medicare if you have lost your current plan?
No matter your reasons for deferring, you must enroll in Medicare within 8 months of losing your current coverage.
How long do you have to work to get Medicare Part A?
Medicare Part A covers hospital expenses. If you or your spouse worked for at least 10 years (40 quarters), you will most likely be eligible for premium-free Part A when you turn 65 years old. You can defer Medicare Part A.
How many employees can you defer Medicare?
To defer Medicare, you must have qualifying health insurance, such as through a large group plan that covers 20 or more employees.
Is Medicare mandatory?
Medicare isn’t mandatory. You can defer Medicare coverage if you feel it’s in your best interest to do so. Keep in mind, though, that most people who are eligible for Medicare do benefit from enrolling in both Part A and Part B ( original Medicare) during their initial enrollment period.
How to qualify for Medicare premium free?
To be eligible for premium-free Part A, an individual must be entitled to receive Medicare based on their own earnings or those of a spouse, parent, or child. To receive premium-free Part A, the worker must have a specified number of quarters of coverage (QCs) and file an application for Social Security or Railroad Retirement Board (RRB) benefits. The exact number of QCs required is dependent on whether the person is filing for Part A on the basis of age, disability, or End Stage Renal Disease (ESRD). QCs are earned through payment of payroll taxes under the Federal Insurance Contributions Act (FICA) during the person's working years. Most individuals pay the full FICA tax so the QCs they earn can be used to meet the requirements for both monthly Social Security benefits and premium-free Part A.
What is the income related monthly adjustment amount for Medicare?
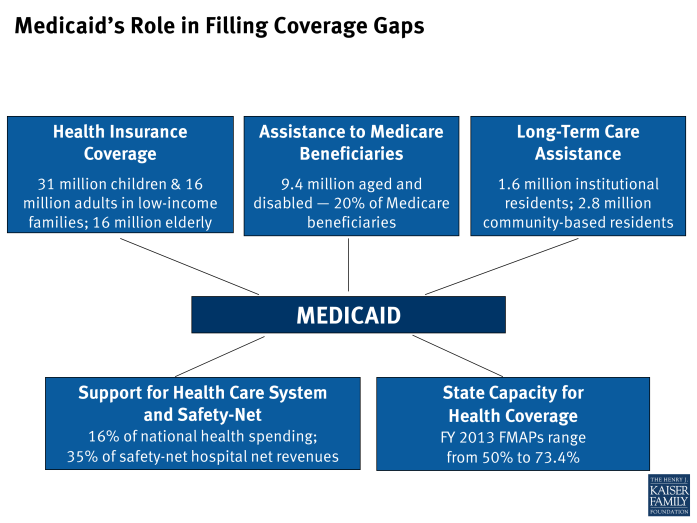
Individuals with income greater than $85,000 and married couples with income greater than $170,000 must pay a higher premium for Part B and an extra amount for Part D coverage in addition to their Part D plan premium. This additional amount is called income-related monthly adjustment amount. Less than 5 percent of people with Medicare are affected, so most people will not pay a higher premium.
How long do you have to be on Medicare if you are disabled?
Disabled individuals are automatically enrolled in Medicare Part A and Part B after they have received disability benefits from Social Security for 24 months. NOTE: In most cases, if someone does not enroll in Part B or premium Part A when first eligible, they will have to pay a late enrollment penalty.
How long does it take to get Medicare if you are 65?
For someone under age 65 who becomes entitled to Medicare based on disability, entitlement begins with the 25 th month of disability benefit entitlement.
How long does Medicare take to pay for disability?
A person who is entitled to monthly Social Security or Railroad Retirement Board (RRB) benefits on the basis of disability is automatically entitled to Part A after receiving disability benefits for 24 months.
When do you have to apply for Medicare if you are already on Social Security?
Individuals already receiving Social Security or RRB benefits at least 4 months before being eligible for Medicare and residing in the United States (except residents of Puerto Rico) are automatically enrolled in both premium-free Part A and Part B. People living in Puerto Rico who are eligible for automatic enrollment are only enrolled in premium-free Part A.
When does Medicare start if you have an IEP?
Coverage begins based on when you enroll during the IEP. If a person enrolls in the first 3 months of the IEP, coverage begins the first month the person is eligible for Medicare. If a person enrolls in any other month of the IEP, coverage will be delayed. Disabled individuals are automatically enrolled in Medicare Part A and Part B after they have received disability benefits from Social Security for 24 months.
What About Medicare Part B?
Medicare Part B DOES have a premium ( $148.50 for 2021, an increase of $3.90 from $144.60 in 2020 ). 1 Therefore, choosing whether to delay enrollment in Part B is the more pertinent question for most people. Medicare does have late enrollment penalties that apply if you are not currently covered by a credible group health plan connected to current employment, so you should make yourself aware of those penalties before making this decision.
Is there a premium for Medicare Part A?
For most people, there is no premium associated with Medicare Part A. People who are receiving Social Security benefits or are on Medicare disability will be enrolled in Part A automatically at age 65. For most everyone else, because there is no premium for this coverage, enrolling in Part A may be beneficial. ...
When is Medicare open enrollment?
Medicare open enrollment period — October 15 through December 7. During this time, you can switch from a Medicare Advantage (Part C) plan back to original Medicare. You can also change Part C plans or add, remove, or change a Medicare Part D (prescription drug) plan. Special enrollment period — 8 months following a qualifying event.
How long do you have to pay back Medicare Part B?
If you were disenrolled from your Medicare part B plan for missing premium payments, you have 30 days from the official termination date to repay what’s due. If accepted, your coverage will continue. If you don’t pay back the premiums within the allotted time, you’ll have to reenroll during the next general enrollment period, ...
What happens if you cancel Medicare Part B?
If you’ve disenrolled from or cancelled your Medicare Part B coverage, you may have to pay a costly late enrollment penalty to reenroll. This is especially true if you have a gap in coverage. If you’re looking to reenroll in Medicare Part B, follow these steps: Go to the Social Security Administration website. Complete the application.
How long does it take to reenroll in Medicare?
Special enrollment period — 8 months following a qualifying event. If you qualify, you may be granted this 8-month window to reenroll in original Medicare or change your Medicare coverage after a significant life event, such as a divorce or move. Read on to learn more about how to reenroll in Medicare Part B and what it covers.
When do you have to reenroll in Medicare if you don't pay back?
If you don’t pay back the premiums within the allotted time, you’ll have to reenroll during the next general enrollment period, which runs from January 1 through March 31 each year. You can also ask for reinstatement under the Medicare Good Cause policy.
How old do you have to be to get medicare?
People 65 years old or over qualify for Medicare coverage.
Can you pay premiums on a late enrollment plan?
The caveat to this enrollment period is that you may have to pay higher premiums on the plan for late enrollment.