If you're asking whether Medicare would pay for home-health care ("a sitter") the answer is yes. The care must be provided by a person or agency that is accredited and contracted to receive Medicare payments.
How much does someone pay for a sitter?
Pet sitter rates vary widely, depending on a number of factors, including:
- Their experience
- Their training
- Where you live
- Whether you are in an urban or rural setting
- How many pets you have
- The cost of living
Does Medicare pay for senior bed rails?
Unfortunately, Medicare does not cover the cost of detachable bed rails that are meant to be used on conventional beds. However, Medicare recipients may be eligible for a hospital bed which includes attachable and adjustable side rails. Click to see full answer. Similarly one may ask, what kind of medical equipment does Medicare cover?
Does Medicare help pay for caregiver services?
Medicare typically doesn’t pay for in-home caregivers for personal care or housekeeping if that’s the only care you need. Medicare may pay for short-term caregivers if you also need medical care to recover from surgery, an illness, or an injury.
Does Medicare pay for home IV therapy?
When infusions are done in the hospital or in a skilled nursing facility, Medicare picks up the payment for infusion therapy. However, it is has not extended that benefit to home IV therapy, even though the costs are much less than what is entailed when receiving IV therapy in a hospital or nursing home.
Does Medicare pay for a family member to be a caregiver?
Medicare (government health insurance for people age 65 and older) does not pay for long-term care services, such as in-home care and adult day services, whether or not such services are provided by a direct care worker or a family member.
Does Medicare cover light housekeeping?
Personal home care services (assistance with activities of daily living) or homemaker services (e.g. light housekeeping and laundry) will only be covered if they are part of the skilled services detailed in the care plan. Medicare does not cover around-the-clock home care of any kind or meals delivered to the home.
How Much Does Medicare pay for home health care per hour?
Medicare will cover 100% of the costs for medically necessary home health care provided for less than eight hours a day and a total of 28 hours per week. The average cost of home health care as of 2019 was $21 per hour.
What will Medicare not pay for?
Generally, Original Medicare does not cover dental work and routine vision or hearing care. Original Medicare won't pay for routine dental care, visits, cleanings, fillings dentures or most tooth extractions. The same holds true for routine vision checks. Eyeglasses and contact lenses aren't generally covered.
Will Medicare cover skilled nursing care?
Medicare will pay for what’s considered intermittent nursing services, meaning that care is provided either fewer than seven days a week, or daily...
Will Medicare cover physical, occupational, and speech therapy?
Medicare will pay for physical therapy when it’s required to help patients regain movement or strength following an injury or illness. Similarly, i...
Does Medicare cover durable medical equipment?
Medicare will cover the cost of medically necessary equipment prescribed by a doctor for in-home use. This includes items such as canes or walkers,...
Does Medicare cover medical social services?
Medicare will pay for medically prescribed services that allow patients to cope with the emotional aftermath of an injury or illness. These may inc...
Who’s eligible for in-home care through Medicare?
Medicare enrollees are eligible for in-home care under Medicare Parts A and B provided the following conditions are met: The patient is under the c...
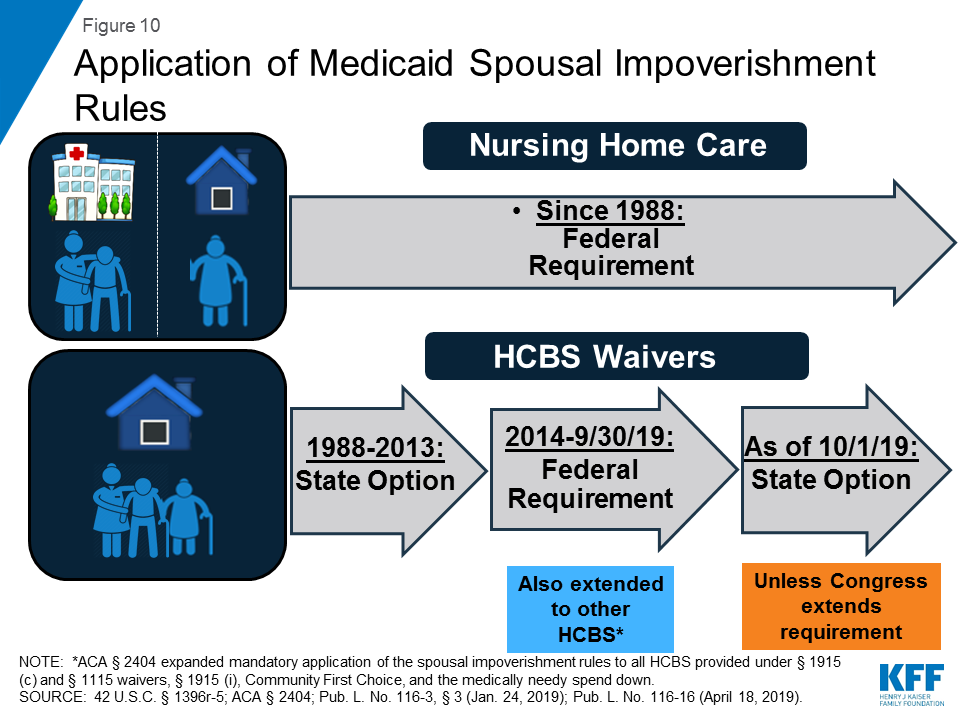
Will Medicaid pay for long-term care services?
Many Medicare enrollees are qualify for Medicaid due to their limited incomes and assets. Unlike Medicare, Medicaid covers both nursing home care a...
What is the Medicare Part B copayment?
For Medicare Part B, this comes to 20%. Copayment: This is a fixed dollar amount that an insured person pays when receiving certain treatments. For Medicare, this usually applies to prescription drugs.
What is a local Medicaid office?
A local Medicaid office can offer advice on eligibility and answer questions about enrollment. Medicare Savings Programs (MSP): Medicare Savings Programs are plans for those with limited resources. How the plans work can differ by state, but all assist with paying Medicare out-of-pocket costs.
What is a Medigap plan?
Medigap: Private insurance companies administer Medicare supplement insurance, or Medigap plans, to help to pay Medicare parts A and B copayments, coinsurance, and deductibles. Medigap plans K and L have an out-of-pocket limit. Once someone’s costs reach this limit, the plan pays 100% of Part B services, which could lower ...
Can you get medicaid if you have limited income?
Medicaid: Individuals qualify for Medicaid if they have limited resources and income or a disability. The rules can differ by state. Medicaid may help with costs that Medicare does not cover. The Medicaid Self-Directed Care Program allows people to hire family members to care for them.
Does Medicare cover medical supplies?
Medical supplies. Help with caregiver cost. Summary. Original Medicare only covers treatment by certain types of caregivers. Rules apply depending on the kind of care a person receives and the services a caregiver provides.
Does Medicare pay for home care?
Medicare does not pay for caregivers that provide the following: 24-hour care at home. meal delivery. homemaker services when this is the only service needed. supervision, or personal care, when this is the only service required.
Can you be homebound for Medicare?
the care delivered is through a written plan that the doctor regularly reviews. Although Medicare stipulates that a person must be homebound to receive coverage, they may leave home for short periods to attend doctor visits or for non-medical reasons, such as religious services.
How long does Medicare pay for custodial care?
Medicare will sometimes pay for short-term custodial care (100 days or less) if it’s needed in conjunction with actual in-home medical care prescribed by a doctor.
How long does Medicare pay for intermittent nursing?
Medicare will pay for what’s considered intermittent nursing services, meaning that care is provided either fewer than seven days a week, or daily for less than eight hours a day, for up to 21 days. Sometimes, Medicare will extend this window if a doctor can provide a precise estimate on when that care will end.
How many hours does Medicare pay for a week?
The maximum amount of weekly care Medicare will pay for is usually 28 hours, though in some circumstances, it will pay for up to 35. But it won’t cover 24-hour-a-day care.
What is skilled nursing?
Skilled nursing services are generally required to treat an illness or assist in the recovery of an injury. As the name implies, those who provide this care are licensed to administer medical treatment such as injections, catheter changes, wound dressings, and tube feedings.
Does Medicare cover social services?
Does Medicare cover medical social services? Medicare will pay for medically prescribed services that allow patients to cope with the emotional aftermath of an injury or illness. These may include in-home counseling from a licensed therapist or social worker.
Does Medicaid have a higher income limit?
Due to the high cost of long-term care, many states have higher Medicaid income limits for long-term care benefits than for other Medicaid coverage. However, Medicaid’s asset limits usually require you to “spend-down” resources before becoming eligible.
Is skilled nursing part time?
The need for skilled nursing is only part-time or intermittent. The home health agency used to provide care is approved by Medicare. Additionally, other than durable medical care, patients usually don’t pay anything for in-home care.
What services does Medicare cover for long term care?
Long-term care policies may also cover homemaker support services, such as meal preparation, laundry, light housekeeping and supervised intake of medications . Family Caregiver Support. Family caregivers are vital to the health and well-being of many Medicare recipients.
Do you have to be Medicare certified to be a home health agency?
The home health agency servicing you must be Medicare-certified, meaning they are approved by Medicare and accept assignment . If Medicare approves the claim for home health services, the authorized fees may be covered. Custodial Care for Day-to-Day Living.
Does Medicare cover hospital stays?
Some Medicare recipients are fortunate enough to have family members care for them and want to know if Medicare can help. Original Medicare is structured to cover costs incurred during hospital stays (Part A) and medical office visits (Part B).
What is Medicare Part A?
Medicare Part A (Hospital Insurance) and/or Part B (Medical Insurance) will help cover the costs of in-home health services if you are being treated by a doctor who creates a plan of care and reviews it regularly.
How many hours of skilled nursing per week?
Your doctor must certify that you require one of these services: Intermittent skilled nursing care, defined by Medicare as less than 7 days per week or less than 8 hours each day over a period of 21 days or less. Physical therapy, speech language pathology, or occupational therapy.
Is home health care the best?
Home health care may be the best solution to your needs. Home health services can be just as effective as treatment you would receive in a hospital or skilled nursing facility and may be less expensive. The wide range of services can include: Coordination of care with your medical providers. Monitoring serious illness.
Is home health insurance covered by Medicare?
When you are recovering from an illness or injury, your own home may provide the best environment to help you heal. If your doctor recommends it and you meet the criteria, your in-home health services may be covered by your Medicare insurance. Home health care may be the best solution to your needs.