If you recently got a welcome packet saying you automatically got Medicare Part A and Part B, follow the instructions in your welcome packet, and send your Medicare card back. If you keep the card, you agree to keep Part B, and you’ll start paying the monthly Part B premium.
Does Medicaid replace Medicare Part B?
To drop Part B (or Part A if you have to pay a premium for it), you usually need to send your request in writing and include your signature. Contact Social Security. If you recently got a welcome packet saying you automatically got Medicare Part A and Part B, follow the instructions in your welcome packet, and send your Medicare card back.
What is the current deductible for Medicare Part B?
for Part B when you’re first eligible. This amount can change every year. You can find up-to-date premium amounts on Medicare.gov. Important: In most cases, if you don’t sign up for Part B when you’re first eligible, you’ll have to pay a late enrollment penalty for as long as you have Part B. Also, you may have to wait until the
What is the current cost of Medicare Part B?
To be eligible for premium Part A, an individual must be age 65 or older and be enrolled in Part B. Enrollment in premium Part A and Part B can only happen at certain times. (The section titled Enrollment Periods and When Coverage Begins explains the times when someone can enroll). More Information on Enrolling in Part A
Does everyone pay the same for Medicare Part B?
Nov 24, 2021 · If you have questions, please contact Social Security at 1-800-772-1213 (TTY 1-800-325-0778). Note: When completing the forms CMS-40B and CMS-L564: State “I want Part B coverage to begin (MM/YY)” in the remarks section of the CMS-40B form or online application. If your employer is unable to complete Section B, please complete that portion ...

Can Medicare Part B be added at any time?
You can sign up for Medicare Part B at any time that you have coverage through current or active employment. Or you can sign up for Medicare during the eight-month Special Enrollment Period that starts when your employer or union group coverage ends or you stop working (whichever happens first).
Can you discontinue Medicare Part A?
To cancel Medicare Part A, fill out CMS form 1763 and return it to your local Social Security office.Jan 20, 2022
How do I opt into Medicare Part B?
Most people get Medicare Part B (Medical Insurance) when they turn 65....There are 3 ways you can sign up:Fill out a short form, and send it to your local Social Security office.Call Social Security at 1-800-772-1213. TTY users can call 1-800-325-0778.Contact your local Social Security office.Feb 22, 2021
Is it hard to switch Medicare plans?
The good news is that changing Medicare Advantage Plans is easy: Simply join a new plan and you'll be automatically disenrolled from your old plan. The bad news is there are only certain times of the year when you can change your Medicare Advantage Plan.Jan 15, 2022
Can you opt out of Medicare Part B?
A. Yes, you can opt out of Part B. (But make sure that your new employer insurance is “primary” to Medicare. If it's “secondary” — perhaps because the employer has fewer than 20 employees — you may still need Part B.)
Can I opt out of Medicare Part B at any time?
You can voluntarily terminate your Medicare Part B (medical insurance). However, since this is a serious decision, you may need to have a personal interview. A Social Security representative will help you complete Form CMS 1763.Nov 24, 2021
How long does it take to get Medicare Part B after?
Most Medicare provider number applications are taking up to 12 calendar days to process from the date we get your application. Some applications may take longer if they need to be assessed by the Department of Health. We assess your application to see if you're eligible to access Medicare benefits.Dec 10, 2021
What happens if I don't want Medicare Part B?
If you didn't get Part B when you're first eligible, your monthly premium may go up 10% for each 12-month period you could've had Part B, but didn't sign up. In most cases, you'll have to pay this penalty each time you pay your premiums, for as long as you have Part B.
What happens if I cancel Medicare Part B?
Canceling Part B because you were automatically enrolled But beware: if you opt out of Part B without having creditable coverage—that is, employer-sponsored health insurance from your current job that's as good or better than Medicare—you could face late-enrollment penalties (LEPs) down the line.Jun 5, 2020
Can you switch to Medicare at any time?
Can I make that change during the Medicare Open Enrollment period? Yes, you can elect to switch to traditional Medicare from your Medicare Advantage plan during the Medicare Open Enrollment period, which runs from October 15 to December 7 each year.
Can you switch Medicare Supplement plans anytime?
You can change your Medicare Supplement Plan anytime, just be aware that you might have to answer medical questions if your outside your Open Enrollment Period.
Why do doctors not like Medicare Advantage plans?
If they don't say under budget, they end up losing money. Meaning, you may not receive the full extent of care. Thus, many doctors will likely tell you they do not like Medicare Advantage plans because the private insurance companies make it difficult for them to get paid for the services they provide.
What is MEC in Medicare?
Medicare and Minimum Essential Coverage (MEC) Medicare Part A counts as minimum essential coverage and satisfies the law that requires people to have health coverage. For additional information about minimum essential coverage (MEC) for people with Medicare, go to our Medicare & Marketplace page.
How long does it take to get Medicare if you are 65?
For someone under age 65 who becomes entitled to Medicare based on disability, entitlement begins with the 25 th month of disability benefit entitlement.
How long do you have to be on Medicare if you are disabled?
Disabled individuals are automatically enrolled in Medicare Part A and Part B after they have received disability benefits from Social Security for 24 months. NOTE: In most cases, if someone does not enroll in Part B or premium Part A when first eligible, they will have to pay a late enrollment penalty.
What age do you have to be to get a Social Security card?
Understanding the Rules for People Age 65 or Older. To be eligible for premium-free Part A on the basis of age: A person must be age 65 or older; and. Be eligible for monthly Social Security or Railroad Retirement Board (RRB) cash benefits.
How long does Part A coverage last?
If the application is filed more than 6 months after turning age 65, Part A coverage will be retroactive for 6 months. NOTE: For an individual whose 65th birthday is on the first day of the month, Part A coverage begins on the first day of the month preceding their birth month.
When do you get Part A?
An individual who is receiving monthly Social Security or RRB benefits at least 4 months prior to turning age 65 does not need to file a separate application to become entitled to premium-free Part A. In this case, the individual will get Part A automatically at age 65.
Do you have to pay Part A and Part B?
Also enroll in or already have Part B. To keep premium Part A, the person must continue to pay all monthly premiums and stay enrolled in Part B. This means that the person must pay both the premiums for Part B and premium Part A timely to keep this coverage. Premium Part A coverage begins prospectively, based on the enrollment period ...
What is the individual health insurance marketplace?
NOTE: The Individual Health Insurance Marketplace is a place where people can go to compare and enroll in health insurance. In some states the Marketplace is run by the state and in other states it is run by the federal government. The Health Insurance Marketplace was set up through the Affordable Care Act, also known as Obamacare.
When do you get Part A and Part B?
You will automatically get Part A and Part B starting the first day of the month you turn 65. (If your birthday is on the first day of the month, Part A and Part B will start the first day of the prior month.)
Do you have to pay a penalty if you don't get Part A?
NOTE: If you don’t get Part A and Part B when you are first eligible, you may have to pay a lifetime late enrollment penalty. However, you may not pay a penalty if you delay Part A and Part B because you have coverage based on your (or your spouse’s) current employment.
What happens if you don't get Part B?
NOTE: If you don’t get Part B when you are first eligible, you may have to pay a lifetime late enrollment penalty. However, you may not pay a penalty if you delay Part B because you have coverage based on your (or your spouse’s) current employment.
What is Medicare Part B?
Part B – Costs. Premium. Medicare Part B has a monthly insurance premium that is based on when you enroll and your annual household income. This premium is commonly paid through Social Security withholdings.
How long does Medicare Part A last?
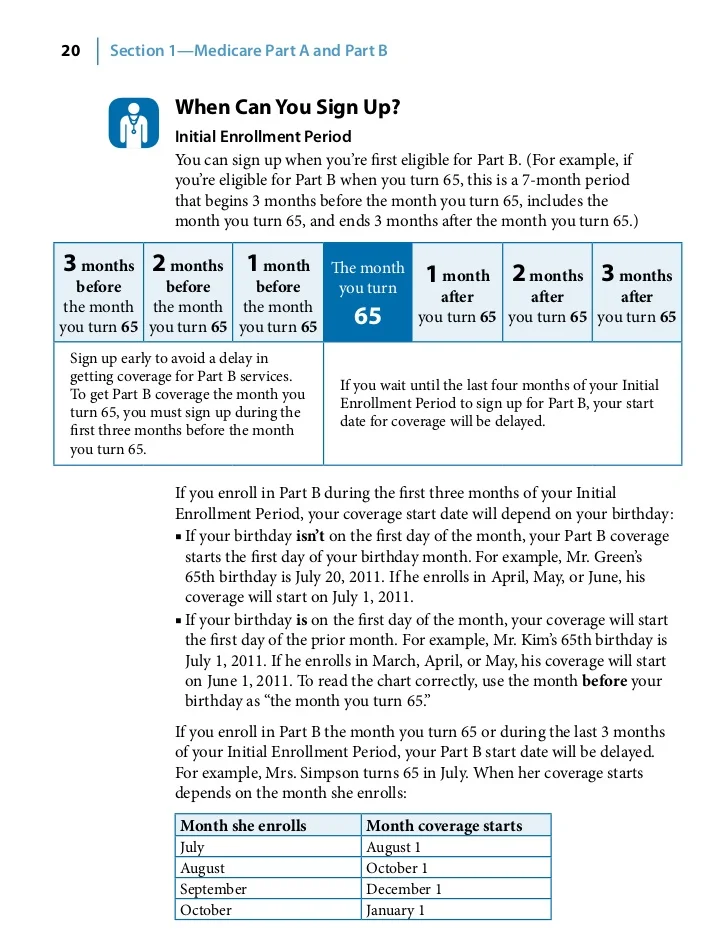
Title. When to Enroll. Description. When you are first eligible, your Initial Enrollment Period for Medicare Part A and Part B lasts seven months and starts when you qualify for Medicare, either based on your age or an eligible disability.
Is there a premium for Medicare Part A?
Premium. There is no insurance premium for Part A if you or your spouse contributed to Social Security for at least 10 years. Otherwise, an option to buy Medicare Part A is available. Deductible.
What is open enrollment period for Medicare?
The Medicare Open Enrollment Period provides an annual opportunity to review, and if necessary, change your Medicare coverage. Below are some examples of changes that you can make during Open Enrollment:
What is a copay?
Copays. A copayment or cost sharing may apply to specific services, such as those received in an outpatient hospital setting. Coinsurance. You pay 20 percent for some medical services, such as doctor services, outpatient therapy and durable medical equipment.
What is Medicare Part A?
Medicare Part A is hospital insurance. It may cover your care in certain situations, such as: You’re admitted to a hospital or mental hospital as an inpatient. You’re admitted to a skilled nursing facility and meet certain conditions. You qualify for hospice care.
How much does Medicare pay in 2019?
On the other hand, most people do pay a monthly premium for Medicare Part B. The standard premium in 2019 is $135.50, but you may pay more if your income is above a certain level. If you have a low income or no income, in some cases Medicaid might pay your Part B premium.
Can you get hospice care with Medicare?
You qualify for hospice care. Your doctor orders home health care for you and you meet the Medicare criteria. Medicare Part A may cover part-time home health care for a limited time. Even when Medicare Part A covers your care: You may have to pay a deductible amount and/or coinsurance or copayment.
How many Medicare Supplement Plans are there?
There are up to 10 standardized Medicare Supplement plans available in most states. Learn more about Medicare Supplement insurance. You can compare Medicare Supplement plans and Medicare coverage options anytime you like, with no obligation. Type your zip code in the box on this page to begin.
Do you have to pay Medicare Part A or B?
Although both Medicare Part A and Part B have monthly premiums, whether you’re likely to pay a premium – and how much – depends on the “part” of Medicare. Most people don’t have to pay a monthly premium for Medicare Part A. If you’ve worked and paid Medicare taxes for at least 10 years (40 quarters), you typically don’t pay a premium.
What are preventive services?
Preventive services, like annual checkups and flu shots. Medical supplies and durable medical equipment, such as walkers and wheelchairs. Certain lab tests and screenings. Diabetes care, such as screenings, supplies, and a prevention program. Chemotherapy.
When is the annual election period?
Annual Election Period. From October 15 to December 7 each year is the Annual Election Period. This period is also referred to as the Annual Enrollment Period. During this time, you can elect to make changes to your Medicare coverage. You can switch Medicare Advantage plans, switch Part D plans, drop Original Medicare and enroll in ...
When does Medicare open enrollment end?
Any changes that you make will take effect on January 1 of the following year. Medicare Advantage Open Enrollment Period. This open enrollment period applies to recipients who are currently using a Medicare Advantage plan. This period lasts from January 1 to March 31 each year, and during this time, you can make one change to your healthcare ...
When does Medicare kick in?
If you make a change during the Medicare Advantage Open Enrollment Period, your new Medicare benefits will kick in on the first day of the month following your enrollment. For example, if you make a change to your Medicare Advantage plan at any point during the month of January, your new coverage will take effect on February 1.
What happens if you don't have health insurance?
Without health insurance that’s as good or better than Medicare, you could start racking up late-enrollment penalties the longer you go without coverage. If you decide to re-enroll in Part B later, these penalties could make your premiums (what you pay for coverage) even less affordable.
Is Medicare Part B free?
Medicare Part B helps qualified Americans pay health care costs related to doctor visits, lab testing, preventative services, and more, but this coverage isn't free, and not everyone needs it. Those who don’t need Part B can disenroll—but it’s not a straightforward process. The Centers for Medicare and Medicaid Services (CMS) ...
Is Medicare a secondary payer?
Conversely, a secondary payer health plan covers only costs left over after Medicare covers its share. If your health plan at work is a primary payer, that’s great. Feel free to drop your Part B coverage if you wish. The Part B premiums might not be worth any additional coverage you receive. But if you have secondary-payer insurance ...
Does Medicare Advantage pay for dental?
These plans aren't available in all areas, but even the average Medicare Advantage plan could help save you money. With most plans, you won't have to pay an extra premium ...
Can Medicare tack late enrollment penalties?
If you have a gap in coverage, the Medicare program could tack late-enroll ment penalties onto your Part B premiums if you re-enroll in coverage again later. Avoid this pitfall by working with your human resources department to ensure that your company's insurance is indeed creditable (meaning that it’s as good or better than Medicare Part B). You may need to provide documentation of creditable coverage during your Part B cancellation interview.
How to schedule an interview with Social Security?
Call a Licensed Agent: 833-271-5571. You can schedule an in-person or over-the-phone interview by contacting the SSA. If you prefer an in-person interview, use the Social Security Office Locator to find your nearest location. During your interview, fill out Form CMS 1763 as directed by the representative.