The ACA enabled people to gain coverage by 1) expanding the publicly funded Medicaid Medicaid in the United States is a federal and state program that helps with medical costs for some people with limited income and resources. Medicaid also offers benefits not normally covered by Medicare, including nursing home care and personal care services. The Health Insurance As…Medicaid
How does ACA affect Medicare?
- “Keep your hands off my Medicare.”. There is perhaps no quote more memorable – nor more contentious – from the battle over the Affordable Care Act (aka Obamacare ).
- Cost savings through Medicare Advantage. ...
- Focus on prescription drugs. ...
- Higher premiums for higher-income enrollees. ...
- Free preventive services. ...
- New funding for Medicare. ...
- Cost containment. ...
How did ACA affect Medicare?
- Payments to Health Care Providers. ...
- Payments to Medicare Advantage Plans. ...
- Medicare Benefit Improvements. ...
- Revenues to the Medicare Trust Funds. ...
- Medicare Part B and Part D Premiums for Higher-Income Beneficiaries. ...
- Payment and Delivery System Reforms and New Quality Incentives. ...
- Independent Payment Advisory Board. ...
How will ACA repeal affect Medicare?
Here are three key effects that a repeal of the ACA would have: Higher spending on Medicare Part A and Part B, leading to higher premiums, deductibles and copayments for beneficiaries. The Congressional Budget Office estimates that the ACA reduced Medicare spending by $350 billion over 10 years just by changing how providers are paid.
What are the pros and cons of ACA?
The ACA Has 10 Sections in All, and Most Do More Than Provide Insurance
- It created the National Prevention Council that coordinates all federal health efforts to promote active, drug-free lifestyles.
- It funds scholarships and loans to double the number of healthcare providers in five years.
- It cuts down on fraudulent doctor/supplier relationships.
See more
How does the ACA affect the US health care system and Medicare?
The ACA reduced the annual increases in payments to hospitals under the traditional Medicare program. It also reduced payments to Medicare Advantage plans. Partly because of these measures, increases in Medicare expenditures have been 20 percent lower than projected since the law was enacted.
Did the ACA expand Medicare?
The Affordable Care Act's (ACA) Medicaid expansion expanded Medicaid coverage to nearly all adults with incomes up to 138% of the Federal Poverty Level ($17,774 for an individual in 2021) and provided states with an enhanced federal matching rate (FMAP) for their expansion populations.
How will ACA repeal affect Medicare?
Dismantling the ACA could thus eliminate those savings and increase Medicare spending by approximately $350 billion over the ten years of 2016- 2025. This would accelerate the insolvency of the Medicare Trust Fund.
What changes did the Patient Protection and Affordable Care Act of 2010 make to the Medicaid program?
To provide for those who need long-term care, the Act creates new Medicaid options to promote community-based care and protect spouses of those with serious illness from becoming impoverished. It also creates a voluntary long-term-care insurance program, the Community Living Assistance Services and Support Act.
Does Medicaid fall under the Affordable Care Act?
Key Federal Provisions The 2010 Affordable Care Act (ACA) expands Medicaid to all Americans under age 65 whose family income is at or below 133 percent of federal poverty guidelines ($14,484 for an individual and $29,726 for a family of four in 2011) by Jan. 1, 2014.
Is Affordable Care Act and Medicare the same thing?
Medicare is a federal health insurance program for Americans over age 65 and certain people under age 65 who have qualifying conditions or disabilities. "Obamacare" is a nickname for the Patient Protection and Affordable Care Act of 2010 (also known as the ACA). Learn more about the basics of Medicare vs.
How does the Affordable Care Act affect the elderly?
"The ACA expanded access to affordable coverage for adults under 65, increasing coverage for all age groups, races and ethnicities, education levels, and incomes."Under the ACA, older adults' uninsured rate has dropped by a third, indicators of their health and wellness have improved, and they're now protected from ...
How does the Affordable Care Act affect Medicaid quizlet?
How did the Affordable Care Act affect Medicaid? Federal government will provide funds for increases in payments to primary care doctors, including family physicians, internal medicine, and pediatricians.
Why are there variations of Medicaid after the Affordable Care Act was enacted?
Medicaid enrollment has grown regardless of expansion status in most states following implementation of the ACA. This is likely due to the so-called welcome-mat effect in which enrollment increases among individuals who were previously eligible for coverage but not enrolled.
What is the difference between Medicaid and the Affordable Care Act?
The Obamacare scheme seeks to ensure everyone gets affordable health insurance coverage while the Medicaid scheme provides health insurance to Americans who are above 65 years of age. It also covers younger citizens with certain qualifying disabilities like End-Stage Renal Disease.
How did the ACA increase the number of Americans with health insurance?
Beyond the Medicaid expansion, the ACA sought to increase the number of Americans with health insurance by providing new premium tax credits for the purchase of private health insurance and made a number of reforms to the private insurance market, such as eliminating preexisting condition exclusions and establishing annual limits on out-of-pocket costs. The law also allowed young adults to remain on their parents’ insurance plans up to age 26 and required most individuals to secure minimum essential coverage. 2
When did the Supreme Court rule on Medicaid expansion?
Originally a requirement, the June 2012 Supreme Court ruling in National Federation of Independent Business v. Sebelius effectively made the Medicaid expansion an option. To date, almost three-quarters of states have opted to expand.
What is the ACA 111-148?
The Patient Protection and Affordable Care Act (ACA, P.L. 111-148, as amended) made a number of changes to Medicaid. Perhaps the most widely discussed is the expansion of eligibility to adults with incomes up to 133 percent of the federal poverty level (FPL). 1
Does the ACA require a single application for Medicaid?
The ACA also included provisions to streamline eligibility, enrollment, and renewal processes, for example, by requiring a single application for Medicaid, CHIP, and subsidized exchange coverage. In part due to these changes, enrollment and spending in Medicaid has increased in all states, regardless of whether the state expanded coverage ...
How does the ACA affect health care?
The Patient Protection and Affordable Care Act (ACA) expands access to health insurance in the United States , and, to date, an estimated 20 million previously uninsured individuals have gained coverage. Understanding the law’s impact on coverage, access, utilization, and health outcomes, especially among low-income populations, is critical to informing ongoing debates about its effectiveness and implementation. Early findings indicate that there have been significant reductions in the rate of uninsurance among the poor and among those who live in Medicaid expansion states. In addition, the law has been associated with increased health care access, affordability, and use of preventive and outpatient services among low-income populations, though impacts on inpatient utilization and health outcomes have been less conclusive. Although these early findings are generally consistent with past coverage expansions, continued monitoring of these domains is essential to understand the long-term impact of the law for underserved populations.
How does the reliance on the ACA affect health insurance?
Despite the availability of subsidies and cost-sharing reductions, the reliance of the ACA on health insurance exchanges may both increase access to health insurance and simultaneously pose unintended barriers to access, particularly for low-income populations. These barriers can arise in two ways. The most publicized method is through the creation of narrow networks, where insurers offer plans and policies with fewer doctors and hospitals in an effort to keep premiums as competitive as possible. Whether narrow networks create actual, rather than perceived, barriers to care has not been well established yet through research. Nevertheless, the existence of narrow networks has created the perception that exchange-based QHPs are limiting access to a greater extent than did pre-ACA policies, despite the absence of adequate baseline data from pre-ACA years.
What is the coverage gap?
Approximately 9% of the remaining uninsured (almost 3 million Americans) fall into what is known as the “coverage gap.” This group represents poor, uninsured adults who reside in the 19 non–Medicaid expansion states whose income is above the state’s threshold for Medicaid eligibility but less than the 100% threshold for Marketplace subsidy eligibility. Also included are childless adults who were not previously eligible for Medicaid. Almost 90% of all adults in the coverage gap live in the South, half in either Texas or Florida, which aligns with this region’s high uninsurance rates, limited Medicaid eligibility, and low uptake of Medicaid expansion (37). Consistent with demographic characteristics and policies excluding nondisabled adults in states that did not expand Medicaid, African Americans and childless adults also account for a disproportionate share of individuals in the coverage gap (37). If all current nonexpansion states opted to expand Medicaid, 5.2 million currently uninsured adults would gain coverage: 2.9 million who are in the coverage gap, 0.5 million who are already eligible for Medicaid though alternate pathways, and an additional 1.8 million who are presently eligible for Marketplace subsidies with incomes from 100% FPL to 138% FPL yet did not enroll (37). Because a substantial portion of the remaining uninsured are either eligible for coverage or fall in the coverage gap, the law’s potential impact on the poor has not yet been fully realized.
How effective is Medicaid expansion?
The expansion of Medicaid has been particularly effective in states that took advantage of the opportunity for early Medicaid expansion allowed under the ACA. Between 2010 and 2014, six states (California, Colorado, Connecticut, Minnesota, New Jersey, Washington) and the District of Columbia extended Medicaid eligibility for low-income adults through the early Medicaid expansion option or the Section 1115 waiver process (18). In California, the LIHP significantly increased coverage by 7.3 percentage points for poor adults (up to 138% FPL) within the first two years (38). Similarly, one year after early expansion, Medicaid coverage increased significantly in Connecticut (4.9 percentage points) and modestly in Washington, DC (3.7 percentage points) among low-income childless adults—a key subpopulation targeted by Medicaid expansion (86). Trends in coverage gains in these early expansions echoed those of the Massachusetts health reform, which was associated with an estimated 18.4-percentage-point increase in coverage among low-income adults and even larger gains among low-income childless adults (54). Though these expansions were implemented prior to the ACA, their positive findings inform potential coverage gains for the poor under the ACA.
What are the effects of pre-ACA coverage?
Pre-ACA insurance expansions have largely demonstrated improved access to care for low-income populations. For example, the Massachusetts health reform was associated with significant reductions in forgone or delayed care and improvements in access to a personal doctor and usual source of care among adults overall (46, 54, 56, 58, 72, 88) and, in particular, for subgroups targeted by the ACA, such as low-income and childless adults (54, 56, 58). With regard to affordability, the Medicaid expansion in Oregon diminished financial hardship from medical costs, markedly reducing catastrophic OOP expenditures (5, 35, 98). In addition, other states that expanded public insurance prior to the ACA demonstrated improvements in access and affordability among low-income adults (62, 82) and children (33, 44) across comparable measures. More recently, the California LIHP waiver project found large reductions in the likelihood of any family OOP health care spending but did not detect significant differences in access to care, which may be explained by a well-established safety net in the state prior to program implementation (38). One ongoing concern about expanding coverage is that increased demand for services by newly insured individuals may limit access to care, but evidence from prior expansions does not appear to sufficiently support this hypothesis (67).
What is the goal of increased coverage eligibility and affordability?
An important goal of increased coverage eligibility and affordability is to increase access to adequate health care services for the poor. As a result, the ACA’s impact on access to high-quality health care has been evaluated across multiple dimensions, including access to a doctor, having a usual source of care, timeliness of care, affordability, and access to medications and preventive, primary, and specialty care.
Does the ACA expand Medicaid?
In summary, early evidence following ACA implementation has demonstrated significant progress toward its goal of expanding coverage for millions of low-income individuals who would have otherwise remained uninsured. Not all individuals equally experience the potential benefits of the law, however, and disparities have developed on the basis of state decisions regarding whether to expand Medicaid.
How did the Affordable Care Act affect Medicare?
The Affordable Care Act also affected Medicare by adding coverage for a "Wellness Visit" and a “Welcome to Medicare” preventative visit. It also eliminated cost-sharing for almost all of the preventive services covered by Medicare.
When was the Affordable Care Act signed into law?
December 10, 2019. The Affordable Care Act was signed into law on March 23, 2010. Its goals were to provide greater access to health care coverage, to improve the quality of health care services provided, and to slow the rate of increase in health spending. As far as Medicare is concerned, the Affordable Care Act primarily made improvements ...
What is the Affordable Care Act?
The Affordable Care Act provides ways for hospitals, doctors and other health care providers to coordinate their care for Medicare beneficiaries. As a result, health care quality is improved and unnecessary spending is reduced.
What are the initiatives under the Affordable Care Act?
Under these initiatives, your doctor may get additional resources that will help ensure that your treatment is consistent. The Affordable Care Act provides ways for hospitals, doctors and other health care providers to coordinate their care for Medicare beneficiaries. As a result, health care quality is improved and unnecessary spending is reduced.
How much does Medicare pay for generic drugs?
In 2016, people with Medicare paid 45% for brand-name drugs and 58% for generic drugs while in the coverage gap. These percentages have shrunk over the last few years. Starting in 2020, however, you’ll pay only 25% for covered brand-name and generic drugs during the coverage gap.
How long does Medicare cover preventive visits?
This is a one-time visit. During the visit, your health care provider will review your health, as well as provide education and counseling about preventive services and other care.
How long does it take to sign up for Medicare?
You will get an initial enrollment period to sign up for Medicare. In most cases, the initial enrollment period begins three months before your 65th birthday and ends three months afterward. For most people, it’s beneficial to sign up for Medicare during this time. This is because those who sign up for Medicare after the initial enrollment period ends, face some negative consequences. For example, you might be required to pay a Part B (medical insurance) late enrollment penalty for as long as you have Medicare. Also, you are only permitted to enroll in Medicare Part B (and Part A in some cases) during the Medicare general enrollment period that runs from January 1 to March 31 each year. However, coverage will not begin until July of that year. This could create a gap in your insurance coverage.
How does the ACA affect Medicaid?
The ACA’s Medicaid eligibility and enrollment changes may affect people with disabilities. The 2014 rules seek to allow people with disabilities to enroll in coverage as quickly as possible (either in Medicaid based solely on their low income or in a Marketplace QHP with APTC, where eligible), even while their Medicaid eligibility in a disability-related coverage group is being determined. The 2014 rules also seek to ensure that people who qualify in a disability-related Medicaid coverage group or who are medically frail can access the most appropriate benefits package for their needs. As these rules are implemented, it will be important to continue to assess how eligibility and benefits for people with disabilities are affected by the new streamlined eligibility, enrollment and renewal procedures, coordination between state Medicaid agencies and the Marketplaces, application screening questions, and the extent to which states align their new adult ABPs with state plan benefits.
How does the ACA affect Medicaid eligibility?
The 2014 rules seek to allow people with disabilities to enroll in coverage as quickly as possible (either in Medicaid based solely on their low income or in a Marketplace QHP with APTC, where eligible), even while their Medicaid eligibility in a disability-related coverage group is being determined. The 2014 rules also seek to ensure that people who qualify in a disability-related Medicaid coverage group or who are medically frail can access the most appropriate benefits package for their needs. As the ACA’s 2014 eligibility and enrollment rules are implemented, it will be important to continue to assess how eligibility determinations and benefits for people with disabilities are affected by the new streamlined eligibility, enrollment and renewal procedures, coordination between state Medicaid agencies and the Marketplaces, the application screening questions, and the extent to which states align their new adult ABPs with state plan benefits.
What are the changes to Medicaid?
The Affordable Care Act (ACA) makes several changes to Medicaid eligibility and enrollment rules that may affect people with disabilities. While the ACA’s adult coverage expansion is effectively a state option, other changes apply to all state Medicaid programs as of 2014, including simplified eligibility determination procedures with a new income counting methodology and increased reliance on electronic data matching; modernizations to the application and renewal processes; and coordination with other insurance affordability programs, including the new Marketplaces that offer qualified health plans (QHPs) and administer advance payment of premium tax credits (APTC) and cost-sharing reductions.
What is the poverty level for Medicaid in 2014?
As of 2014, the ACA expands Medicaid eligibility up to 138% of the federal poverty level (FPL, $16,104 for an individual in 2014), although implementation of the expansion is effectively a state option. In states that are not implementing the ACA’s Medicaid expansion, people with disabilities can qualify for Medicaid based solely on their low ...
What are the requirements for Medicaid?
The ADA and Section 504 also require state Medicaid agencies to: 1 provide information about eligibility requirements, available Medicaid services, and the rights and responsibilities of applicants and beneficiaries in a way that is accessible to people with disabilities. 52 This information must be provided to all applicants and anyone who requests it, not just people with disabilities. Information must be available in paper and electronic forms, including online, and orally as appropriate, and must be provided in plain language. 2 provide assistance to people seeking help with the application or renewal process in a manner that is accessible to people with disabilities. 53 This assistance must be provided to anyone, not just people with disabilities, and must be available in person, by phone, and online. State Medicaid agencies also must allow applicants and beneficiaries to have a person of their choice assist them with the application and renewal process. 3 use applications, supplemental forms, renewal forms and notices that are accessible to people with disabilities. 54 CMS intends to issue future guidance with specific accessibility standards after consulting with states and other stakeholders.
Is Medicaid an insurance?
Executive Summary. Medicaid is an important source of health insurance coverage for people with disabilities. This issue brief explains how Medicaid eligibility and benefits for people with disabilities are affected by the Affordable Care Act (ACA) rules as of 2014. Marketplace rules are discussed to the extent that they relate to Medicaid ...
Is Medicaid a source of health insurance?
While Medicaid often is regarded as a source of health insurance for people with low incomes, the program also provides important primary or supplemental coverage for people with disabilities. This is true in part because health insurance typically is offered as an employment benefit, making it inaccessible to people with disabilities who are ...
How long will the ACA last?
The ACA ensures the protection of Medicare for years to come. The life of the Medicare Trust fund will be extended to at least 2029—a 12-year extension due to reductions in waste, fraud and abuse, and Medicare costs, which will provide you with future savings on your premiums and coinsurance.”
When will Medicaid phase down?
Beginning in 2014 coverage for the newly eligible adults will be fully funded by the federal government for three years. It will phase down to 90% by 2020.
What do you need to know about the Affordable Care Act?
Per the Medicare.gov website, here are the “top five things you need to know” about the Affordable Care Act (ACA) if you have Medicare: “Your Medicare coverage is protected. Medicare isn’t part of the Health Insurance Marketplace established by ACA, so you don’t have to replace your Medicare coverage with Marketplace coverage.
What is a new office for Medicare?
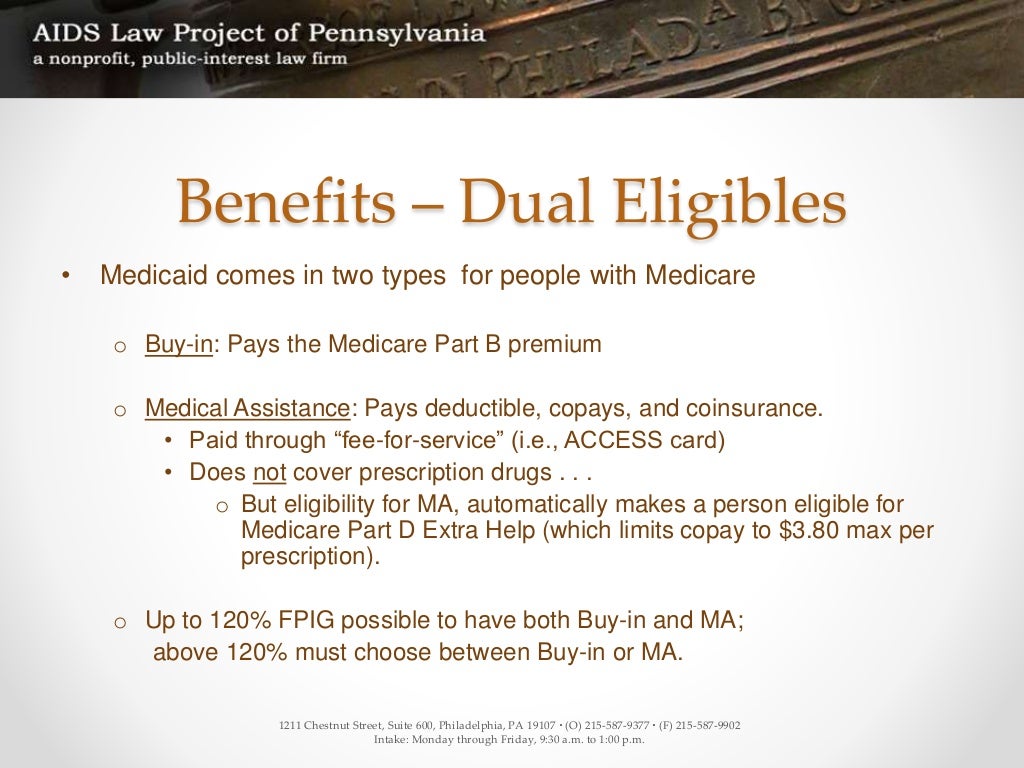
A new office will be created within the Centers for Medicare & Medicaid Services to coordinate care for individuals who are eligible for both Medicaid and Medicare (“dual eligibles” or Medicare-Medicaid enrollees)
Is the Affordable Care Act up and running?
The Affordable Care Act’s new health insurance marketplaces are now up and running. The exchanges will allow Americans without insurance, or those unhappy with current coverage options to buy private plans at a variety of price points.
Does Alabama have an exchange?
Unlike many states, Alabama has opted not to set up its own exchange, so residents will need to purchase through the federally-facilitated exchange at Healthcare.gov. Click here to get started exploring your plan options.
Does Medicare cover mammograms?
You get more preventive services, for less. Medicare now covers certain preventive services, like mammograms or colonoscopies, without charging you for the Part B coinsurance or deductible. You also can get a free yearly “Wellness” visit. You can save money on brand-name drugs.
How does the ACA affect Medicaid?
The new enrollment data reported by CMS suggest that the ACA is having a strong positive impact on Medicaid enrollment, particularly in states that have implemented the Medicaid expansion. However, ultimately the key measure of the ACA’s success will changes in the number of uninsured. Early survey findings show promising reductions in the uninsured rate to date. However, fully assessing the impact of the ACA will require monitoring changes in coverage over longer periods of time to determine changing patterns in health insurance coverage and access to care and the extent to which individuals are able to maintain continuous coverage. While waiting for these measures is challenging, they ultimately will provide the most meaningful measures of the ACA’s progress in achieving its broader coverage goals. In the meantime, the data released by CMS is expected to continue to improve and expand over time, allowing for greater analysis, and surveys like the Kaiser Survey of Low-income Americans will provide insight into low-income consumers’ experiences to provide greater understanding about the impact of the ACA on the low-income uninsured.7
How did the ACA impact the enrollment of Medicaid?
Increased outreach and enrollment efforts. The ACA spurred outreach and enrollment efforts to help connect eligible people to coverage. Leading up to and throughout the open enrollment period for the Marketplaces, there was significant outreach to encourage individuals to apply for coverage and an array of assistance was available to help individuals enroll. Moreover, because Medicaid enrollment is not limited to the Marketplace open enrollment period, Medicaid outreach and enrollment efforts continue year-round.
What are the changes to Medicaid?
Overall, there are three main changes the ACA makes to eligibility and enrollment that are expected to contribute to Medicaid enrollment gains (Figure 1): Figure 1: ACA Medicaid Changes that Will Impact Enrollment. Medicaid expansion to low-income adults. The ACA expands Medicaid eligibility to adults with incomes at or below 138 percent ...
How many people were on Medicaid in 2014?
As of March 2014, Medicaid and CHIP enrollment grew by more than 4.8 million people compared to average monthly enrollment in the three months leading up to the start of open enrollment.
How many states are expanding Medicaid?
To date, 27 states, including DC, are implementing the expansion and additional states may expand moving forward. 1. Modernized, simpler enrollment processes. The ACA makes it easier for people to enroll in and renew Medicaid coverage.
What percentage of the poverty line is Medicaid?
Medicaid expansion to low-income adults. The ACA expands Medicaid eligibility to adults with incomes at or below 138 percent of the poverty line, which is just over $16,000 per year for an individual today.
Is Medicaid open enrollment year round?
Moreover, because Medicaid enrollment is not limited to the Marketplace open enrollment period, Medicaid outreach and enrollment efforts continue year-round. Together, these three key changes are expected to lead to increased Medicaid coverage and a reduction in the number of uninsured.
