Does the amount of Medicare tax change?
· The new tax law did a couple of things to affect Medicare costs. Number one, it added a new tier on the top. This won’t affect many people – it’s for people who make $500,000 and above if you’re a single filer or $750,000 for joint filers. That’s not as big of a deal.
Will the Affordable Care Act change Medicare?
· As part of the Medicare payment solution that Congress enacted in 2015 to solve the “doc fix” problem, new income brackets were created to determine Part B premiums for high-income Medicare enrollees. These new brackets took effect in 2018, bumping some high-income enrollees into higher premium brackets.
What changes are coming to Medicare in 2019?
· To aid in this effort, the ACA added an additional Medicare tax for high income earners. This raised the tax from 1.45 percent to 2.34 percent for people with an earned annual income of more than $200,000 ($250,000 for married couples filing jointly). 1
When did the government start reducing Medicare Advantage costs?
· The annual Part B deductible will be $233 this year, an increase of $30. For Medicare Part A, which covers hospitalizations, hospice care and some nursing facility and home health services, the inpatient deductible that enrollees must pay for each hospital admission will be $1,556, an increase of $72 over 2021.

How did the ACA change Medicare?
Medicare Premiums and Prescription Drug Costs The ACA closed the Medicare Part D coverage gap, or “doughnut hole,” helping to reduce prescription drug spending. It also increased Part B and D premiums for higher-income beneficiaries. The Bipartisan Budget Act (BBA) of 2018 modified both of these policies.
Why did my employee Medicare tax go up?
The Affordable Care Act expanded the Medicare payroll tax to include the Additional Medicare Tax. This new Medicare tax increase requires higher wage earners to pay an additional tax (0.9%) on earned income. All types of wages currently subject to the Medicare tax may also be subject to the Additional Medicare Tax.
Why is Medicare taken out of my paycheck?
If you see a Medicare deduction on your paycheck, it means that your employer is fulfilling its payroll responsibilities. This Medicare Hospital Insurance tax is a required payroll deduction and provides health care to seniors and people with disabilities.
What are the 2021 tax law changes?
A temporary tax change enacted in the CARES Act allows taxpayers who select standard deduction, to claim a deduction of up to $300 for cash contributions made to qualifying charities in 2021. It increases to $600 for those filing married and filing jointly.
Who pays additional Medicare tax 2021?
The Additional Medicare Tax applies to people who are at predetermined income levels. For the 2021 tax year, those levels are: Single tax filers: $200,000 and above. Married tax filers filing jointly: $250,000 and above.
What is the additional Medicare tax for 2021?
0.9%2021 updates. 2.35% Medicare tax (regular 1.45% Medicare tax + 0.9% additional Medicare tax) on all wages in excess of $200,000 ($250,000 for joint returns; $125,000 for married taxpayers filing a separate return). (Code Sec. 3101(b)(2))
Can you opt out of paying Medicare tax?
The problem is that you can't opt out of Medicare Part A and continue to receive Social Security retirement benefits. In fact, if you are already receiving Social Security retirement benefits, you'll have to pay back all the benefits you've received so far in order to opt out of Medicare Part A coverage.
At what income do you stop paying Medicare tax?
FICA tax includes a 6.2% Social Security tax and 1.45% Medicare tax on earnings. In 2021, only the first $142,800 of earnings are subject to the Social Security tax ($147,000 in 2022). A 0.9% Medicare tax may apply to earnings over $200,000 for single filers/$250,000 for joint filers.
Do I get a refund on Medicare tax withheld?
If your employer has withheld Social Security or Medicare taxes in error, follow these steps: Request a refund from your employer. You must first request a refund of these taxes from your employer. If your employer is able to refund these taxes, no further action is necessary.
Is there an extra deduction for over 65 in 2021?
Increased Standard Deduction: You qualify for a larger standard deduction if you or your spouse is age 65 or older. The standard deduction for single seniors in 2021 is $1,700 higher than the deduction for taxpayer younger than 65 who file as single or head of household.
How much of my Social Security is taxable in 2021?
For the 2021 tax year (which you will file in 2022), single filers with a combined income of $25,000 to $34,000 must pay income taxes on up to 50% of their Social Security benefits. If your combined income was more than $34,000, you will pay taxes on up to 85% of your Social Security benefits.
At what age is Social Security no longer taxed?
At 65 to 67, depending on the year of your birth, you are at full retirement age and can get full Social Security retirement benefits tax-free.
Q: What are the changes to Medicare benefits for 2022?
A: There are several changes for Medicare enrollees in 2022. Some of them apply to Medicare Advantage and Medicare Part D, which are the plans that...
How much will the Part B deductible increase for 2022?
The Part B deductible for 2022 is $233. That’s an increase from $203 in 2021, and a much more significant increase than normal.
Are Part A premiums increasing in 2022?
Roughly 1% of Medicare Part A enrollees pay premiums; the rest get it for free based on their work history or a spouse’s work history. Part A premi...
Is the Medicare Part A deductible increasing for 2022?
Part A has a deductible that applies to each benefit period (rather than a calendar year deductible like Part B or private insurance plans). The de...
How much is the Medicare Part A coinsurance for 2022?
The Part A deductible covers the enrollee’s first 60 inpatient days during a benefit period. If the person needs additional inpatient coverage duri...
Can I still buy Medigap Plans C and F?
As a result of the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA), Medigap plans C and F (including the high-deductible Plan F) are n...
Are there inflation adjustments for Medicare beneficiaries in high-income brackets?
Medicare beneficiaries with high incomes pay more for Part B and Part D. But what exactly does “high income” mean? The high-income brackets were in...
How are Medicare Advantage premiums changing for 2021?
According to CMS, the average Medicare Advantage (Medicare Part C) premiums for 2022 is about $19/month (in addition to the cost of Part B), which...
Is the Medicare Advantage out-of-pocket maximum changing for 2022?
Medicare Advantage plans are required to cap enrollees’ out-of-pocket costs for Part A and Part B services (unlike Original Medicare, which does no...
How is Medicare Part D prescription drug coverage changing for 2022?
For stand-alone Part D prescription drug plans, the maximum allowable deductible for standard Part D plans is $480 in 2022, up from $445 in 2021. A...
Did Medicare and Social Security change?
Recent updates in the new tax law to Medicare and Social Security rules may not seem like that big of a deal, but they did change some of the rules. How is that going to impact your retirement income? When taken together, there were 7 changes to Medicare means testing, Social Security cost of living adjustments, and claiming strategies that could increase healthcare costs and reduce the value of your benefits, according to a report by InvestmentNews.
Is the $170,000 threshold adjusted for inflation?
And, unfortunately, these $85,000 and $170,000 thresholds are not adjusted for cost of living on an annual basis. So, these thresholds affect more and more people every year due to inflation.
Did Medicare go up in 2018?
That means that your Medicare premium didn’t go up. In 2018, the cost of living adjustment went up 2.3 percent. For the average beneficiary, however, almost all of that increase was wiped out by a Medicare premium increase. If you make over the defined thresholds, though, you’re not protected by the “hold harmless” clause.
When did Medicare start putting new brackets?
These new brackets took effect in 2018, bumping some high-income enrollees into higher premium brackets.
When will Medicare Part D change to Advantage?
Some of them apply to Medicare Advantage and Medicare Part D, which are the plans that beneficiaries can change during the annual fall enrollment period that runs from October 15 to December 7.
How many people will have Medicare Advantage in 2020?
People who enroll in Medicare Advantage pay their Part B premium and whatever the premium is for their Medicare Advantage plan, and the private insurer wraps all of the coverage into one plan.) About 24 million people had Medicare Advantage plans in 2020, and CMS projects that it will grow to 26 million in 2021.
When will Medicare stop allowing C and F?
As a result of the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA), Medigap plans C and F (including the high-deductible Plan F) are no longer available for purchase by people who become newly-eligible for Medicare on or after January 1, 2020.
How long is a skilled nursing deductible?
See more Medicare Survey results. For care received in skilled nursing facilities, the first 20 days are covered with the Part A deductible that was paid for the inpatient hospital stay that preceded the stay in the skilled nursing facility.
How much is the Medicare coinsurance for 2021?
For 2021, it’s $371 per day for the 61st through 90th day of inpatient care (up from $352 per day in 2020). The coinsurance for lifetime reserve days is $742 per day in 2021, up from $704 per day in 2020.
Does Medicare Advantage have a copay?
Many Medicare Advantage plans have low copays and deductibles that don’t necessarily increase in lockstep with the Part B deductible, so their benefits designs have had different fluctuations over the last few years. [Medicare Advantage enrollees pay the Part B premium plus the Advantage plan premium if the plan has a separate premium. Medicare Advantage plans wrap Part A, Part B, usually Part D, and various supplemental coverage together into one plan, with out-of-pocket costs that are different from Original Medicare.]
How is Medicare financed?
1-800-557-6059 | TTY 711, 24/7. Medicare is financed through two trust fund accounts held by the United States Treasury: Hospital Insurance Trust Fund. Supplementary Insurance Trust Fund. The funds in these trusts can only be used for Medicare.
When was the Affordable Care Act passed?
The Affordable Care Act (ACA) was passed in 2010 to help make health insurance available to more Americans. To aid in this effort, the ACA added an additional Medicare tax for high income earners.
What is the surtax rate for 2021?
The additional tax (0.9% in 2021) is the sole responsibility of the employee and is not split between the employee and employer. If you make more than $200,000 per year in 2021, the 0.9 percent surtax only applies to the amount you make that is over $200,000.
Who can help with Medicare enrollment?
If you’d like more information about Medicare, including your Medicare enrollment options, a licensed insurance agent can help.
How much Medicare tax do self employed pay?
Medicare taxes for the self-employed. Even if you are self-employed, the 2.9% Medicare tax applies. Typically, people who are self-employed pay a self-employment tax of 15.3% total – which includes the 2.9% Medicare tax – on the first $142,800 of net income in 2021. 2. The self-employed tax consists of two parts:
What is Medicare Part A?
Medicare Part A premiums from people who are not eligible for premium-free Part A. The Hospital Insurance Trust Fund pays for Medicare Part A benefits and Medicare Program administration costs. It also pays for Medicare administration costs and fighting Medicare fraud and abuse.
How is the Hospital Insurance Trust funded?
The Hospital Insurance Trust is largely funded by Medicare taxes paid by employees and employers , but is also funded by: The Hospital Insurance Trust Fund pays for Medicare Part A benefits and Medicare Program administration costs. It also pays for Medicare administration costs and fighting Medicare fraud and abuse.
How will the new tax plan affect health care?
How the New U.S. Tax Plan Will Affect Health Care. It will mean less coverage, less revenue, and a less productive workforce. Summary. Earlier today, the U.S. House of Representatives passed a new tax bill which will eliminate the penalties against people who don’t have health insurance and significantly increase the federal deficit.
How much of the federal budget was spent on Medicare and Medicaid in 2016?
Because Medicare and Medicaid together accounted for about $1.25 trillion in federal spending in 2016, about 30% of the federal budget, they will be the major targets for deficit reduction. There is no guarantee that such efforts will succeed, but if they do, reforms could take a number of directions.
How many Americans will lose health insurance?
But there are also practical questions for American businesses. The 13 million Americans who will lose health insurance and many millions of Medicaid eligible individuals who may lose coverage or benefits are current or potential workers whose health influences their productivity.
Is a precipitous cut bad for Medicare?
Precipitous cuts, however, could be damaging. In any case, if the nation were to embark on a drive to make the delivery of health care more efficient, Medicare and Medicaid would not be the most promising places to start.
Will Medicaid reforms reduce the size of government?
For Medicaid, reforms would likely lead similarly to fewer people covered, reduced benefits, and/or higher cost-sharing. For conservatives who have long sought to reduce the generosity of entitlements in the United States, these changes would be a welcome way to reduce the size of government.
What age can you get Medicare?
For Medicare, this could include increasing the eligibility age from 65 to 67 or beyond (resulting in fewer covered elderly), caps on spending per beneficiary (possibly reducing covered benefits), or increases in cost-sharing that would lead to beneficiaries using fewer services.
How many people will not buy health insurance after the ACA repeal?
According to the Congressional Budget Office (CBO), the repeal of the individual mandate penalties could result in as many as 13 million fewer Americans having health insurance. About 5 million are projected to be people who previously bought health insurance as individuals either within or outside the ACA’s marketplaces. Some will choose not to buy insurance because the penalty has disappeared. Others, especially higher-income individuals who don’t qualify for subsidies under the ACA, will drop insurance because of increases in average premiums predicted by the CBO. These premium increases will occur because, with the repeal of the mandate, many young, healthy people will exit markets, leaving a sicker, more costly insurance pool behind. Older individuals will be most affected. For example, a 60-year-old not receiving subsidies could face premium increases of $1,781, $1,469, $1,371, and $1,504, respectively, in Alaska, Arizona, Nevada, and Maine.
How did the ACA reduce Medicare costs?
Cost savings through Medicare Advantage. The ACA gradually reduced costs by restructuring payments to Medicare Advantage, based on the fact that the government was spending more money per enrollee for Medicare Advantage than for Original Medicare. But implementing the cuts has been a bit of an uphill battle.
When did Medicare start phasing in?
In 2011, the law froze the benchmark amount at 2010 levels for the maximum amount paid for MA plans in each county. Then, in 2012, the government began phasing in payment reductions to Medicare Advantage in an effort to bring Medicare Advantage spending in line with the fee-for-service program (Original Medicare), although benchmark amounts could also increase based on plan quality.
When was Medicare Part D created?
When Medicare Part D was created in 2003, part of the legislation specifically forbid the government from negotiating drug prices with manufacturers, and that has continued to be the case. There has been considerable debate about changing this rule, but it has met with continued pushback from the pharmaceutical lobby.
Is there a donut hole in Medicare?
Technically, this means that there is no longer a donut hole, but it’s important to understand that the donut hole concept is still relevant: It plays a role in determining how your out-of-pocket costs are counted and who actually pays for your drugs (you, your health plan, the drug manufacturer, or the Medicare program).
What percentage of Medicare donut holes are paid?
The issue was addressed immediately by the ACA, which began phasing in coverage adjustments to ensure that enrollees will pay only 25 percent of “donut hole” expenses by 2020, compared to 100 percent in 2010 and before.
How many Medicare Advantage plans will be available in 2021?
For 2021, there are 21 Medicare Advantage and/or Part D plans with five stars. CMS noted that more than three-quarters of all Medicare beneficiaries enrolled in Medicare Advantage plans with integrated Part D prescription coverage would be in plans with at least four stars as of 2021.
Is Medicare Advantage free?
Medicare Advantage takes the place of Medicare A and B. For most seniors, Medicare A is free, but Medicare B has a premium of $148.50/month for most beneficiaries in 2021; it’s important to understand that Medicare Advantage enrollees have to pay their Medicare Part B premium in addition to whatever premium they owe for the Medicare Advantage plan, so a zero-premium plan would mean that the person just has to pay the Part B premium.
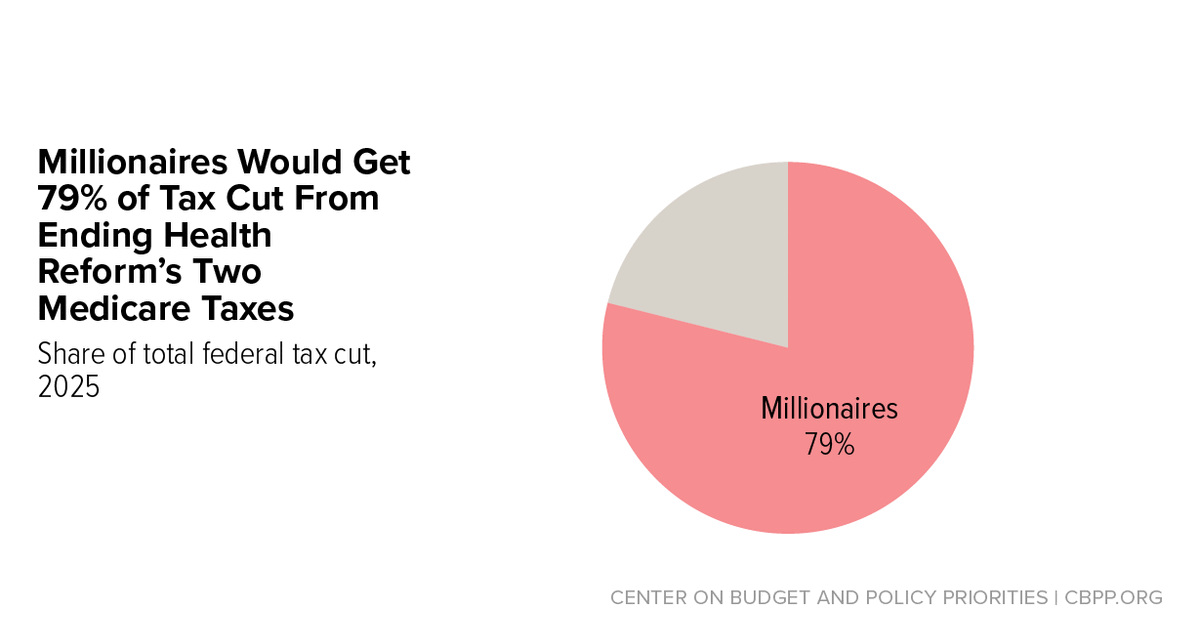
How much did Medicare raise in 2019?
The additional Medicare tax raised $10 billion and the NII tax raised $31 billion in 2019. Nearly all families affected by the additional Medicare tax and NII tax are in the top 5 percent of income, with most of the burden borne by families in the top 1 percent of income.
When will the medical device tax be repealed?
Subsequent legislation passed in late 2019 permanently repealed the medical device tax starting in 2020 and the health-insurer tax starting in 2021. Excise taxes on the health care industry raised $12 billion in 2019.
What is the medical deduction limit?
An additional limit on the medical expense deduction. Pre-ACA, taxpayers could deduct medical expenses exceeding 7.5 percent of income when calculating taxable income. The ACA increased the threshold to 10 percent of income, and later legislation temporarily lowered the limit back to 7.5 percent until 2021, when the threshold is scheduled to in-crease to 10 percent.
When was the Cadillac tax repealed?
However, the Cadillac tax was repealed by the Further Consolidated Appropriations Act of 2020. Tax changes were an important component of the package of reforms enacted by the ACA. Any major change to the ACA would require making tax policy decisions with implications for health insurance coverage, the budget deficit, ...
What is Cadillac tax?
An excise tax on employer-sponsored health benefits whose value exceeds specified thresholds (the “Cadillac tax”). Including the impact on income and payroll taxes, the tax on high-cost health plans was projected to raise $8 billion in 2022 with the revenue gain growing rapidly over time, reaching $39 billion by 2028. The Cadillac tax would have reduced after-tax incomes the most in percentage terms for middle-income families. However, the Cadillac tax was repealed by the Further Consolidated Appropriations Act of 2020.
When did the individual mandate end?
The 2017 Tax Cuts and Jobs Act eliminated the individual mandate starting in 2019.
How much is excise tax on Medicare?
Excise taxes on the health care industry raised $12 billion in 2019. An additional 0.9 percent Medicare tax on earnings and a 3.8 percent tax on net in-vestment income (NII) for individuals with incomes exceeding $200,000 and couples with incomes exceeding $250,000.
What will happen to capital gains tax in 2022?
After 2022, the thresholds would be indexed for inflation. Increase capital gain rates: Long-term capital gains and qualified dividends of taxpayers with an adjusted gross income of more than $1 million would be taxed at ordinary income tax rates, with 37% generally being the highest rate (40.8% including the net investment income tax), ...
What is the SECA tax for 2022?
Beginning in 2022, the additional income that would be subject to SECA tax would be the lesser of (i) the potential SECA income , and (ii) the excess over $400,000 of the sum of the potential SECA income, wage income subject to FICA under current law, and 92.35% of self-employment income subject to SECA tax under current law.
Do LLCs pay SECA tax?
Second, limited partners and LLC members who provide services and materially participate in their partnerships and LLCs would be subject to SECA tax on their distributive shares of partnership or LLC income to the extent that this income exceeds certain threshold amounts. The exemptions from SECA tax provided under current law for certain types of partnership income (e.g., rents, dividends, capital gains, and certain retired partner income) would continue to apply to these types of income.
Will Biden change the tax law in 2021?
Summary of Proposed 2021 Federal Tax Law Changes. President Biden has proposed major changes to the Federal tax laws, some of which are sought to be effective earlier in 2021 (i.e., we are already operating under these changes, if they later become adopted), as compared to the effective date the new tax law changes may be passed by Congress ...
Do S corporations pay SECA taxes?
Third, S corporation owners who materially participate in the trade or business would be subject to SECA taxes on their distributive shares of the business’s income to the extent that this income exceeds certain threshold amounts. The exemptions from SECA tax provided under current law for certain types of S corporation income (e.g., rents, dividends, and capital gains) would continue to apply to these types of income.
When does the RMD kick in?
Today, Required Minimum Distributions (RMDs) generally kick in on retirement accounts after age 72 and is based on an IRS provided uniform lifetime distribution number (essentially a life expectancy number) and the value of the account at the end of the prior year. This new provision would apply a new (and much larger) RMD for those with larger accounts and significant taxable income.
What is the RMD for a $16 million IRA?
If the individual’s combined traditional IRA, Roth IRA, and defined contribution retirement account balances exceed $10 million at the end of the prior year, and has taxable income above $400,000 for single filers and $450,000 for married filing jointly, then there would be a new RMD that is generally 50 percent of the aggregate amount above $10 million. So if you had $16 million, you would have a $3 million RMD since 50 percent of the $6 million over $10 million is $3 million.
How does the marriage penalty affect retirement?
This marriage penalty would impact retirement planning in two different ways: first, married couples might just end up with less savings after tax than if they were single filers – allowing less money to be saved for retirement. Second, because many married couples will be more likely to fall into the highest tax rates versus single filers, there is more of an incentive for higher income married filers to save as much as possible in tax-deductible retirement accounts, like a 401 (k), to reduce their tax liability and save for retirement.
