How much Medicare pays hospitals?
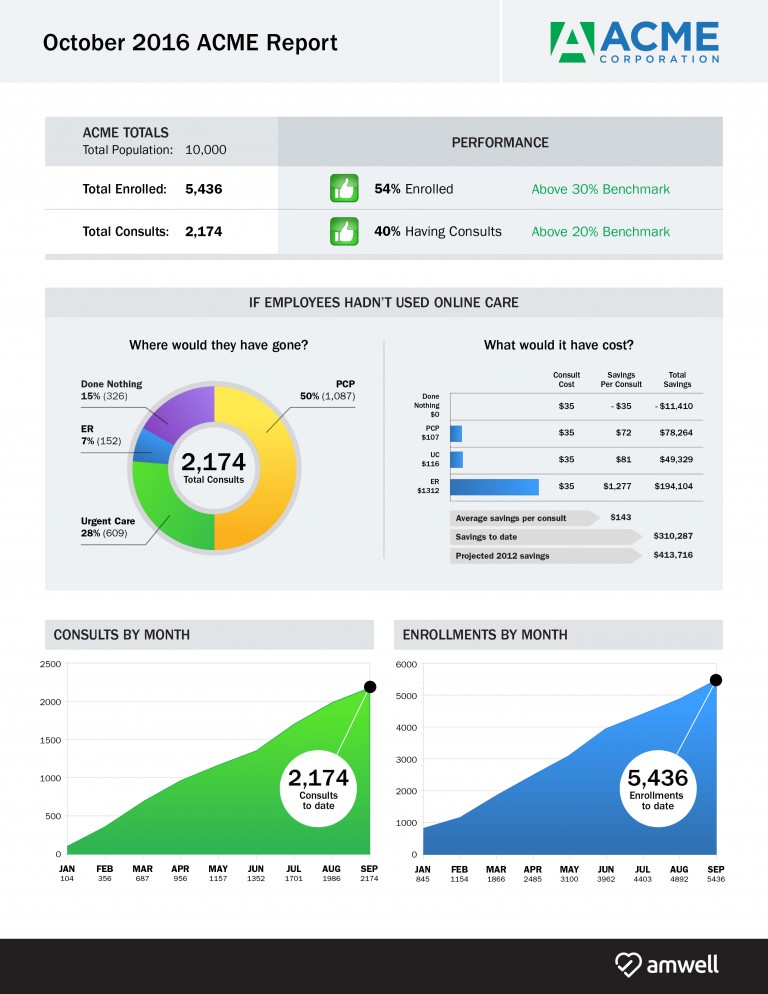
How Does Medicare Insurance Pay Hospitals? Medicare payment systems have evolved over the past few decades, but they continue to use a pay-per-service payment model. This is known as the Inpatient Prospective Payment System, or IPPS. This …
How does Medicare reimburse hospitals?
Mar 23, 2020 · Reimbursement is based on the DRGs and procedures that were assigned and performed during the patient’s hospital stay. Each DRG is assigned a cost based on the average cost based on previous visits. This assigned cost provides a simple method for Medicare to reimburse hospitals as it is only a simple flat rate based on the services provided.
How does Medicare rate hospitals and nursing homes?
The New York Times has a simplified explanation of this highly complicated process. It's simple really. First the hospital labor component is adjusted for geographic location and then added to the capital depreciation expenditures adjusted for geographic location and then a medical severity adjusted diagnosis related group multiplier is added (MS-DRG).
How long will Medicare pay for a hospital stay?
Mar 20, 2015 · Inpatient hospitals (acute care): Medicare pays hospitals per beneficiary discharge, using the Inpatient Prospective Payment System. The base rate for each discharge corresponds to one of over 700...
Does Medicare pay 100 percent of hospital bills?
Most medically necessary inpatient care is covered by Medicare Part A. If you have a covered hospital stay, hospice stay, or short-term stay in a skilled nursing facility, Medicare Part A pays 100% of allowable charges for the first 60 days after you meet your Part A deductible.
Do hospitals benefit from Medicare?
Medicare helps cover certain medical services and supplies in hospitals. If you have both Medicare Part A (Hospital Insurance) and Medicare Part B (Medical Insurance), you can get the full range of Medicare-covered services in a hospital.
Where does the money for a hospital come from?
Financing for hospital services comes from a multitude of private insurers as well as the joint federal-state Medicaid program, the federal Medicare program, and out-of-pocket costs paid by insured and uninsured people.
What percent of hospital revenue is from Medicare?
The percentage of the total payor mix from private/self-pay increased from 66.5% in 2018 to 67.4% in 2020. The Medicare percentage decreased from 21.8% to 20.5%. These shifts likely reflect some of the delays in care throughout the COVID-19 pandemic.
How much does Medicare Part A pay for hospitalization?
Part A – Hospital Insurance Premiums, Deductibles & CoinsuranceIf You HaveIn 2022, You Will Pay a Monthly Premium ofInpatient Hospital Deductible$1,556Inpatient Hospital Coinsurance$389 per day for days 61–90 $778 per day for days 91-150Skilled Nursing Facility Coinsurance$194.50 per day for days 21-1003 more rows
How Long Does Medicare pay for hospital stay?
90 daysMedicare covers a hospital stay of up to 90 days, though a person may still need to pay coinsurance during this time. While Medicare does help fund longer stays, it may take the extra time from an individual's reserve days. Medicare provides 60 lifetime reserve days.May 29, 2020
Do hospitals lose money on Medicare patients?
Those hospitals, which include some of the nation's marquee medical centers, will lose 1% of their Medicare payments over 12 months. The penalties, based on patients who stayed in the hospitals anytime between mid-2017 and 2019, before the pandemic, are not related to covid-19.Feb 19, 2021
Why do hospitals charge so much?
Hospitals say that additional fee helps cover the cost of operations, but consumer advocates say the charges can run into the hundreds of dollars. Buying up doctors' offices can also be very lucrative for large hospitals because those doctors then refer their patients back to the hospital for lab tests and procedures.Sep 7, 2021
What part of the hospital makes the most money?
The Top 10 Revenue-Driving Specialties for HospitalsCardiovascular Surgery. Average revenue: $3.7 million (first year this specialty has been included in the survey) ... Cardiology (Invasive) ... Neurosurgery. ... Orthopedic Surgery. ... Gastroenterology. ... Hematology/Oncology. ... General Surgery. ... Internal Medicine.More items...•Sep 8, 2020
Who is the largest payer in healthcare?
The Centers for Medicare & Medicaid Services (CMS) is the single largest payer for health care in the United States. Nearly 90 million Americans rely on health care benefits through Medicare, Medicaid, and the State Children's Health Insurance Program (SCHIP).
Is Medicare funded by the federal government?
As a federal program, Medicare relies on the federal government for nearly all of its funding. Medicaid is a joint state and federal program that provides health care coverage to beneficiaries with very low incomes.Mar 23, 2022
Why is US healthcare so expensive?
The price of medical care is the single biggest factor behind U.S. healthcare costs, accounting for 90% of spending. These expenditures reflect the cost of caring for those with chronic or long-term medical conditions, an aging population and the increased cost of new medicines, procedures and technologies.
How much does Medicare reimburse?
In addition, Medicare will only reimburse patients for 95 percent of the Medicare approved amount. This means that the patient may be required to pay up to 20 percent extra in addition to their standard deductible, copayments, coinsurance payments, and premium payments.
What is Medicare reimbursement based on?
Reimbursement is based on the DRGs and procedures that were assigned and performed during the patient’s hospital stay. Each DRG is assigned a cost based on the average cost based on previous visits. This assigned cost provides a simple method for Medicare to reimburse hospitals as it is only a simple flat rate based on the services provided.
What is Medicare Part A?
What Medicare Benefits Cover Hospital Expenses? Medicare Part A is responsible for covering hospital expenses when a Medicare recipient is formally admitted. Part A may include coverage for inpatient surgeries, recovery from surgery, multi-day hospital stays due to illness or injury, or other inpatient procedures.
Does Medicare cover hospital care?
Medicare recipients can receive care at a variety of facilities, and hospitals are commonly used for emergency care , inpatient procedures, and longer hospital stays. Medicare benefits often cover care at these facilities through Medicare Part A, and Medicare reimbursement for these services varies. Billing is based on the provider’s relationship ...
What Does DRG Mean?
DRG stands for diagnosis-related group. Medicare's DRG system is called the Medicare severity diagnosis-related group, or MS-DRG, which is used to determine hospital payments under the inpatient prospective payment system (IPPS).
Figuring Out How Much Money a Hospital Gets Paid for a Given DRG
In order to figure out how much a hospital gets paid for any particular hospitalization, you must first know what DRG was assigned for that hospitalization.
Are Hospitals Making or Losing Money?
After the MS-DRG system was implemented in 2008, Medicare determined that hospitals' based payment rates had increased by 5.4% as a result of improved coding (i.e., not as a result of anything having to do with the severity of patients' medical issues).
What is the SGR for Medicare?
Under current law, Medicare’s physician fee-schedule payments are subject to a formula, called the Sustainable Growth Rate (SGR) system, enacted in 1987 as a tool to control spending. For more than a decade this formula has called for cuts in physician payments, reaching as high as 24 percent.
Does Medicare have a fee for service?
Current payment systems in traditional Medicare have evolved over the last several decades, but have maintained a fee-for-service payment structure for most types of providers. In many cases, private insurers have modeled their payment systems on traditional Medicare, including those used for hospitals and physicians.
The claim: Hospitals get paid more if patients are listed as COVID-19, and on ventilators
Sen. Scott Jensen, R-Minn., a physician in Minnesota, was interviewed by "The Ingraham Angle" host Laura Ingraham on April 8 on Fox News and claimed hospitals get paid more if Medicare patients are listed as having COVID-19 and get three times as much money if they need a ventilator.
Provision in the relief act
The coronavirus relief legislation created a 20% premium, or add-on, for COVID-19 Medicare patients.
How does Medicare pay?
Snopes investigated the claim, finding it's plausible Medicare pays in the range Jensen mentions but doesn't have a "one-size-fits-all" payment to hospitals for COVID-19 patients.
Our ruling: True
We rate the claim that hospitals get paid more if patients are listed as COVID-19 and on ventilators as TRUE.
What are the emotions that patients experience in the hospital?
Patients often experience a myriad of emotions when they enter the hospital, including anxiety, vulnerability, and fear. To help ease their patients’ concerns and create a positive, nurturing environment, healthcare professionals must strive to create a strong, respectful connection with their patients by:
How does noise affect hospital patients?
Loud noises and bright lights in particular may negatively affect their sleep and anxiety levels, disrupting the healing process.
What is the best way to manage pain?
Once they have identified their patient’s pain level, healthcare professionals must determine how best to manage it. Administering medication, repositioning the patient, or providing a cold compress are just a few of the many pain management techniques a healthcare professional can deploy.
Is healthcare a consumer driven industry?
By Katherine Detwiler and Natalie Vaughn, MBA, on September 11, 2020. There’s no question about it—healthcare is quickly becoming a consumer-driven industry. As a result, healthcare facilities must now compete with one another to gain new patients and maintain their loyalty. For many of these institutions, that means earning high patient ...
