Can I enroll in Medicare Part D online?
Can you add Medicare Part D at any time?
How long does it take to enroll in Medicare Part D?
Can you buy Medicare Part D by itself?
Is Part D deducted from Social Security?
Is GoodRx better than Medicare Part D?
Who is eligible for Medicare Part D?
Do I need Medicare Part D if I don't take any drugs?
What is the main problem with Medicare Part D?
What is the most popular Medicare Part D plan?
| Rank | Medicare Part D provider | Medicare star rating for Part D plans |
|---|---|---|
| 1 | Kaiser Permanente | 4.9 |
| 2 | UnitedHealthcare (AARP) | 3.9 |
| 3 | BlueCross BlueShield (Anthem) | 3.9 |
| 4 | Humana | 3.8 |
What drugs are not covered by Medicare Part D?
- Drugs used to treat anorexia, weight loss, or weight gain. ...
- Fertility drugs.
- Drugs used for cosmetic purposes or hair growth. ...
- Drugs that are only for the relief of cold or cough symptoms.
- Drugs used to treat erectile dysfunction.
How does Part D Medicare work?
What is Medicare Part D enrollment?
Medicare Part D enrollment is the first step in getting the coverage you need for your prescription medications. With multiple plans to choose from, it is helpful to compare plans carefully to find the right plan for you. You can start by entering your zip code on this page.
How long can you go without Medicare Part D?
However, if you go without Medicare Part D or other creditable prescription drug coverage for a continuous period of 63 days or longer after your IEP is over, you could be subject to a Part D late enrollment penalty. Coverage could come from a stand-alone prescription drug plan, a Medicare Advantage plan with prescription drug coverage (Part C), ...
What is Medicare Advantage Plan?
A Medicare Advantage plan is an alternative way to get your Original Medicare (Part A and Part B) benefits. These plans might also offer coverage for additional services like routine vision or dental care, and prescription medications.
How much is Part D late enrollment penalty?
The amount of the Part D late enrollment penalty depends on how long you went without prescription drug coverage. Medicare calculates the amount by multiplying the number of months you didn’t have prescription drug coverage by 1% of the national base beneficiary premium. In 2021, the national base beneficiary premium is $33.06.
How long can you go without prescription drug coverage?
You can avoid this penalty by ensuring you don’t go without creditable prescription drug coverage for 63 days or longer .
What is a SEP in Medicare?
Special Enrollment Periods or SEPs offer the chance for Medicare Part D enrollment when certain events happen in your life. Those events might include changing where you live or losing your current coverage. If your current plan changes its contract with Medicare or you have an opportunity to get other coverage, you might also qualify for an SEP.
What is Medicare Part D?
Medicare Part D enrollment provides you with choices of plans in most service areas. All plans are required by Medicare to offer a standard level of coverage. Some plans may offer additional benefits beyond this standard. The cost of plans may include monthly premiums, deductibles, copayments, and coinsurance.
How long does a SEP last?
Typically a SEP lasts for 63 days.
What do you need to know before enrolling in a Part D plan?
The most important preparation you can do before finding a Part D plan is recording information about your medications.
How does dosage affect Part D?
Your dosage can affect your final cost or enact certain plan restrictions depending on the Part D plan. The frequency of the medication. The number of pills you take also affects the cost, so double check how often you take your medication and write it down. Once you have these recorded, you’ll be able to compare plans, apples-to-apples.
How long does it take to reply to a 401(k) plan?
Once you’ve applied, the plan has 10 calendar days to reply in one of three ways:
When is the best time to sign up for Part D?
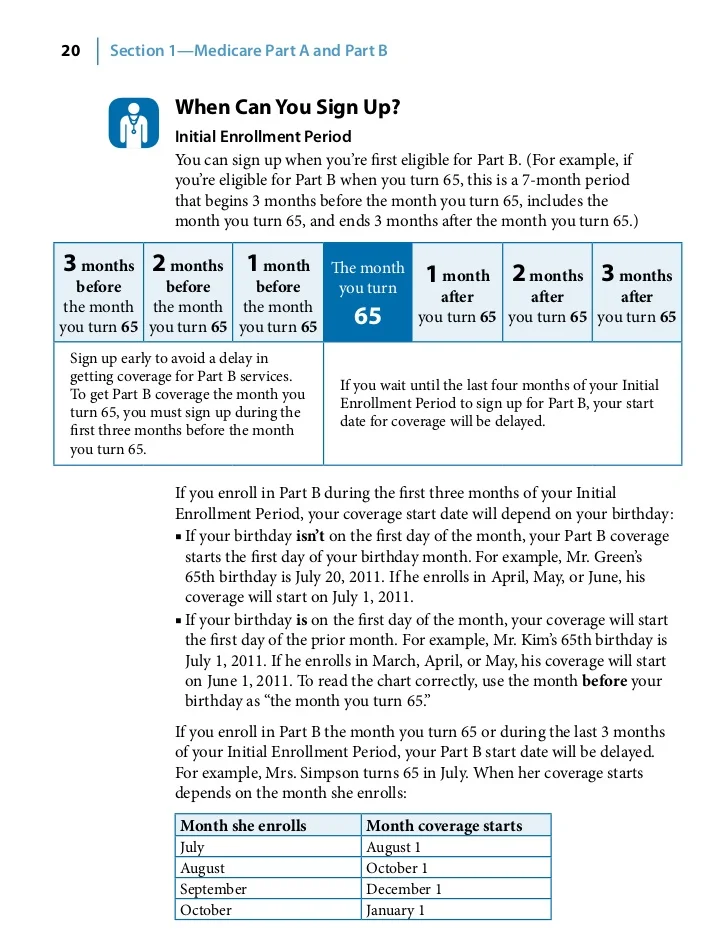
If you don’t have creditable drug coverage or health insurance from a current employer, the best time to sign up for Part D is during your 7-month initial enrollment period (IEP) to avoid penalties. Under your IEP, you have a 7-month window that opens 3 months before you turn 65 and closes at the end of the 3rd month following your birthday month.
Is Medicare Part D a good program?
Although Medicare is not without its faults, one thing is clear: Medicare Part D has been a successful program. With nearly 70% of all beneficiaries enrolled in Part D, this optional add-on to Original Medicare is a popular way to lower drug costs. 1. But before diving into the deep end of Part D plans, you’ll want to perform due diligence ...
Is eligibility.com a DBA?
Content on this site has not been reviewed or endorsed by the Centers for Medicare & Medicaid Services, the United States Government, any state Medicare agency, or any private insurance agency (collectively "Medicare System Providers"). Eligibility.com is a DBA of Clear Link Technologies, LLC and is not affiliated with any Medicare System Providers.
How long before Medicare card is sent out?
We’ll mail you a welcome package with your Medicare card 3 months before your Medicare coverage starts.
How to contact railroad retirement board?
If you or your spouse worked for a railroad, call the Railroad Retirement Board at 1-877-772-5772.
How long do you have to sign up for Part A?
You get Part A automatically. If you want Part B, you need to sign up for it. If you don’t sign up for Part B within 3 months of turning 65, you might have to wait to sign up and pay a monthly late enrollment penalty.
How long after you sign up for Part A do you have to sign up for Part B?
You get Part A automatically. If you want Part B, you need to sign up for it. If you don’t sign up for Part B within 3 months after your Part A starts, you might have to wait to sign up and pay a monthly late enrollment penalty.
What is a.gov website?
A .gov website belongs to an official government organization in the United States.
Can you voluntarily terminate Medicare Part B?
Voluntary Termination of Medicare Part B. You can voluntarily terminate your Medicare Part B (medical insurance). It is a serious decision. You must submit Form CMS-1763 ( PDF, Download Adobe Reader) to the Social Security Administration (SSA). Visit or call the SSA ( 1-800-772-1213) to get this form.
Does Medicare cover travel?
If you have Original Medicare and have a Medigap policy, it may provide coverage for foreign travel emergency health care. Learn more about Original Medicare outside the United States.
How to become a Medicare provider?
Become a Medicare Provider or Supplier 1 You’re a DMEPOS supplier. DMEPOS suppliers should follow the instructions on the Enroll as a DMEPOS Supplier page. 2 You’re an institutional provider. If you’re enrolling a hospital, critical care facility, skilled nursing facility, home health agency, hospice, or other similar institution, you should use the Medicare Enrollment Guide for Institutional Providers.
How to get an NPI?
If you already have an NPI, skip this step and proceed to Step 2. NPIs are issued through the National Plan & Provider Enumeration System (NPPES). You can apply for an NPI on the NPPES website.
How long does it take to change your Medicare billing?
To avoid having your Medicare billing privileges revoked, be sure to report the following changes within 30 days: a change in ownership. an adverse legal action. a change in practice location. You must report all other changes within 90 days. If you applied online, you can keep your information up to date in PECOS.
What can a Mac do?
Your MAC can help you navigate the enrollment process and answer questions about your application. Contact your MAC (PDF).
Can you bill Medicare for your services?
You’re a health care provider who wants to bill Medicare for your services and also have the ability to order and certify. You don’t want to bill Medicare for your services, but you do want enroll in Medicare solely to order and certify.
Do you need to be accredited to participate in CMS surveys?
ii If your institution has obtained accreditation from a CMS-approved accreditation organization, you will not need to participate in State Survey Agency surveys. You must inform the State Survey Agency that your institution is accredited. Accreditation is voluntary; CMS doesn’t require it for Medicare enrollment.