How to find doctors who accept your Medicare Advantage plan?
- Your plan may pay less toward your care. ...
- The fees for health services may be higher. ...
- Any amount you pay might not contribute to your plan deductible, if you have one.
- You may need preauthorization for any services you receive in order for any coverage to apply.
Who offers Medicare Advantage plans?
The ratings are meant to encourage quality and help prospective enrollees choose between different plans. "Our goals for Medicare Advantage mirror our vision ... and we may publish it in print. MH magazine offers content that sheds light on healthcare ...
What are the requirements for Medicare Advantage plan?
When can I enroll in a Part C plan?
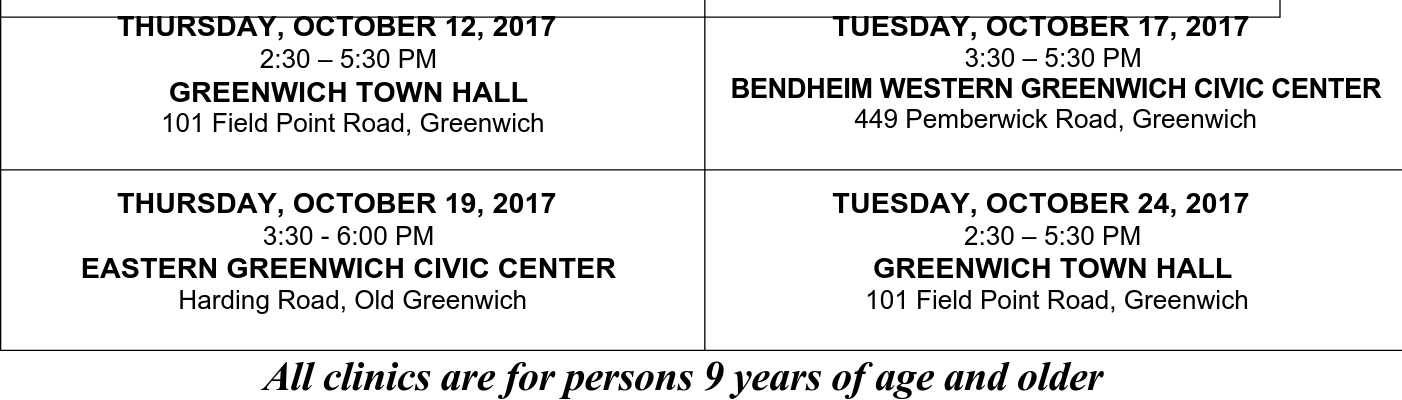
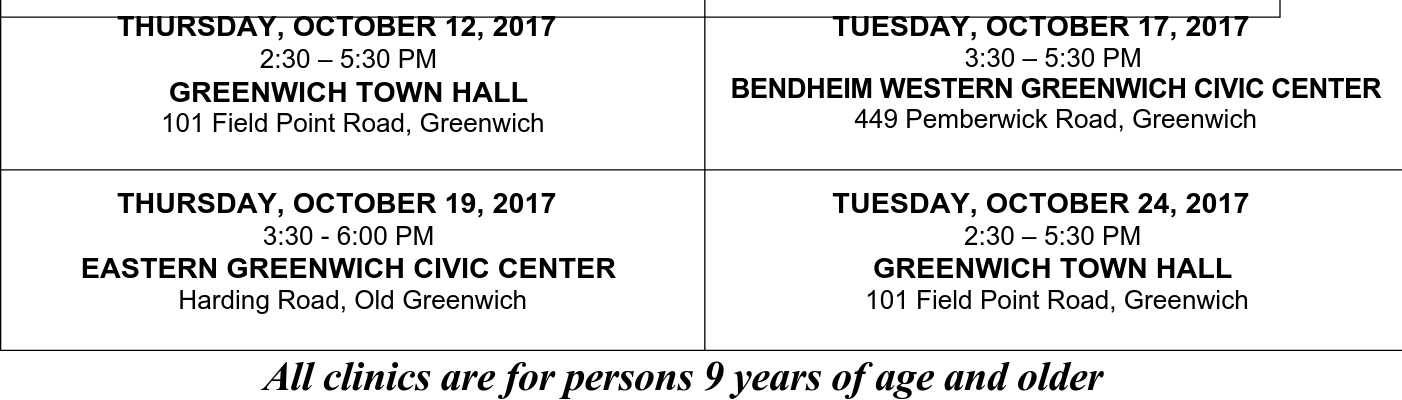
- Initial Enrollment Period (IEP)
- Annual Enrollment Period (AEP)
- Special Enrollment Period (SEP)
Why Advantage plans are bad?
disadvantage of medicare advantage plans
- Networks
- Referrals
- Prior Authorizations
- Frequent Expenses
- Out-of-Pocket Maximums
- Plan Changes
- Medicare is no longer managing your healthcare
Are Medicare Advantage plans profitable for insurance companies?
Medicare Advantage is the common thread. Big-name health insurers raked in $8.2 billion in profit for the fourth quarter of 2019 and $35.7 billion over the course of the year.
Who is the largest provider of Medicare Advantage plans?
UnitedHealthcareStandout feature: UnitedHealthcare offers the largest Medicare Advantage network of all companies, with more than 1 million network care providers.
What agency provides oversight for Medicare Advantage products?
The Centers for Medicare & Medicaid Services (CMS) is the agency within the Department of Health and Human Services (HHS) responsible for overseeing the Medicare Advantage (MA) program—Medicare's private plan alternative.
Does CMS oversee Medicare Advantage plans?
The Federal Center for Medicare Services (CMS) regulates Medicare Advantage plans.
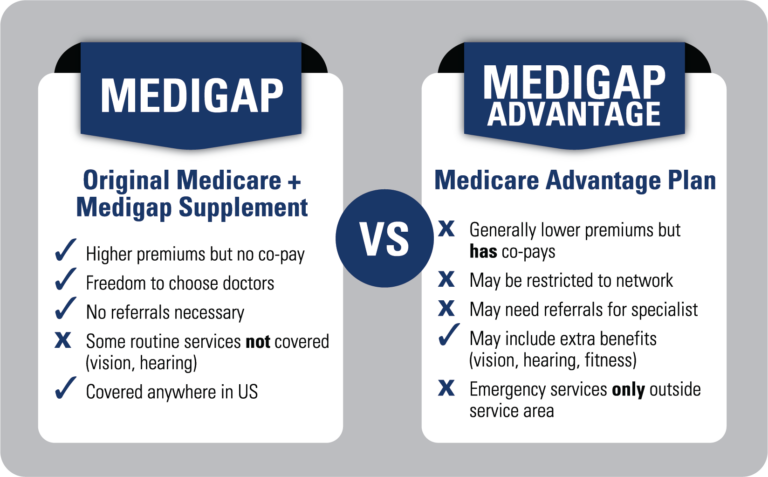
What is the biggest disadvantage of Medicare Advantage?
Medicare Advantage can become expensive if you're sick, due to uncovered copays. Additionally, a plan may offer only a limited network of doctors, which can interfere with a patient's choice. It's not easy to change to another plan. If you decide to switch to a Medigap policy, there often are lifetime penalties.
What are 4 types of Medicare Advantage plans?
Below are the most common types of Medicare Advantage Plans.Health Maintenance Organization (HMO) Plans.Preferred Provider Organization (PPO) Plans.Private Fee-for-Service (PFFS) Plans.Special Needs Plans (SNPs)
What does it mean to be CMS certified?
Certification is when the State Survey Agency officially recommends its findings regarding whether health care entities meet the Social Security Act's provider or supplier definitions, and whether the entities comply with standards required by Federal regulations.
What does CMS mean in Medicare?
Centers for Medicare & Medicaid ServicesHome - Centers for Medicare & Medicaid Services. CMS.
Who is in charge of CMS?
The Centers for Medicare & Medicaid Services, CMS, is part of the Department of Health and Human Services (HHS).
Why do doctors not like Medicare Advantage plans?
If they don't say under budget, they end up losing money. Meaning, you may not receive the full extent of care. Thus, many doctors will likely tell you they do not like Medicare Advantage plans because private insurance companies make it difficult for them to get paid for their services.
Who audits Medicare Advantage plans?
the OIG"The Company expects [the Centers for Medicare & Medicaid Services] and the OIG to continue these types of audits," CVS said in the filing. Earlier this year, the feds said a Florida Humana plan overcharged Medicare by more than $200 million, the largest audit penalty ever posed on an MA plan.
What is a downstream provider?
downstream provider means an entity or individual that is contracted by a First Tier Entity to provide services to Enrollees. A Downstream Provider includes, but is not limited to physicians, ancillary providers, and other health care providers.
How do costs differ for providers of Medicare Advantage plans?
One essential difference between Original Medicare and Medicare Advantage is that Medicare Advantage plans are offered by private insurance companies approved by Medicare. This means they are free to set their own premiums and cost structures.
How do benefits differ for providers of Medicare Advantage plans?
Most Medicare Advantage plans include Part D coverage for prescription drugs, although some do not. You may also get discounts or an allowance toward over-the-counter medications with some Medicare Advantage plans.
Are there any other differences between providers of Medicare Advantage plans?
There are several types of Medicare Advantage plans, but the most common are managed care plans, either health maintenance organizations (HMOs) and preferred provider organizations (PPOs*). These plans use provider networks to help keep costs low for their members.
Would you like more information about Medicare Advantage plans?
I am happy to help you find the information you need; you can schedule a phone call or request an email by clicking on the buttons below. You can also find out about Medicare plan options in your area by clicking the Compare Plans button.
When does Medicare Advantage plan include OTP?
Medicare Advantage Plans. Medicare Advantage (MA) plans must include the OTP benefit as of January 1, 2020 and contract with OTP providers in their service area, or agree to pay an OTP on a non-contract basis.
What should an OTP do with a MA plan?
OTPs should contact MA plans and ask for “provider services” to help with questions about payment for OTP services under that MA plan. If you’re not sure if your Medicare patient is enrolled in an MA plan:
Does MA have to use Medicare OTP?
In covering the OTP benefit, MA plans must use only Medicare-enrolled OTP providers. Regardless of whether an OTP is under contract with an MA plan or rendering services on a non-contract basis, the OTP must contact each specific plan with payment questions.