Can you put 01968 and 01967 on the same card?
Are you putting them on the same date of service since the 01968 is an add on code or can you have the 01967 on the day it was given and then use 01968 on the next day? Thanks I code 01967 for the epidural and 01968 on a separate card for failure to progress if an emergency c-sec is done.
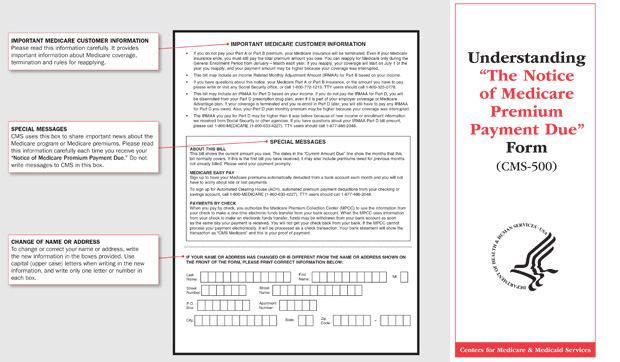
How do I Pay my Medicare bill online?
Sign up for Medicare Easy Pay. Check if your bank offers an online bill payment service to pay electronically from your savings or checking account. Mail your payment by check, money order, credit card, or debit card (using the coupon on your bill) Get details about these payment options.
How do I file a Medicare claim?
Submit your completed Patients Request for Medical Payment form, itemized medical bill or bills, and any supporting documents to your states Medicare contractor. All claims must be submitted by mail you cant file a Medicare claim online.
How do I get Medicare to give my personal health information?
You need to fill out an " Authorization to Disclose Personal Health Information " if you want someone to be able to call 1-800-MEDICARE on your behalf or you want Medicare to give your personal information to someone other than you. Get this form in Spanish. Find out who to call about Medicare options, claims and more.

How do I bill anesthesia claims to Medicare?
The following policies reflect national Medicare correct coding guidelines for anesthesia services. 1. CPT codes 00100-01860 specify “Anesthesia for” followed by a description of a surgical intervention.
What is procedure code 01967?
01967 - epidural insertion for labor and vaginal delivery. 01968 - anesthesia for cesarean delivery following labor analgesia. 01969 - anesthesia for cesarean hysterectomy following labor analgesia.
How does Medicare reimburse CRNA?
The Medicare program pays the CRNA 80% of this allowable charge (non-medically directed). Deductible and coinsurance apply. If the CRNA is medically directed, pay 50% of the allowable charge.
Can 01967 and 01968 be billed together?
In the obstetrical area, code 01968 (2 base units) is used in conjunction with code 01967 (5 base units); code 01969 (5 base units) is used in conjunction with code 01967 (5 base units).
What modifier is used for medically directed CRNA services?
The “QX” modifier identifies the CRNA service under medical direction by a physician.
What is an AA modifier?
HCPCS Modifier AA — anesthesia Services performed personally by the anesthesiologist. Guidelines and Instructions. This modifier may only be submitted with anesthesia procedure codes (e.g., CPT codes 00100 through 01999)
Can anesthesiologist and CRNA bill for the same procedure?
There is a maximum allowable for both Certified Registered Nurse Anesthetist (CRNA) and Physician Anesthesiologists when they bill for the same service. Anesthesia is covered for both medically directed and non-medically directed CRNA services.
How are anesthesia services reimbursed?
Time-based anesthesia services are reimbursed according to the following formulas: Standard Anesthesia Formula without Modifier AD* = ([Base Unit Value + Time Units + Modifying Units] x Conversion Factor) x Modifier Percentage.
Why is anesthesia billed separately?
Why did I receive more than one bill for anesthesia care? Anesthesiologists typically are not employees of the care facility and bill separately for their services. CRNAs can bill separately for their services and may be employed independent of the care facility or the anesthesiologist.
What are the three classifications of anesthesia?
There are three types of anesthesia: general, regional, and local. Sometimes, a patient gets more than one type of anesthesia. The type(s) of anesthesia used depends on the surgery or procedure being done and the age and medical conditions of the patient.
How do you calculate anesthesia units?
Time units are computed by dividing the reported anesthesia time by 15 minutes (17 minutes / 15 minutes = 1.13 units).
What is neuraxial labor analgesia?
Neuraxial analgesia is the preferred method of providing analgesia for labor and vaginal delivery. If needed, the epidural catheter will usually provide anesthesia for cesarean section and other surgical procedures related to pregnancy.
How much is Medicare reimbursement for 2020?
Reimbursements match similar in-person services, increasing from about $14-$41 to about $60-$137, retroactive to March 1, 2020. In addition, Medicare is temporarily waiving the audio-video requirement for many telehealth services during the COVID-19 public health emergency. Codes that have audio-only waivers during the public health emergency are ...
What is the CPT code for Telehealth?
Medicare increased payments for certain evaluation and management visits provided by phone for the duration of the COVID-19 public health emergency: Telehealth CPT codes 99441 (5-10 minutes), 99442 (11-20 minutes), and 99443 (20-30 minutes)
Does Medicare cover telehealth?
Telehealth codes covered by Medicare. Medicare added over one hundred CPT and HCPCS codes to the telehealth services list for the duration of the COVID-19 public health emergency. Telehealth visits billed to Medicare are paid at the same Medicare Fee-for-Service (FFS) rate as an in-person visit during the COVID-19 public health emergency.
What Information Do You Need To Fill Out This Form
Medicare will need you to fill out a patient request form with some basic information about yourself as well as the service or medical item you are filing about. Youll need to provide:
Find Cheap Medicare Plans In Your Area
Medicare reimbursement is the process by which a doctor or health facility receives funds for providing medical services to a Medicare beneficiary. However, Medicare enrollees may also need to file claims for reimbursement if they receive care from a provider that does not accept assignment.
Medicare Claims And Reimbursement
In most cases, you wont have to worry about filing Medicare claims. Here are some situations where you might or might not need to get involved in the claim process.
What Do I Do If My Doctor Does Not Accept Medicare
You can choose to stay and cover the costs out-of-pocket, but this is not an affordable option for most Americans. Instead, you can ask your doctor for a referral to another healthcare provider that does accept Medicare, do your own research, or visit an urgent care facility. Most urgent care offices accept Medicare.
How Long Do I Have To File A Claim
Original Medicare claims have to be submitted within 12 months of when you received care. Medicare Advantage plans have different time limits for when you have to submit claims, and these time limits are shorter than Original Medicare. Contact your Advantage plan to find out its time limit for submitting claims.
You Should Only Need To File A Claim In Very Rare Cases
Medicare claims must be filed no later than 12 months after the date when the services were provided. If a claim isn’t filed within this time limit, Medicare can’t pay its share. For example, if you see your doctor on March 22, 2019, your doctor must file the Medicare claim for that visit no later than March 22, 2020.
How Do I File A Medicare Claim
Medicare beneficiaries occasionally have to submit their own healthcare claims instead of relying on a provider to submit them. | Photo credit: Helloquence | Unsplash