- Step one - Verify the technical requirements.
- Step two - Enroll for PC-ACE using the EDI Enrollment form.
- Step three - Download the software.
- Step four - Configure the program.
- Step five - Claim entry and transmission.
How do I submit MSP claims to Novitas?
Medicare Secondary Payer (MSP) claims can be submitted electronically to Novitas Solutions via your billing service/clearinghouse, directly through a Secure File Transfer Protocol (SFTP) connection, or via Novitasphere portal's batch claim submission.
How do I Bill my Medicare Advantage patients?
Use your patients’ Medicare Beneficiary Identifiers (MBIs) (not their Medicare Advantage Plan Member IDs) to bill Original Medicare. Ask your Medicare Advantage patients for their Original Medicare card. All Medicare patients have a red, white, and blue Medicare card with an MBI, including those enrolled in a Medicare Advantage Plan.
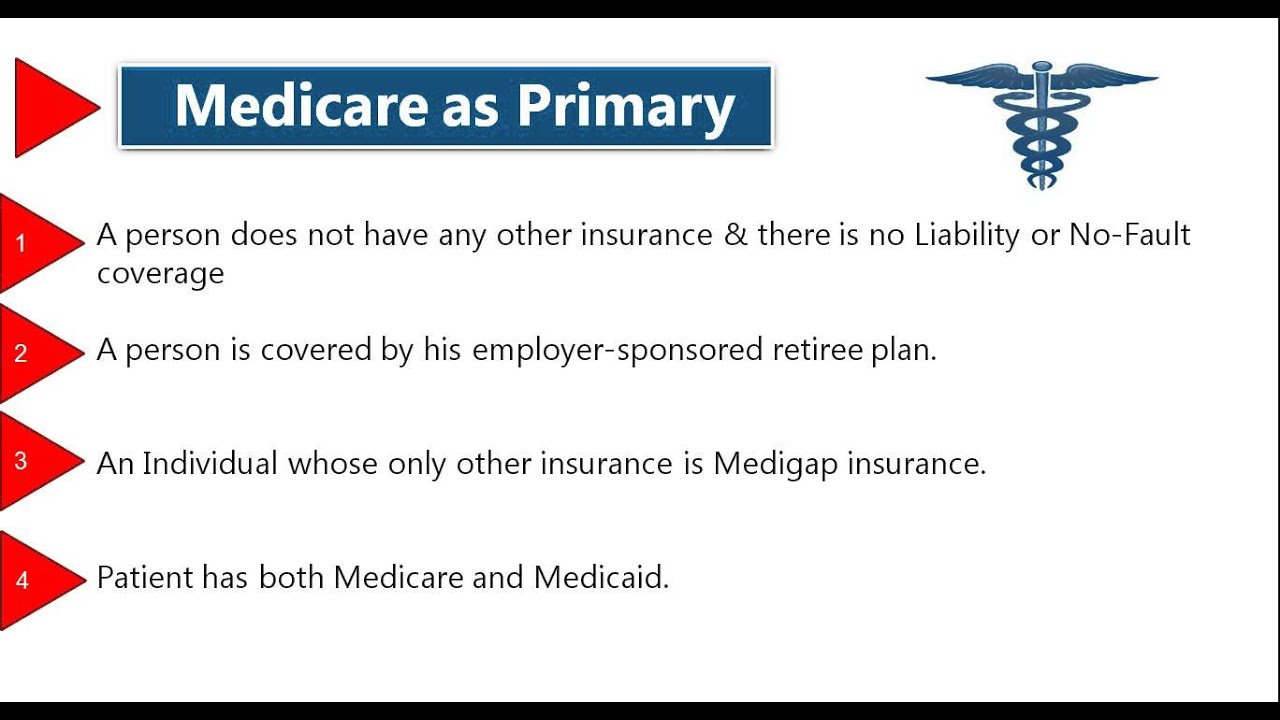
How do I bill Medicare for primary insurance?
It is the provider's responsibility to obtain primary insurance information from the beneficiary and bill Medicare appropriately. When submitting a paper claim to Medicare as the secondary payer, the CMS-1500 (02-12) claim form must indicate the name and policy number of the beneficiary's primary insurance in items 11-11c.
How do I look up the MBI for Medicare patients?
You can look up the MBI for any Medicare patients, including those enrolled in a Medicare Advantage Plan. For Part A and Home Health and Hospice (HHH) claims, include Condition Code (CC) 78. For Medicare Advantage patients you vaccinate on or after January 1, 2022, submit COVID-19 vaccine administration claims to the Medicare Advantage Plan.

Is novitas a Medicare solution?
Novitas Solutions welcomes you to the Medicare Program. We look forward to serving your needs and establishing a rewarding partnership with you. Now that you have joined the growing ranks of Medicare providers, it is important for you to understand the Medicare guidelines and to submit accurate claims.
How do I bill a claim to Medicare?
Contact your doctor or supplier, and ask them to file a claim. If they don't file a claim, call us at 1-800-MEDICARE (1-800-633-4227). TTY: 1-877-486-2048. Ask for the exact time limit for filing a Medicare claim for the service or supply you got.
How do you fill out CMS 1500 when Medicare is secondary?
0:239:21Medicare Secondary Payer (MSP) CMS-1500 Submission - YouTubeYouTubeStart of suggested clipEnd of suggested clipHere when the insured. And the patient are the same the biller enters the word. Same if medicare isMoreHere when the insured. And the patient are the same the biller enters the word. Same if medicare is primary this item is left blank.
How do I submit a Medicare claim electronically?
How to Submit Claims: Claims may be electronically submitted to a Medicare Administrative Contractor (MAC) from a provider using a computer with software that meets electronic filing requirements as established by the HIPAA claim standard and by meeting CMS requirements contained in the provider enrollment & ...
What form is used to send claims to Medicare?
CMS-1500 claim formThe CMS-1500 claim form is used to submit non-institutional claims for health care services provided by physicians, other providers and suppliers to Medicare.
What is the first step in submitting Medicare claims?
The first thing you'll need to do when filing your claim is to fill out the Patient's Request for Medical Payment form. ... The next step in filing your own claim is to get an itemized bill for your medical treatment.More items...•
Does Medicare accept the CMS 1500 claim form?
Medicare will accept any Page 3 type (i.e., single sheet, snap-out, continuous feed, etc.) of the CMS-1500 claim form for processing. To purchase forms from the U.S. Government Printing Office, call (202) 512-1800. The following instructions are required for a Medicare claim.
How do I submit a 1500 claim to Medicare?
CMS-1500 should be submitted with the appropriate resubmission code (value of 7) in Box 22 of the paper claim with the original claim number of the corrected claim. Include a copy of the original Explanation of Payment (EOP) with the original claim number for which the corrected claim is being submitted.
Where do you put none with Medicare as a primary payer claim?
If there is no insurance primary to Medicare, the word "none" should be entered in block 11. Completion of item 11 (i.e., insured's policy/group number or "none") is required on all claims.
What is the electronic payer ID for Medicare?
01112Medicare claim address, phone numbers, payor id – revised listStatePayer IDCaliforniaCA01112ColoradoCO04112ConnecticutCT13102DelawareDE1210246 more rows
Where do I send Medicare claim form?
Send the completed form to the Department of Human Services, GPO Box 9822 in your capital city or place in the 'drop box' at one of our Service Centres.
What is the difference between paper claims and electronic claims?
Paper claims that are almost obsolete are still used by certain payers. To send out paper claims, billers will have to enter claim details in the forms provided by insurance companies and send the completed details across. In contrast electronic claims are created and sent to clearinghouses/insurers via their EHRs.
What is CMS unlabeled?
CMS provides the national guidelines on the unlabeled use for anti-cancer drugs. An off-label usage of a Food and Drug Administration approved drug will be considered for coverage when there are no specific contraindications and one of the following criteria is met: Its usage is supported by one or more citations in at least one ...
What is a discarded drug?
The discarded drug amount is the amount of a single use vial or other single use package that remains after administering a dose/quantity of the drug to a Medicare beneficiary. Therefore, if no amount of the drug was administered to the patient, then no claim should be submitted.
How does Medicare Part B work?
Medicare Part B claims process through the standard Multi-Carrier System. The standard system uses a series of edits and audits to help determine whether claims are eligible for payment. The standard system has been programmed to reject or deny a claim based on the first edit or audit that it does not pass.
What is the American Medical Association Drug Evaluation?
American Medical Association Drug Evaluations. United States Pharmacopoeia Drug Information. The use is supported by clinical research that appears in peer reviewed medical literature. This applies only when an unlabeled use does not appear in any of the compendia or is listed as insufficient data or investigational.
What is peer reviewed medical literature?
Peer reviewed medical literature includes scientific, medical, and pharmaceutical publications in which original manuscripts are published, only after having been critically reviewed for scientific accuracy, validity, and reliability by unbiased independent experts . This does not include in-house publications of pharmaceutical manufacturing ...
Can A/B MACs increase or decrease payment for a service?
Thus, A/B MACs (B) may increase or decrease the payment for a service only under very unusual circumstances based upon review of medical records and other documentation.”. Reference.
Do you need to document the site of an injection?
The site of the injection should also be documented as well as any patient reactions to the medication and signature of the person administering the medication. Documentation must be maintained in the patient's chart to support the medical necessity of the injection given.
Why is it important to report the correct MSP insurance type?
It is extremely important to report the correct MSP insurance type on a claim to avoid claim rejections. Some examples of incorrect MSP insurance types are:
What is CAS in electronic claims?
The CAS is the section of the file where you report the outcome of the claim.
What is Workers Compensation?
Workers’ Compensation – This is insurance that employers are required to provide employees that become ill or injured on the job. 47. Liability – Insurance (including a self-insured plan) that provides payment based on the policyholder’s alleged legal liability for injury, illness or damage to property.
Is Medicare a secondary payer?
End Stage Renal Disease – This coverage is for beneficiaries enrolled with Medicare solely due to renal failure and are insured their own, or through a family member’s current or former employment. Medicare is secondary payer for the first 30 months. There is no age restriction on this type of coverage.
Can EOBs be sent separately?
The EOB from the primary insurance should not be sent separately and do not use the PWK Segment and form to submit primary payment information or EOBs. Other records may also be necessary depending on the information obtained by the primary insurer.
Who do I contact to submit a paper claim for Medicare?
Providers who are required to bill electronically due to the Administration Simplification Compliance Act (ASCA) must contact the EDI Helpdesk before submitting a paper claim for Medicare as a tertiary payer.
Does Novitas require a test?
Novitas Solutions requires testing to ensure the electronic claim data is accurate, complete, and that the software is compatible with our systems. Providers enrolling in Medicare’s free software or software that is approved for Medicare claims submission are not required to test.
Can Medicare claims be entered directly into the system?
Claims can also be entered directly into the Medicare processing systems by enrolling for Direct Data Entry. Information on the two options for using Direct Data Entry is available in the below sections:
Indian Health Services (IHS), Tribal and Urban Indians
For billing guidance for Indian Health Services, Tribal and Urban Indians please refer to the Indian Health Services COVID-19 vaccine and monoclonal antibody (mAb) infusion administration article.
Federally qualified health centers (FQHCs)
COVID-19 vaccines and their administration will be paid the same way influenza and pneumococcal vaccines and their administration are paid in FQHCs. Influenza and pneumococcal vaccines and their administration are paid at 100 percent of reasonable cost through the cost report.
Rural health clinics (RHCs)
Independent and provider-based RHCs do not include charges for vaccine or administration for COVID-19 or mAb on a claim, reimbursement is made at the time of cost settlement. Claims will process with $0 payment when submitted with only the vaccine and/or administration.
Medicare Advantage beneficiaries to traditional Medicare
CMS provided special guidance for Medicare Advantage plan patients. For 2020 and 2021, submit the vaccine or infusion administration claims for Medicare Advantage plan enrollees to traditional Medicare using the Medicare Beneficiary Identifier (MBI) for processing and payment.
SNFs - enforcement discretion to certain pharmacy billing
In order to facilitate the efficient administration of COVID-19 vaccines and monoclonal antibody treatments to SNF residents, CMS will exercise enforcement discretion with respect to these statutory provisions as well as any associated statutory references and implementing regulations, including as interpreted in pertinent guidance, SNF CB provisions.
General Information
CPT codes, descriptions and other data only are copyright 2020 American Medical Association. All Rights Reserved. Applicable FARS/HHSARS apply.
Article Guidance
This article describes the least restrictive coverage possible. Providers must read the entire NCD and related Internet Only Manual (IOM) sections (see "Sources" at end of this article) in order to correctly understand and apply the following coding guidance.
Bill Type Codes
Contractors may specify Bill Types to help providers identify those Bill Types typically used to report this service. Absence of a Bill Type does not guarantee that the article does not apply to that Bill Type.
Revenue Codes
Contractors may specify Revenue Codes to help providers identify those Revenue Codes typically used to report this service. In most instances Revenue Codes are purely advisory. Unless specified in the article, services reported under other Revenue Codes are equally subject to this coverage determination.
What is the MBI for Medicare?
All Medicare patients have a red, white, and blue Medicare card with an MBI, including those enrolled in a Medicare Advantage Plan. If your patients don’t have their Original Medicare card or don’t know their MBI, use the MBI look-up tool in your MAC’s secure portal (PDF).
What is the POS code for Part B?
When you choose the Place of Service (POS) code for your Part B claims, carefully consider where you provided the vaccine. Roster billers should use POS code 60 regardless of your provider type, even if you’re not a mass immunization roster biller (provider specialty type 73). When the government provides COVID-19 vaccines at no cost, ...
What is the CMS format for billing?
You may use roster billing format or submit individual claims using the CMS-1500 form (PDF) or the 837P electronic format. CMS systems will accept roster bills for 1 or more patients that get the same type of shot on the same date of service.
Can you bill Medicare for additional in home care?
You should only bill for the additional in-home payment amount if the sole purpose of the visit is to administer a COVID-19 vaccine. You shouldn’t bill for the additional amount if you provide and bill Medicare for another service in the same home on the same date.
Do you have to include the code on a claim for a free shot?
Don’t include the vaccine codes on the claim when the vaccines are free. You must administer the vaccine with no out-of-pocket cost to your patients for the vaccine or administration of the vaccine. If you want to administer the vaccine for free, you don’t have to submit a claim to Medicare, Medicaid, or another insurer.