
When can I Change my Medicare plan?
There are many plan changes that Medicare beneficiaries might want to make from one year to the next. For most of them, the applicable open enrollment period is October 15 to December 7, with changes effective on January 1. During that timeframe, you can: Switch from Original Medicare to Medicare Advantage, or vice versa.
How long does it take to see a Medicare claim?
You’ll usually be able to see a claim within 24 hours after Medicare processes it. Check your Medicare Summary Notice (MSN). The MSN is a notice that people with Original Medicare get in the mail every 3 months. It shows: All your Part A and Part B-covered services or supplies billed to Medicare during a 3-month period; What Medicare paid
Do physician Billings have to match the date of service?
Physicians and non-physician practitioners need to identify the correct date of service for the services they provide to a Medicare patient. Most services must be billed to Medicare reflecting the exact date the services were performed for or provided to the patient, with some exceptions.
What happens when a Medicare claim is corrected?
As a Medicare provider, you are accountable to ensure the information you submit on your claim is correct, and according to Medicare regulations. When claims are corrected from the RTP file, a new receipt date is assigned.
How do I correct a DDE claim?
Make your correction and press F9. Repeat this process (F1, F3, F9) until the claim has been corrected, and you are returned to Map 1741. - More than one reason code may appear in the lower left-hand corner of Page 01 of the claim.
How do I retract a Medicare claim?
The fastest way to cancel a claim is to call Medicare at 800-MEDICARE (800-633-4227). Tell the representative you need to cancel a claim you filed yourself. You might get transferred to a specialist or to your state's Medicare claims department.
How long do you have to correct a Medicare claim?
Redeterminations (Appeals) Redetermination requests must be submitted within 120 days of the date on the Remittance Advice (RA). Inappropriate requests for redeterminations: Items not denied due to medical necessity. Clerical errors that can be handled as online adjustments or clerical reopenings.
How do I correct a Medicare billing error?
If the issue is with the hospital or a medical provider, call them and ask to speak with the person who handles insurance. They can help assist you in correcting the billing issue. Those with Original Medicare (parts A and B) can call 1-800-MEDICARE with any billing issues.
What is a claim adjustment?
Claims adjusting is the process of determining coverage, legal liability, and settling a claim. The claim function exists to fulfill the insurer's promises to its policyholders. Claim adjusting is integral to establishing an insurer's relationship to its policyholders.
What is a Medicare adjustment?
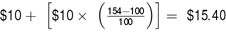
The Medicare system adjusts fee-for-service payment rates for hospitals and practitioners1 according to the geographic location in which providers practice, recognizing that certain costs beyond the providers' control vary between metropolitan and nonmetropolitan areas and also differ by region.
Does Medicare Take corrected claims?
In general, Medicare claims must be filed to the Medicare claims processing contractor no later than 12 months, or 1 calendar year, from the date the services were furnished. This includes resubmitting corrected claims that were unprocessable.
Which date does Medicare consider the date of service?
The date of service for the Certification is the date the physician completes and signs the plan of care. The date of the Recertification is the date the physician completes the review. For more information, see the Medicare Claims Processing Manual, Chapter 12, Section 180.1.
What is the resubmission code for a corrected claim?
7Complete box 22 (Resubmission Code) to include a 7 (the "Replace" billing code) to notify us of a corrected or replacement claim, or insert an 8 (the “Void” billing code) to let us know you are voiding a previously submitted claim.
How do I contact Medicare?
(800) 633-4227Centers for Medicare & Medicaid Services / Customer service
How do I correct a claim on Novitasphere?
Step 1: Access the Claim Correction feature on the left sidebar. Step 2: Access the claim by entering the required fields (marked by a red *) in the Claim Correction screen, and click the Search button. Step 3: Clic k the Reopen Claim for Correction button to perform a Claim Correction.
How do providers check Medicare claim status?
Providers can enter data via the Interactive Voice Response (IVR) telephone systems operated by the MACs. Providers can submit claim status inquiries via the Medicare Administrative Contractors' provider Internet-based portals. Some providers can enter claim status queries via direct data entry screens.
Who needs to identify the correct date of service for the services they provide to a Medicare patient?
This article is applicable to physicians, non-physician practitioners, and others submitting claims for reimbursement for Medicare Part B services. Physicians and non-physician practitioners need to identify the correct date of service for the services they provide to a Medicare patient.
When is non-complex service billed to Medicare?
The non-complex service can be billed to Medicare when the time threshold for the procedure code has been met and documented in the patient’s records. Services would continue as medically necessary throughout the month. The date of the time completion is the date of the service.
What is a CPO in Medicare?
CPO is physician supervision of a patient receiving complex and/or multidisciplinary care as part of Medicare covered services provided by a participating home health agency or Medicare approved hospice. This service provides physician supervision of a patient involving 30 minutes or more providing specified services. The claim for CPO must not include any other services and is only billed after the end of the month in which CPO was provided. The date of service can be the last date of the month or the date in which at least 30 minutes of time is completed.
What is the date of service for a NPP certification?
The date of service for the Certification is the date the physician/non-physician practitioner (NPP) completes and signs the plan of care. The date of the Recertification is the date the physician/NPP completes the review.
Is Medicare incurred on the date of the service?
If you are providing these services, please take advantage of the information available on the Centers for Medicare & Medicaid Services (CMS) website in addition to your Medicare Administrative Contractor’s web portals. Generally , expenses are considered to have been incurred on the date the beneficiary received the item or service, regardless of when it was paid for or ordered. Any exceptions are discussed below.
Do Medicare services have to be billed?
Most services must be billed to Medicare reflecting the exact date the services were performed for or provided to the patient, with some exceptions. This article will discuss some of the situations where there have been questions from the provider community.
What is Medicare 935?
The limitation on recoupment (935), as required by Section 935 of the Medicare Prescription Drug, Improvement, and Modernization Act of 2003 (MMA) changes the process by which CGS can recoup an overpayment resulting from a post payment adjustment , such as a denial or Medicare Secondary Payer (MSP) recovery. For additional information, refer to the Medicare Financial Management Manual, (CMS Pub. 100-06), Ch. 3 §200.
Can you adjust a P claim?
If a claim in a P status has been reviewed by Medical Review and has one or more line items denied, adjustments can be made to the paid line items. Please note: Adjustments cannot be made to any part of a denied line item on a partially paid claim.
When does a provider's fiscal year end?
A fiscal year end can be the end of any quarter — March 31, June 30, September 30, or December 31.
When does a split billing end?
A calendar year is the one-year period that begins on January 1 and ends on December 31. Outpatient split billing is only required for services that span the calendar year end. Outpatient split billing is not required for services that span the provider or federal fiscal year end.
What form is used for HCPCS claim?
All inpatient Part B and outpatient claims require a single line item date of service for each revenue code line reporting a HCPCS reported in form locator (FL) 45 of the uniform bill (UB)-04 claim form or its electronic equivalent.
What is line item date of service?
The line item date of service for the emergency room (ER) service is the date the patient entered the ER, even if it spans multiple service dates.
What is the date of service policy for clinical laboratory test/service?
The date of service policy for clinical laboratory test/service must be the date the specimen was collected.
What happens if a line item date of service is not reported on each revenue code line?
If a line item date of service is not reported on each revenue code line, or the line item dates of service reported are outside the statement-covers period, your claim will be returned.
How long was the patient in the ER on 12/31/2017?
The patient was seen in the ER on 12/31/2017, was placed in observation on 12/31/2017 for 32 hours and discharged home on 1/1/2021. Submit the claims as follows:
When does the fiscal year end?
A fiscal year end can be the end of any quarter — March 31, June 30, September 30, or December 31. The federal fiscal year is the 12-month period ending on September 30 of that year, having begun October 1 of the previous calendar year. A calendar year is the one-year period that begins on January 1 and ends on December 31.
How many months does an inpatient hospital stay in fiscal year?
There are times when an inpatient admission may cross over the provider’s fiscal year end, the federal fiscal year end or calendar year end. The fiscal year is any 12 consecutive months chosen to be the official accounting period by a business or organization.
What is the statement cover period?
Each inpatient claim contains the Statement Covers Period ('From' and 'Through' dates) to identify the span of service dates included in a particular bill.
When does a calendar year end?
A calendar year is the one-year period that begins on January 1 and ends on December 31. The following chart provides guidance on when to split a claim by provider specialty or by federal fiscal year or calendar year in these situations. Provider Type. Provider Fiscal Year End. Federal Fiscal Year End.
Is discharge counted as a day?
Note: Date of discharge not counted as a day, thus the reason for submitting a no-pay bill.
What is the responsibility of Medicare providers to ensure the information submitted on your billing transactions (claims, adjustments, and cancel?
Note:It is the responsibility of Medicare providers to ensure the information submitted on your billing transactions (claims, adjustments, and cancels) are correct, and according to Medicare regulations. CGS is required by the Centers for Medicare & Medicaid Services (CMS) to monitor claim submission errors through data analysis, and action may be taken when providers exhibit a pattern of submitting claims inappropriately, incorrectly or erroneously. Providers should be aware that a referral to the Office of Inspector General (OIG) may be made for Medicare fraud or abuse when a pattern of submitting claims inappropriately, incorrectly, or erroneously is identified.
How long does a claim stay in status after being suppressed?
After suppressing the view of a claim, it will no longer display in the RTP file; however, when viewing the Claim Inquiry (option 12) or Claim Count Summary (option 56) screens, the claim may still appear in status/location T B9997 for several weeks, until FISS purges suppressed claims to the “I” status.
What happens when a claim is submitted to the FISS?
When a claim is submitted into the FISS, it processes through a series of edits to ensure the information submitted on the claim is complete and correct. If the claim has incomplete, incorrect or missing information, it will be sent to your Return to Provider (RTP) file for you to correct. Claims in the RTP file receive a new date of receipt when they are corrected (F9’d) and are subject to the Medicare timely claim filing requirements. See the “Note” on page 7 of this chapter for additional information on Medicare timely filing guidelines.
How long is a claim in RTP?
NOTE: Claims are available in your RTP file for up to 36 months (see the “Note” below regarding timely filing). After 36 months, the claim will purge off of FISS. If you choose not to correct the claim in RTP, we strongly encourage you to suppress the view of the claim, wMIDh will remove the claim from your RTP file sooner. This will help to limit the number of claims that are viewable in your RTP file, and will assist you in avoiding duplicate claim submission errors. Refer to the “Suppress View” information later in this chapter. As a Medicare provider, you are accountable to ensure the information you submit on your claim is correct, and according to Medicare regulations. When claims are corrected from the RTP file, a new receipt date is assigned. Therefore, it is important to remember that Medicare timely claim filing requirements apply. Correct your claims as soon as possible. The “# DAYS” field on Map 1741 tells you how long the claim has been in your RTP file. If the #DAYS field is blank, the claim just went to the RTP file during the nightly system cycle. Additional information about timely filing requirements is available on the “Timely Claim Filing Requirements” (https://www. cgsmedicare.com/Articles/COPE18411.html ) CGS Web page.
Can you delete a claim in FISS?
Occasionally, you may have claims in RTP that you do not need to correct. Although FISS does not allow you to delete a claim in RTP, we strongly recommend that you suppress the view of a claim you choose not to correct to avoid duplicate billing errors. Suppressed claims will move to the status/location I B9997 (I=inactivated), and will no longer appear on your list of claims in your RTP file. The following steps explain how to suppress the view of a claim.
Can you adjust a claim after it has been processed?
At times, you may need to adjust a claim after it has been processed to make changes (e.g., add or remove services). Claim adjustments can be made to paid or rejected claims (i.e., status/ location P B9997 or R B9997). However, adjustments cannot be made to:
Can I reverse a B9997 claim?
This action cannot be reversed. Please make sure that you want to suppress the view of the claim before following the steps below. Suppressed claims (I B9997 status/location) will still appear when viewing claims in option 12 (Claim Summary Inquiry screen).
How long does it take to see a Medicare claim?
Log into (or create) your secure Medicare account. You’ll usually be able to see a claim within 24 hours after Medicare processes it. A notice you get after the doctor, other health care provider, or supplier files a claim for Part A or Part B services in Original Medicare.
What is Medicare Part A?
Check the status of a claim. To check the status of. Medicare Part A (Hospital Insurance) Part A covers inpatient hospital stays, care in a skilled nursing facility, hospice care, and some home health care. or.
What is MSN in Medicare?
The MSN is a notice that people with Original Medicare get in the mail every 3 months. It shows: All your Part A and Part B-covered services or supplies billed to Medicare during a 3-month period. What Medicare paid. The maximum amount you may owe the provider. Learn more about the MSN, and view a sample.
What is Medicare Advantage Plan?
Medicare Advantage Plan (Part C) A type of Medicare health plan offered by a private company that contracts with Medicare. Medicare Advantage Plans provide all of your Part A and Part B benefits, excluding hospice. Medicare Advantage Plans include: Health Maintenance Organizations. Preferred Provider Organizations.
Is Medicare paid for by Original Medicare?
Medicare services aren’t paid for by Original Medicare. Most Medicare Advantage Plans offer prescription drug coverage. or other. Medicare Health Plan. Generally, a plan offered by a private company that contracts with Medicare to provide Part A and Part B benefits to people with Medicare who enroll in the plan.
Does Medicare Advantage offer prescription drug coverage?
Medicare Advantage Plans may also offer prescription drug coverage that follows the same rules as Medicare drug plans. Check your Explanation of Benefits (EOB). Your Medicare drug plan will mail you an EOB each month you fill a prescription. This notice gives you a summary of your prescription drug claims and costs.
When to switch to original Medicare?
Switch to Original Medicare during the first year on the Medicare Advantage plan (trial period). Switch to Original Medicare during the annual Medicare Advantage open enrollment period (January 1 to March 31).
How to leave Medicare Advantage?
To protect Medicare beneficiaries, lawmakers provided escape hatches for Medicare Advantage enrollees who decide – for whatever reason – that they’d rather be covered under Original Medicare . There are essentially four different avenues available to enrollees who want to leave their Medicare Advantage plan: 1 Make changes during general open enrollment (October 15 to December 7, with changes effective January 1). 2 Switch to Original Medicare during the first year on the Medicare Advantage plan (trial period). 3 Switch to Original Medicare during the annual Medicare Advantage open enrollment period (January 1 to March 31). Note that Medicare Advantage enrollees also have the option to switch to a different Medicare Advantage plan during this time. 4 Switch to Original Medicare (or a different Medicare Advantage plan, depending on the situation) if a special enrollment period becomes available.
How to get Medicare private enrollment advice?
Your State Health Insurance Assistance Program (SHIP) can help, as can a broker who specializes in Medigap plans; you can also contact the carriers in your area that offer Medigap plans and ask them about their underwriting guidelines. You can click on a state on this map to see details about state-based regulations and requirements for Medigap plans. You can also get Medicare private enrollment advice from a licensed agent at 1-844-309-3504.
How long is the disenrollment period for Medicare?
The disenrollment period, created by the Affordable Care Act, was only a month and a half long. It allowed Medicare Advantage enrollees to switch to Original Medicare and a Part D plan, but did not allow them to switch to a different Medicare Advantage plan.
What is the first year of Medicare Advantage?
First year of Advantage coverage – One-time trial period during which it’s possible to switch from Medicare Advantage to Original Medicare, Medigap or Part D plan.
What percentage of Medicare beneficiaries are in Medicare Advantage?
Medicare Advantage (Medicare Part C) has become increasingly popular over the last decade. Thirty-four percent of all Medicare beneficiaries were in Medicare Advantage plans as of 2019, up from just 13 percent in 2005. And by late 2019, nearly 38 percent of Medicare beneficiaries had private coverage, nearly all of whom had Medicare Advantage ( Medicare Cost plans are another form of private Medicare coverage, but very few people are enrolled in those plans). But that doesn’t mean everyone is happy with Medicare Advantage, or that it’s the right option for all Medicare beneficiaries who enroll in it.
How long is the Medicare trial period?
This applies to people who enrolled in Medicare Advantage as soon as they turned 65 , and also to people who switched from Original Medicare to Medicare Advantage – but only if it’s their first time being on a Medicare Advantage plan.
Step 1: Selection
The first question asked will determine if a Self-Service Reopening or a Recoupment Request will be completed.
Step 2: Corrections
All fields that are able to be adjusted are opened to make corrections. Once the correction has been made, choose Next.
Step 3: Submission
Step 3 provides the user with updated claim lines based on the changes selected. Review the changes, select the checkbox to verify the changes are accurate and choose Confirm Changes.
Step 4: Confirmation
Step 4 provides the Confirmation Number of the request. This indicates the reopening was submitted and will be processed.
