Check Status of Medicare Application
- Logging in to your My Social Security account
- Visiting your local Social Security office
- Calling Social Security
- Visiting the Check Enrollment page on your MyMedicare.gov account
How do I check the status of my Medicare application?
You may check the status of your Medicare application over the phone by calling the Social Security Administration at 1-800-772-1213 and following the automated prompts to check the status of an application or to speak with a representative.
How do I check on the status of my claim?
There are two ways you can check on the status of your claim. 1. Log in to your account at bcbsm.com. If you don't have an account, you can learn how to register in our Help Center. 2. Once you're logged in, click on the "Claims" tab in the blue bar at the top of the page.
How do I receive a health care claim status response from Medicare?
• Providers can send a Health Care Claim Status Request (276 transaction) electronically and receive a Health Care Claim Status Response (277 transaction) back from Medicare.
How do I get my Medicare drug claims information?
Your Medicare drug plan will mail you an EOB each month you fill a prescription. This notice gives you a summary of your prescription drug claims and costs. Learn more about the EOB. Use Medicare's Blue Button by logging into your secure Medicare account to download and save your Part D claims information.

How do I check Medicare claim status?
You can check your claims early by doing either of these: Visiting MyMedicare.gov. Calling 1-800-MEDICARE (1-800-633-4227) and using the automated phone system. TTY users can call 1-877-486-2048 and ask a customer service representative for this information.
How long does it take for Medicare claims to process?
approximately 30 daysMedicare takes approximately 30 days to process each claim. Medicare pays Part A claims (inpatient hospital care, inpatient skilled nursing facility care, skilled home health care and hospice care) directly to the facility or agency that provides the care.
How do I check my Medicare Part B claims?
Log into (or create) your secure Medicare account. You'll usually be able to see a claim within 24 hours after Medicare processes it....It shows:All your Part A and Part B-covered services or supplies billed to Medicare during a 3-month period.What Medicare paid.The maximum amount you may owe the provider.
How do I see pending Medicare claims Australia?
Click Get Reports. For a claim that has a claim status of Claim sent - Awaiting processing, call Medicare on 1800 700 199 to confirm that they did not receive the claim. If they did receive claim, do not complete these steps. If Medicare definitely did not receive the claim, click Reset Bulk Bill.
How long does it take for an online Medicare claim to process?
It can take us up to 7 days to process your claim. When you've submitted your claim, you can select: Download claim summary to view a PDF of the claim you just made. Make another claim.
How are claims processed?
How Does Claims Processing Work? After your visit, either your doctor sends a bill to your insurance company for any charges you didn't pay at the visit or you submit a claim for the services you received. A claims processor will check it for completeness, accuracy and whether the service is covered under your plan.
Why is Medicare not paying on claims?
If the claim is denied because the medical service/procedure was “not medically necessary,” there were “too many or too frequent” services or treatments, or due to a local coverage determination, the beneficiary/caregiver may want to file an appeal of the denial decision. Appeal the denial of payment.
How are Medicare claims paid?
Your provider sends your claim to Medicare and your insurer. Medicare is primary payer and sends payment directly to the provider. The insurer is secondary payer and pays what they owe directly to the provider. Then the insurer sends you an Explanation of Benefits (EOB) saying what you owe, if anything.
How far back will Medicare pay a claim?
12 monthsYou should only need to file a claim in very rare cases Medicare claims must be filed no later than 12 months (or 1 full calendar year) after the date when the services were provided. If a claim isn't filed within this time limit, Medicare can't pay its share.
How do I follow up on Medicare application Australia?
You can send us a general enquiry about Medicare....To send us an email, use the following email addresses:[email protected] (Australian Immunisation Register)[email protected] (Australian Organ Donor Register)[email protected] (Health Identifiers service)More items...•
How do I get my Medicare Summary Notice Online?
Log into (or create) your Medicare account. Select "Get your Medicare Summary Notices (MSNs) electronically" under the "My messages" section at the top of your account homepage. You'll come to the "My communication preferences" page where you can select "Yes" under "Change eMSN preference," then "Submit."
How do I contact Medicare?
(800) 633-4227Centers for Medicare & Medicaid Services / Customer service
File a complaint (grievance)
Find out how to file a complaint (also called a "grievance") if you have a concern about the quality of care or other services you get from a Medicare provider. Contact your State Health Insurance Assistance Program (SHIP) for local, personalized Medicare counseling.
File a claim
Get information on how and when to file a claim for your Medicare bills (sometimes called "Medicare billing"). You should only need to file a claim in very rare cases.
Check the status of a claim
Check your claim status with your secure Medicare account, your Medicare Summary Notice (MSN), your Explanation of Benefits (EOB), Medicare's Blue Button, or contact your plan.
File an appeal
How to appeal a coverage or payment decision made by Medicare, your health plan, drug plan or Medicare Medical Savings Account (MSA) Plan.
Your right to a fast appeal
Learn how to get a fast appeal for Medicare-covered services you get that are about to stop.
Authorization to Disclose Personal Health Information
Access a form so that someone who helps you with your Medicare can get information on your behalf.
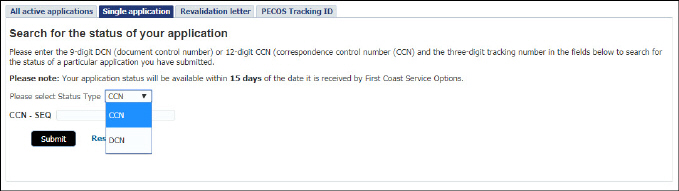
How to check Medicare application status?
To check the status of your Medicare application on the Social Security website, you will need to enter your Social Security number and the confirmation number you received when you filed your application. Your application status will show: The date your application was received. Any requests for additional documents.
How to check status of Social Security application?
Your application status will show: 1 The date your application was received 2 Any requests for additional documents 3 The address of the Social Security office processing your application 4 Whether a decision has been made about your application
How long does it take for Medicare to start?
When and how you enroll for a Medicare plan impacts when your coverage begins. Your benefits may not start until three months after you apply. If you have not received an acceptance letter 45 to 90 days after submitting your application, call the Social Security Administration or check online.
Do you get a second Medicare card?
The Medicare plans you’re enrolled in. Start dates for each plan. If you enroll in a Medicare Advantage plan , you’ll receive a second ID card for these benefits. You’ll also receive a separate card if you sign up for a standalone Part D plan.
Claim Status Inquiry
View the status of claims, Medical Review comments and initiate a redetermination on finalized claims using the Claim Status tab.
Response (Part B and DME)
The claims that match the search criteria are displayed. Select the "View Claim" link to receive additional claim information.
Response (Part A)
The claims that match the search criteria are displayed. Basic claim information is provided: ICN, Date of Service, Status, Total Charges/Billed Amount, Finalized Date, Check/EFT#, Provider Paid Amount, View Claim Details, ADR Status.
Claim Processing Comments
NMP offers access to view claim processing comments if a claim had been selected for prepayment review in which Noridian requested documentation prior to making a claim decision.
Related Claim Details
NMP allows Part B providers access to gain more information about a finalized claim that was denied or received a reduced payment due to related services.
Expanded Denial Details
NMP provides claim denial details for the below claim denials. This will allow access to important details without a separate eligibility inquiry.