As long as you have a prescription from a Medicare-enrolled physician which states that it is “medically necessary”, you will typically be covered. If the walking boots are being used to relieve pressure, especially on the sole of the foot, or are for foot ulcers, the walking boot will not be covered.
Full Answer
Does Medicare cover walking boots?
Does Medicare cover walking boots? Original Medicare Part B and Medicare Advantage plans cover ankle-foot orthosis (commonly referred to as “walking boots”) in certain cases, as long as they are rigid, or semi rigid. In what cases does Medicare Part B cover walking boots ?
Will Medicare pay for a walking aid?
We follow strict editorial standards to give you the most accurate and unbiased information. If you have trouble walking and your doctor has prescribed a walking aid, Medicare will likely pay for part of the bill. Here’s an overview of what’s covered and how best to use the coverage available to you.
What does Medicare Part B cover for walking aids?
Medicare Part B covers doctor-prescribed walking aids deemed medically necessary for use in your home. 1 Walking aids may be prescribed temporarily, such as crutches, to help recover from a broken leg. They may also be prescribed for a permanent condition, such as a wheelchair for a patient with a spinal injury or advanced Multiple Sclerosis.
Does Medicare cover replacing a walker?
So, you can replace your walker with Medicare Part B every five years, unless it has been lost, stolen or damaged beyond repair. Equipment which has been covered by Medicare which is lost, stolen or damaged beyond repair, may be replaced – Medicare will of course require proof of the initial coverage, and purchase.

How do I get Medicare reimbursement for a walker?
As with prescription medication, a walker must be prescribed to you by a doctor in order for it to qualify for coverage by Medicare. In order for a walker to be covered by Medicare, both the doctor writing the prescription and the supplier that is providing the walker must accept Medicare assignment.
Are mobility walkers covered by Medicare?
Summary: Medicare generally covers walkers as part of “durable medical equipment.” To get full coverage, you may need a Medicare Supplement plan. A walker may be essential for you if you struggle to walk without support.
Are orthopedic boots covered by Medicare?
Medicare covers orthopedic shoes if they're a necessary part of a leg brace. The amount you must pay for health care or prescriptions before Original Medicare, your Medicare Advantage Plan, your Medicare drug plan, or your other insurance begins to pay.
Are foot problems covered by Medicare?
Medicare doesn't usually cover routine foot care. You pay 100% for routine foot care, in most cases. Routine foot care includes: Cutting or removing corns and calluses.
What does Medicare cover in mobility?
Medicare Part B (Medical Insurance) covers power-operated vehicles (scooters), walkers, and wheelchairs as durable medical equipment (DME). Medicare helps cover DME if: The doctor treating your condition submits a written order stating that you have a medical need for a wheelchair or scooter for use in your home.
How often will Medicare pay for a new walker?
If your equipment is worn out, Medicare will only replace it if you have had the item in your possession for its whole lifetime. An item's lifetime depends on the type of equipment but, in the context of getting a replacement, it is never less than five years from the date that you began using the equipment.
Is a walking boot considered an orthotic?
A walking boot is an orthotic device used to protect the foot or ankle after an injury. The boot helps keep the foot stable and in the right position so that it can heal properly.
Is a walking boot considered durable medical equipment?
We offer a wide selection of durable medical equipment for orthopedic conditions, including: Crutches and walkers. Custom-fitted and prefabricated splints and walking boots. Air-pump walking boots.
Does Medicare Cover Post op boot?
There is only one HCPCS code that is appropriate for a post-op shoe (L3260, surgical shoe, each). Like orthotics, this item is a statutorily excluded benefit by Medicare and DME and will not be covered under any circumstances.
Can you claim podiatry on Medicare?
Yes it is! Your podiatry visit may be fully or partially covered by a Medicare rebate if you meet specific criteria set out by Medicare and are approved by your General Practitioner through their clinical assessment and professional discretion.
Does Medicare cover pedicures for seniors?
Medicare will cover the treatment of corns, calluses, and toenails once every 61 days in persons having certain systemic conditions. Examples of such conditions include: Diabetes with peripheral arterial disease, peripheral arterial disease, peripheral neuropathy, and chronic phlebitis.
Does Medicare cover toenail removal?
For example, Medicare will cover toenail clipping by a podiatrist if it would be hazardous to your health unless a podiatrist handled the procedure. In most cases, though, toenail clipping is not covered. Other routine foot care procedures that are not covered by Medicare include: Removal of calluses.
What is Medicare approved amount?
Medicare-Approved Amount. In Original Medicare, this is the amount a doctor or supplier that accepts assignment can be paid. It may be less than the actual amount a doctor or supplier charges. Medicare pays part of this amount and you’re responsible for the difference. , and the Part B.
What is original Medicare?
Your costs in Original Medicare. An agreement by your doctor, provider, or supplier to be paid directly by Medicare, to accept the payment amount Medicare approves for the service, and not to bill you for any more than the Medicare deductible and coinsurance.
What are therapeutic shoes?
Therapeutic shoes & inserts 1 One pair of custom-molded shoes and inserts 2 One pair of extra-depth shoes
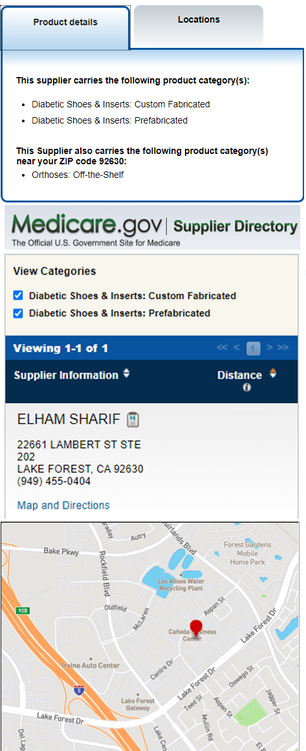
Does Medicare cover therapeutic shoes?
Medicare will only cover your therapeutic shoes if your doctors and suppliers are enrolled in Medicare. Doctors and suppliers have to meet strict standards to enroll and stay enrolled in Medicare. If your doctors or suppliers aren't enrolled, Medicare won't pay the claims submitted by them. It's also important to ask your suppliers ...
Does Medicare cover custom molded shoes?
One pair of custom-molded shoes and inserts. One pair of extra-depth shoes. Medicare also covers: 2 additional pairs of inserts each calendar year for custom-molded shoes. 3 pairs of inserts each calendar year for extra-depth shoes. Medicare will cover shoe modifications instead of inserts.
Do suppliers have to accept assignment for therapeutic shoes?
It's also important to ask your suppliers if they participate in Medicare before you get therapeutic shoes. If suppliers are participating suppliers, they must accept assignment. If suppliers are enrolled in Medicare but aren't "participating," they may choose not to accept assignment.
Overview
To determine whether Medicare will cover walking canes, you must first understand how Medicare works and what is included under its various parts.
Does Medicare Pay For Walking Canes in 2022?
Yes, Medicare will cover the purchase of a cane or walker if used as a medical necessity, such as to aid in an injury or physical ailment. A physician must have prescribed the cane for Medicare to pay for it .
What are the Medicare walking Cane Coverage Requirements?
The following are Medicare’s rules for assessing whether or not a person is qualified for a walking cane.
What Is the Procedure For Medicare To Pay For Your Walking cane?
To get Medicare to pay for a walking cane, some tasks need to be completed. You will have to go through a medical exam and prove you can safely use the cane. Additionally, you must have your physician fill out a statement on the necessity of using the cane. Here is an overview of the process:
What is the Cost That Medicare Pays For A Walking cane?
Medicare covers 80% of the cost of a walking cane, and the seniors are responsible for the remaining 20%.
How often will Medicare Pay For A cane?
Medicare will replace your walker or walking canes with Medicare Part B every five years if it is worn out. If it is lost, stolen, or broken beyond repair, Medicare may replace it, but it will certainly require verification of the original coverage and purchase.
What is Medicare assignment?
assignment. An agreement by your doctor, provider, or supplier to be paid directly by Medicare, to accept the payment amount Medicare approves for the service, and not to bill you for any more than the Medicare deductible and coinsurance. .
What is original Medicare?
Your costs in Original Medicare. In Original Medicare, this is the amount a doctor or supplier that accepts assignment can be paid. It may be less than the actual amount a doctor or supplier charges. Medicare pays part of this amount and you’re responsible for the difference.
Does Medicare cover prescriptions?
applies. Medicare will only cover these items if your doctors and suppliers are enrolled in Medicare.
Can a doctor be enrolled in Medicare?
Doctors and suppliers have to meet strict standards to enroll and stay enrolled in Medicare. If your doctors or suppliers aren't enrolled, Medicare won't pay the claims submitted by them. It's also important to ask your suppliers if they participate in Medicare before you get these items.
How much is the Medicare deductible for a 2021 walker?
You will then have to satisfy the annual Part B deductible ($203 in 2021) before your Medicare coverage of the walker will take effect. If you have already met your Part B deductible, you will typically be responsible for 20 percent of the Medicare-approved amount for the cost of the walker.
How much is Medicare Part B 2021?
In 2021, the standard Part B premium is $148.50 per month, but it can cost more for higher income earners. You will then have to satisfy the annual Part B ...
Does Medicare cover walkers?
Yes, Medicare does cover walkers and other similar durable medical equipment (DME,) which is covered under Medicare Part B. You'll need to meet certain requirements, however. Learn more about Medicare coverage for walkers and other mobility devices, as well as some of the costs you may expect to pay. Medicare will pay for any walker that is ...
Will Medicare pay for walkers in 2021?
May 27, 2021. Reviewed by John Krahnert. Medicare will pay for walkers and wheelchairs if they are considered medically necessary by your doctor. Learn more about coverage, costs and options for Medicare beneficiaries.
Do walkers have to be prescribed by a doctor?
As with prescription medication, a walker must be prescribed to you by a doctor in order for it to qualify for coverage by Medicare . In order for a walker to be covered by Medicare, both the doctor writing the prescription and the supplier that is providing the walker must accept Medicare assignment.
What is the Medicare Part B deductible for 2021?
(The Part B deductible for 2021 is $203. 3) For equipment such as motorized scooters, pre-approval may be necessary. Some Medicare Supplement Insurance plans, also known as Medigap, will cover the deductible.
What is Medicare Part B?
Medicare Part B covers doctor-prescribed walking aids deemed medically necessary for use in your home. 1 Walking aids may be prescribed temporarily, such as crutches, to help recover from a broken leg. They may also be prescribed for a permanent condition, such as a wheelchair for a patient with a spinal injury or advanced Multiple Sclerosis.
Is durable medical equipment covered by Medicare?
One final note on Medicare coverage: The durable medical equipment category is rife with Medicare fraud. 4 Always make sure to have a doctor’s prescription and use a Medicare-approved supplier (or supplier approved by your Medicare Advantage plan) to avoid scams.
Does private insurance cover walking aids?
Private insurers also offer coverage for prescribed walking aids. Depending on your plan, you may need an assessment from your healthcare provider. Whenever a mobility aid is prescribed, call your insurer before buying to check how your coverage works. You may also need to use a DME supplier that accepts your insurance.
Can you be turned down for DME?
Keep in mind, however, that you can still be turned down for coverage if you don’t have the proper prescription or assessment. As with Medicare, private insurers offer coverage under certain conditions.
Does Medicare Supplement Insurance cover deductible?
Some Medicare Supplement Insurance plans, also known as Medigap, will cover the deductible. Check with your Medigap insurer to find out if your policy offers this coverage. Once the deductible is met, any policy will pay the 20% coinsurance.
What is the Medicare Part B deductible?
In 2019, the yearly Part B deductible is $185.00.
What are the orthotics for DME?
Medicare lists the following devices as orthotics under the heading of DME: Bracing for ankle, foot, knee, back, neck, spine, hand, wrist, elbow. Orthopedic shoes as a necessary part of a leg brace. Prosthetic devices like artificial limbs. Medicare recipients must meet all the following prerequisites for eligibility:
Does Medicare cover orthotics?
Medicare Coverage for Orthotic Devices. Medicare Part B pays for 80 percent of the approved cost of either custom-made or pre-made orthotic devices. Of course, this is only possible if your health care provider feels it is medically necessary.
General Information
CPT codes, descriptions and other data only are copyright 2020 American Medical Association. All Rights Reserved. Applicable FARS/HHSARS apply.
Article Guidance
NON-MEDICAL NECESSITY COVERAGE AND PAYMENT RULES For any item to be covered by Medicare, it must 1) be eligible for a defined Medicare benefit category, 2) be reasonable and necessary for the diagnosis or treatment of illness or injury or to improve the functioning of a malformed body member, and 3) meet all other applicable Medicare statutory and regulatory requirements.
ICD-10-CM Codes that Support Medical Necessity
The presence of an ICD-10 code listed in this section is not sufficient by itself to assure coverage. Refer to the LCD section on “ Coverage Indications, Limitations, and/or Medical Necessity ” for other coverage criteria and payment information.
ICD-10-CM Codes that DO NOT Support Medical Necessity
For the specific HCPCS codes indicated above, all ICD-10 codes that are not specified in the preceding section. For all other HCPCS codes, diagnoses are not specified.
Bill Type Codes
Contractors may specify Bill Types to help providers identify those Bill Types typically used to report this service. Absence of a Bill Type does not guarantee that the article does not apply to that Bill Type.
Revenue Codes
Contractors may specify Revenue Codes to help providers identify those Revenue Codes typically used to report this service. In most instances Revenue Codes are purely advisory. Unless specified in the article, services reported under other Revenue Codes are equally subject to this coverage determination.
How to contact Medicare Plan Finder?
The licensed agents at Medicare Plan Finder are highly trained and ready to help you find a plan to suit your budget and lifestyle. Call us at 833-431-1832 or contact us here today. Contact Us | Medicare Plan Finder. This post was originally published on May 28, 2019, and updated on December 11, 2019.
What percentage of Medicare Part B is covered?
Medicare Part B may cover about 80 percent of the Medicare-approved cost, and you may have to pay the remaining co-insurance. The company that supplies your DME must be Medicare-approved. Medicare Durable Medical Equipment.
What is orthotic shoe?
Orthotic shoes are custom-fitted footwear designed to reduce the patient’s pain for a variety of health conditions including: Metatarsalgia: chronic pain in the ball of the foot. Plantar fasciitis: chronic breakdown of soft tissue around the heel. Bunions: a painful, bony bump on the outside of the big toe.
Does Medicare cover hip braces?
However, hip braces oftentimes don’t include a foot orthotic device. Medicare may help pay for the hip brace as part of your DME coverage, but coverage may not include an orthotic device.
Does Medicare cover orthotics for overweight people?
According to the Hospital for Special Surgery (HSS), orthotics can help ease the extra stress on the feet for overweight people. Medicare does not cover orthotics for people who are overweight just because they are overweight. Medicare may cover weight loss services such as surgery and/or nutrition counseling for people who qualify.
Does Medicare cover orthopedic shoes?
For the most part, Medicare does not cover orthopedic or inserts or shoes, however, Medicare will make exceptions for certain diabetic patients because of the poor circulation or neuropathy that goes with diabetes. Medicare may cover the fit and cost of one pair of custom-fitted orthopedic shoes and inserts once per year for those patients.
Can a podiatrist prescribe plantar fasciitis?
Podiatrists often prescribe treatment for plantar fasciitis. If your doctor is able to prove that it is medically necessary and the prescription is required, you may be able to get coverage at the Medicare-approved amount.
How much does an armpit crutch cost?
Sometimes this proves significantly cheaper than using an insurance plan. A pair of standard armpit crutches, for example, may cost $40 at the local pharmacy, while the insurance copayment might be $100. "A savvy consumer will look at the copay and see whether or not they need to use their insurance," Gardner says.
Can urgent care providers negotiate with Medicare?
To make matters more confusing, hospitals, urgent care centers and physicians may themselves negotiate with insurers or Medicare to become an approved supplier of medical equipment for their patients, or they may contract with a medical supply company to provide those items.
Do skinny plans have durable medical equipment coverage?
But some consumers may not get that benefit. "We're seeing more skinny plans with no durable medical equipment coverage at all," says Thomas Ryan, president and CEO of the American Association for Homecare, an advocacy organization for home care equipment manufacturers and providers.
Does insurance cover crutches?
Under the Affordable Care Act, many insurance plans are required to cover a range of essential services, such as hospitalization and prescription drugs. But reimbursement for certain medical equipment — such as crutches or a leg boot after an injury — varies widely from plan to plan.
Does the Affordable Care Act cover crutches?
Under the Affordable Care Act, many insurance plans are required to cover a range of essential services, such as hospitalization and prescription drugs. But reimbursement for certain medical equipment — such as crutches or a leg boot after an injury — varies widely from plan to plan. Under the Affordable Care Act, ...
Do insurance companies contract with medical supply companies?
These days, insurers often contract with certain medical supply companies to provide equipment, just as they negotiate rates for other services. But patients often don't realize that, says Alice Bell, a physical therapist and senior payment specialist at the American Physical Therapy Association, a professional group.
Does insurance cover medical equipment?
Under the Affordable Care Act, many insurance plans are required to cover a range of essential services, such as hospitalization and prescription drugs. But durable medical equipment isn't among them — except for breast pumps, which most plans must cover.
