There are two ways to apply for Medicaid: Contact your state Medicaid agency. You must be a resident of the state where you are applying for benefits. Fill out an application through the Health Insurance Marketplace.
Full Answer
How to apply for a Medicare supplement plan?
How to apply for a Medicare Supplement plan: The basics. Step 1: Research your plan options. There are currently 10 plans to choose from, so you have some decisions to make (for example, if you want coverage ... Step 2: See pricing and availability for your area. Step 3: Apply for the plan you want. ...
How do I enroll in Medicare?
You will not need to do anything to enroll in Medicare. Your Medicare card will be mailed to you about 3 months before your Medicare entitlement date. (Note: If you are under age 65 and have Lou Gehrig's disease (ALS), you get your Medicare benefits the first month you get disability benefits from Social Security or the Railroad Retirement Board.)
How do I apply for Medicaid?
Medicaid is a joint federal and state program that: Each state has different rules about eligibility and applying for Medicaid. Call your state Medicaid program to see if you qualify and learn how to apply. Even if you have too much income to qualify, some states let you "spend down" to become eligible for Medicaid.
Should I enroll in Medicare or Medicaid?
Persons who are enrolled in both Medicaid and Medicare may receive greater healthcare coverage and have lower out-of-pocket costs. For Medicare covered expenses, such as medical and hospitalization, Medicare is always the first payer (primary payer).
What is the highest income to qualify for Medicaid?
Federal Poverty Level thresholds to qualify for Medicaid The Federal Poverty Level is determined by the size of a family for the lower 48 states and the District of Columbia. For example, in 2022 it is $13,590 for a single adult person, $27,750 for a family of four and $46,630 for a family of eight.
What are the disadvantages of Medicaid?
Disadvantages of Medicaid They will have a decreased financial ability to opt for elective treatments, and they may not be able to pay for top brand drugs or other medical aids. Another financial concern is that medical practices cannot charge a fee when Medicaid patients miss appointments.
When the patient is covered by both Medicare and Medicaid what would be the order of reimbursement?
gov . Medicare pays first, and Medicaid pays second . If the employer has 20 or more employees, then the group health plan pays first, and Medicare pays second .
When a patient is covered through Medicare and Medicaid which coverage is primary?
Medicaid can provide secondary insurance: For services covered by Medicare and Medicaid (such as doctors' visits, hospital care, home care, and skilled nursing facility care), Medicare is the primary payer. Medicaid is the payer of last resort, meaning it always pays last.
Which state has best Medicaid program?
New YorkStates with the Best Medicaid Benefit ProgramsRankStateTotal Spending Per Person1New York$12,5912New Hampshire$11,5963Wisconsin$10,0904Minnesota$11,63346 more rows•Jun 16, 2020
How can I qualify for Medicaid?
You may be eligible if you are:65 years of age or older.An individual under 65 years of age who has a disability, or is visually impaired according to Social Security guidelines.An individual 18 years of age or younger.An adult age 19-64.A pregnant woman.A parent or caretaker.A former foster care youth.
Can you have Medicare and Medicaid at the same time?
Yes. A person can be eligible for both Medicaid and Medicare and receive benefits from both programs at the same time.
Does Medicaid pay Medicare premiums?
Medicaid pays Part A (if any) and Part B premiums. Medicaid is liable for Medicare deductibles, coinsurance, and copayments for Medicare-covered items and services. Even if Medicaid doesn't fully cover these charges, the QMB isn't liable for them.
Can you have Medicare and Medicaid?
Some Americans qualify for both Medicare and Medicaid, and when this happens, it usually means they don't have any out-of-pocket healthcare costs. Beneficiaries with Medicare and Medicaid are known as dual eligibles – and account for about 20 percent of Medicare beneficiaries (about 12.3 million people).
How do I qualify for dual Medicare and Medicaid?
Persons who are eligible for both Medicare and Medicaid are called “dual eligibles”, or sometimes, Medicare-Medicaid enrollees. To be considered dually eligible, persons must be enrolled in Medicare Part A (hospital insurance), and / or Medicare Part B (medical insurance).
When a patient has Medicaid coverage in addition to other third party payer coverage Medicaid is always considered the?
For individuals who have Medicaid in addition to one or more commercial policy, Medicaid is, again, always the secondary payer.
Does Medicare automatically forward claims to secondary insurance?
If a Medicare member has secondary insurance coverage through one of our plans (such as the Federal Employee Program, Medex, a group policy, or coverage through a vendor), Medicare generally forwards claims to us for processing.
Learn About Medicaid
What help is available through Medicaid?Medicaid provides free or low-cost medical benefits to eligible:Adults with a low incomeChildrenPregnant wo...
Learn About the Children’s Health Insurance Program (CHIP)
If your income is too high for Medicaid, your child may still qualify for the Children’s Health Insurance Program (CHIP). It covers medical and den...
File a Complaint About Medicaid or CHIP
If you have a problem with Medicaid or CHIP services, you can file a complaint. These programs are managed by each state rather than the federal go...
Who is eligible for medicaid?
Medicaid provides free or low-cost medical benefits to eligible: Adults with a low income. Children. Pregnant women. People who are age 65 or over. People with disabilities.
What age can a child get Medicaid?
It covers medical and dental care for uninsured children and teens up to age 19.
What is Medicaid and CHIP?
How to Apply for Medicaid and CHIP. Medicaid is a federal and state health insurance program for people with a low income. The Children’s Health Insurance Program (CHIP) offers health coverage to children.
How to apply for CHIP?
You have two ways to apply for CHIP: Find a program by state, or call the Health Insurance Marketplace at 1-800-318-2596 (TTY: 1-855-889-4325 ). Fill out an application through the Health Insurance Marketplace.
What is BHP in Medicaid?
Learn how to use your Medicaid or CHIP coverage. Like Medicaid and CHIP, the Basic Health Program (BHP) offers affordable, continuous coverage. It’s an optional program that your state may offer. It’s available to people with incomes that shift above and below Medicaid or CHIP levels.
How many people are covered by medicaid?
Medicaid also provides coverage to 4.8 million people with disabilities who are enrolled in Medicare.
Can you be covered by Medicare and Medicaid?
Individuals who are enrolled in both Medicaid and Medicare, by federal statute, can be covered for both optional and mandatory categories.
Can Medicare help with out of pocket medical expenses?
Medicare enrollees who have limited income and resources may get help paying for their premiums and out-of-pocket medical expenses from Medicaid (e.g. MSPs, QMBs, SLBs, and QIs).
How long does it take to apply for Medicare Supplement?
When to apply for a Medicare Supplement plan. Here's the quick answer: Most people should apply for a Medigap plan within six months of signing up for Part B. Medigap open enrollment begins when you sign up for Medicare Part B (at age 65) and lasts for six months. If you defer Part B coverage past age 65 because of health coverage ...
Is eligibility.com a Medicare provider?
Eligibility.com is a DBA of Clear Link Technologies, LLC and is not affiliated with any Medicare System Providers.
Does Medigap guarantee issue rights?
As you can see, Medigap guaranteed issue rights are incredibly valuable. Outside your open enrollment period, there are a few other scenarios where you have these rights as well. Typically these situations apply to you when you lose your existing coverage or after you try out Medicare Advantage.
Can you keep Medicare and Medigap together?
Be sure to keep your Medicare and Medigap cards together in a safe place. Your Medigap plan will be guaranteed renewable if you apply within your window of guaranteed issue rights. Guaranteed renewable means that as long as you continue to pay your premiums, you’ll keep your plan for as long as you’d like.
If you already receive benefits from Social Security
If you already get benefits from Social Security or the Railroad Retirement Board, you are automatically entitled to Medicare Part A (Hospital Insurance) and Part B (Medical Insurance) starting the first day of the month you turn age 65. You will not need to do anything to enroll.
If you are not getting Social Security benefits
If you are not getting Social Security benefits, you can apply for retirement benefits online. If you would like to file for Medicare only, you can apply by calling 1-800-772-1213.
If you are under age 65 and disabled
If you are under age 65 and disabled, and have been entitled to disability benefits under Social Security or the Railroad Retirement Board for 24 months, you will be automatically entitled to Medicare Part A and Part B beginning the 25th month of disability benefit entitlement. You will not need to do anything to enroll in Medicare.
Can you spend down your medical expenses on medicaid?
On the other hand, in medically needy states, Medicaid applicants are able to “spend down” their “excess” income on medical expenses. Once one has spent their income down to the Medicaid income limit, he / she is eligible for Medicaid for the rest of the spend down period.
Is Medicare the primary or secondary payer?
When one has original Medicare and MediGap, original Medicare is the primary payer, meaning that original Medicare pays the portion of the bills for which it owes first. The remaining portion of the bill is then sent to MediGap, who is the secondary payer.
Do you need a medicaid supplement policy?
Essentially, Medicaid takes the place of a MediGap policy. Therefore, there is no need for Medicaid beneficiaries to have a Medicare supplement insurance policy. However, in the rare case that a Medicaid beneficiary does have a MediGap policy, original Medicare is the primary payer, MediGap, the secondary payer, and Medicaid, the final payer.
Is Medicare Supplement Insurance necessary?
However, for persons who qualify for Medicaid, Medicare supplement insurance is not necessary. This is because original Medicare will continue to be the primary payer, while Medicaid will be the secondary payer. Essentially, Medicaid takes the place of a MediGap policy. Therefore, there is no need for Medicaid beneficiaries to have ...
Can you have Medigap if you have medicaid?
It is not advised that persons eligible for Medicaid maintain a MediGap health insurance policy. This is because Medicare supplement insurance helps to cover the costs that original Medicare does not, such as deductibles, coinsurance, and copayments.
Can you deposit excess income into a medicaid trust?
In income cap states (approximately half of the states), Medicaid applicants can deposit their “excess” income (the income over Medicaid’s income limit) into a Qualified Income Trust (also called a Miller Trust) in order to meet Medicaid’s income limit.
Is it illegal to sell medicaid?
That said, it is actually illegal (in most cases) for insurance companies to sell Medicaid beneficiaries a Medicare supplement insurance policy. For persons who have income over Medicaid’s income limit, there are other ways for one to meet Medicaid’s income limit.
How to apply for medicaid?
How to Apply. To apply for Medicare, contact your local Social Security Administration (SSA) office. To apply for Medicaid, contact your state’s Medicaid agency. Learn about the long-term care Medicaid application process. Prior to applying, one may wish to take a non-binding Medicaid eligibility test.
How old do you have to be to qualify for medicare?
Citizens or legal residents residing in the U.S. for a minimum of 5 years immediately preceding application for Medicare. Applicants must also be at least 65 years old. For persons who are disabled or have been diagnosed with end-stage renal disease or Lou Gehrig’s disease (amyotrophic lateral sclerosis), there is no age requirement. Eligibility for Medicare is not income based. Therefore, there are no income and asset limits.
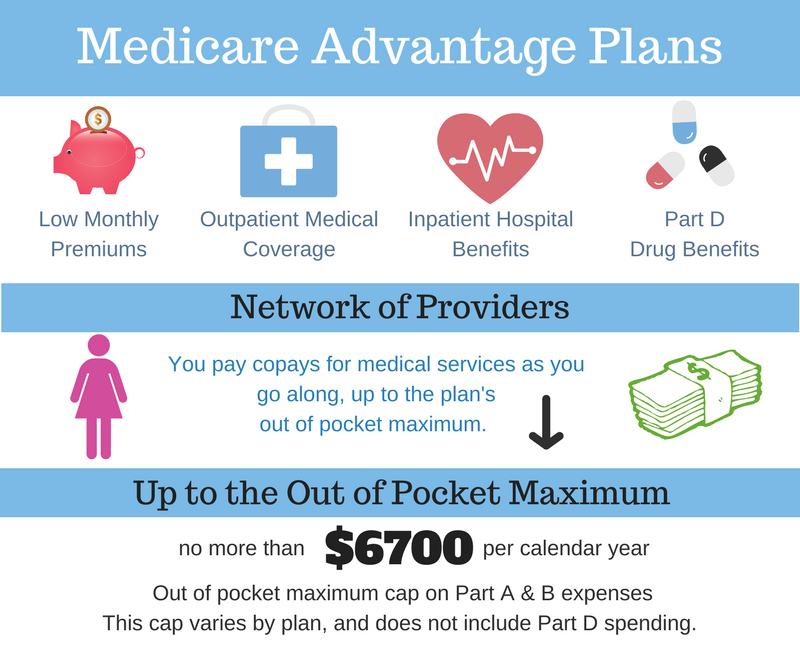
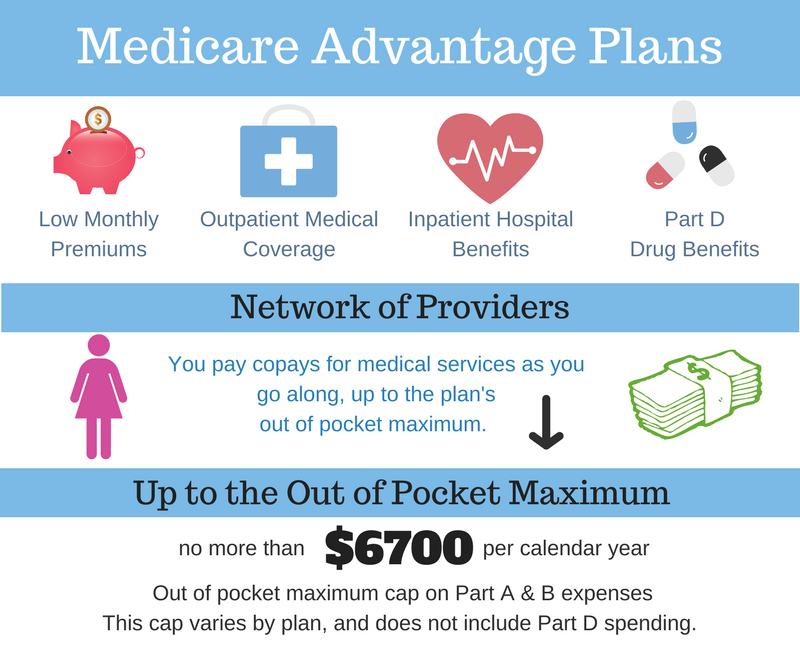
How much does Medicare Part B cost?
For Medicare Part B (medical insurance), enrollees pay a monthly premium of $148.50 in addition to an annual deductible of $203. In order to enroll in a Medicare Advantage (MA) plan, one must be enrolled in Medicare Parts A and B. The monthly premium varies by plan, but is approximately $33 / month.
What is Medicare and Medicaid?
Differentiating Medicare and Medicaid. Persons who are eligible for both Medicare and Medicaid are called “dual eligibles”, or sometimes, Medicare-Medicaid enrollees. Since it can be easy to confuse the two terms, Medicare and Medicaid, it is important to differentiate between them. While Medicare is a federal health insurance program ...
What is dual eligible?
Definition: Dual Eligible. To be considered dually eligible, persons must be enrolled in Medicare Part A, which is hospital insurance, and / or Medicare Part B, which is medical insurance. As an alternative to Original Medicare (Part A and Part B), persons may opt for Medicare Part C, which is also known as Medicare Advantage.
What is the income limit for Medicaid in 2021?
In most cases, as of 2021, the individual income limit for institutional Medicaid (nursing home Medicaid) and Home and Community Based Services (HCBS) via a Medicaid Waiver is $2,382 / month. The asset limit is generally $2,000 for a single applicant.
Does Medicare cover out-of-pocket expenses?
Persons who are enrolled in both Medicaid and Medicare may receive greater healthcare coverage and have lower out-of-pocket costs. For Medicare covered expenses, such as medical and hospitalization, Medicare is always the first payer (primary payer). If Medicare does not cover the full cost, Medicaid (the secondary payer) will cover the remaining cost, given they are Medicaid covered expenses. Medicaid does cover some expenses that Medicare does not, such as personal care assistance in the home and community and long-term skilled nursing home care (Medicare limits nursing home care to 100 days). The one exception, as mentioned above, is that some Medicare Advantage plans cover the cost of some long term care services and supports. Medicaid, via Medicare Savings Programs, also helps to cover the costs of Medicare premiums, deductibles, and co-payments.
Check when to sign up
Answer a few questions to find out when you can sign up for Part A and Part B based on your situation.
When coverage starts
The date your Part A and Part B coverage will start depends on when you sign up.
Is United American a Medicare Supplement?
United American has been a prominent Medicare Supplement insurance provider since Medicare began in 1966. Additionally, we’ve been a long-standing participant in the task forces working on Medicare Supplement insurance policy recommendations for the National Association of Insurance Commissioners.
Does Medicare Supplement Insurance cover deductibles?
The purpose of Medicare Supplement Insurance is to cover the cost left by deductibles and coinsurance in Original Medicare, but as full Medicaid coverage should cover the majority of those costs, a Medicare Supplement Insurance policy isn’t necessary. 3.
